Introduction
Abdominal wall hernias repair surgery is one of the most common surgical procedures. Inguinal hernias are undoubtedly the commonest hernia type (70% - 75%) with incidence rate 11 for each 10,000 in persons between 16 and 24 years of age, 200 for each 10,000 in persons more than 75 years of age [1]. The management of post-operative pain is oftentimes unsatisfactory. Opioids, non-steroidal anti-inflammatory drugs, and analgesics are routinely used to alleviate post-operative pain, but they are associated with several undesirable effects and do not seem to be completely effective on preventing and treating postoperative pain [2]. The estimated incidence rate of chronic pain after inguinal herniorrhaphy is about 10%. It represents a major problem that significantly affects daily activities. The severity of early postoperative pain correlates with the risk of developing chronic pain [3]. Ilioinguinal-iliohypogastric (II/IH) nerve blocks have been increasingly utilized in patients for perioperative analgesia. The use of ultrasound guidance was associated with improved perioperative analgesia compared to landmark based methods [4].
The ultrasound technology has been used for many types of peripheral nerve blocks in both adult and children. It has the advantages of increasing the success rate by easier identification of the site of the nerve, correct deposition of the local anesthetic around the nerve and decrease the incidence of complication associated with this block [5]. Bupivacaine is an amino amide highly potent local anesthetic that blocks the peripheral afferents nerve by acting on voltage dependent sodium channels so, it prevents the generation of action potential. Bupivacaine is being used for intraoperative anesthesia and postoperative analgesia [6].
In this study, the analgesic efficacy of adding II/IH nerve block to general anesthesia in inguinal hernia repair surgery was evaluated. We hypothesized that II/IH nerve block may reduce perioperative opioids requirements in such patients. The primary outcome measures were the total dose of postoperative fentanyl requirements and the postoperative pain score in the first 24 hours postoperatively. While the secondary outcomes were the hemodynamic parameters, time to first analgesic request and side effects.
Materials and Methods
This prospective, randomized, double blinded, controlled study was conducted from May 2017 to May 2018 after approval from the Institutional Research Board, Faculty of Medicine, Mansoura University given a code number (MS/17.04.46) and after obtaining an informed written consent from each patients prior to surgery. A total of 80 patients of either sex with age ranging from 20-60 years and ASA I and II scheduled for elective unilateral open inguinal hernia repair surgery were included in this study. The exclusion criteria included, patient refusal, coagulation disorders, local skin infection at site of the block, known allergy to the bupivacaine study drug, body mass index > 40 Kg m2-1 and bilateral inguinal hernia repair to be performed at the same procedure.
Patients were randomly into two groups, each group 35 patients by a computer-generated randomization table and closed envelope method. Control group: general anesthesia group and Study group (II/IH group): general anesthesia combined with ilioinguinal-iliohypogastric nerve block group. Patients in II/ IH group were injected with 20 ml of 0. 25% bupivacaine, while patients in the control group were injected with a placebo (20 ml of 0.9 saline). The anesthetist who preparing the injected drugs was not participated in the study and unaware of the patient group allocation. The surgeons, patients and ICU personnel’s who recorded the postoperative data were unaware of group allocation.
All patients were assessed preoperatively by history, physical examination, laboratory evaluation (complete blood picture, liver function, renal function tests) and ECG. The day before the surgery, the study protocol and II/IH nerve block procedure were explained to all patients. Patient was familiar with the use of 10-cm visual analogue scale score (VAS) identifying 0 as no pain and 10 as worst imaginable pain [7]. On arrival of the patient to the recovery room routine monitoring including electrocardiography, non-invasive blood pressure, and pulse oximetry was done. Peripheral intravenous cannula (20 G) was inserted, and Lactated Ringer’s started to be infused (500 mL). All patients were premedicated using midazolam 0.03 mg kg-1 IV. General anesthesia in both groups was induced using IV propofol at dose of 2-3 mg kg-1, fentanyl IV 1μ kg-1 and atracurium besylate 0.6 mg kg-1 to facilitate intubation. Patient was mechanically ventilated using a volume control mode with tidal volume 6-8 ml kg-1, respiratory rate 10-14 breath min- 1 and I: E ratio 1:2 to maintain end tidal CO2 around 35mmHg. Anesthesia was maintained using isoflurane 1, 2% and 60% air in oxygen mixture and top up dose of atracurium. Intravenous fluids were given per body weight and according to intraoperative loss. Patients in both groups received paracetamol infusion (10mg kg- 1) 15 minutes before extubation. Ketorolac amp were given to all patients every 8 hours. All patients were extubated at the end of surgery after neuromuscular reversal with administration of 0.05 mg kg-1 of neostigmine and 0.02 mg kg-1 of intravenous atropine.
The technique of II/IH nerve block was described by Wang Y, et al. [4]. Ilioinguinal-iliohypogastric nerve block was performed by ultrasound guided nerve blocks. In a supine position, the skin overlying the injection site was sterilized with complete antiseptic solution and the probe surface in contact with the skin should be covered with a sterile adhesive dressing. Place a high frequency linear probe (10 MHz or greater) medial and superior to the anterior superior iliac spine in an oblique manner at the line joining the umbilicus and the anterior superior iliac spine (ASIS). The ultrasound image revealed three muscle layers, separated by hyper echoic fascia: external oblique, the internal oblique, and the transversus abdominis muscles. The fascia transversalis is located below transversus abdominis muscle, just above the peritoneum and the abdominal cavity. Position the probe such that the bony shadow from the ASIS is visible on one side of the image on the screen. Identify the peritoneum, transversus abdominis muscle, and internal oblique muscle. The external oblique muscle may not be visible as a distinct muscle layer at this level. Sliding the probe in a cephalic direction up over the iliac crest, while maintaining the orientation of the probe along a line to the umbilicus, will bring all three muscles into view as three distinct layers. This may be useful if there is any doubt about the anatomy and the relevant planes. Always identify the deepest structures first (i.e. the peritoneum) and work toward the superficial structures to identify each layer. The ilioinguinal and Iliohypogastric nerves are seen in close proximity to one another as two small round hypo echoic structures with a hyper echoic border. They lie in the plane between the internal oblique muscle and the transversus abdominis muscle close to the ASIS. Insert the block needle in plane from medial to lateral and ensure that there is a good image of the needle tip at all times as the needle is advanced. 20 mL of 0. 25% bupivacaine was injected around the nerves in the transversus abdominis plane.
The primary outcome measures were total dose of fentanyl consumption in the first postoperative 24 hours, the time period for the first analgesic requirement and postoperative pain scores was assessed by 10 point visual analogue scale (VAS) [7]. When the patients experienced pain (VAS score >3), a bolus dose of IV fentanyl 0.5μ kg-1 was administered and can be repeated till visual analogue scale score ≤ 3 mm was attained. VAS was assessed at 30min after the end of the surgery, 2, 4, 8, 12 and 24 hours postoperatively.
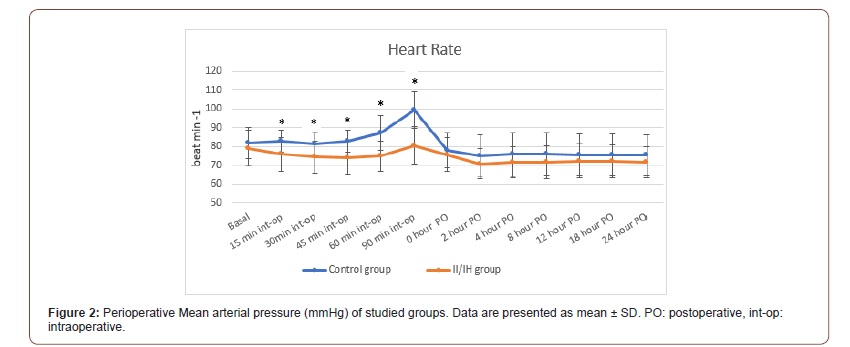
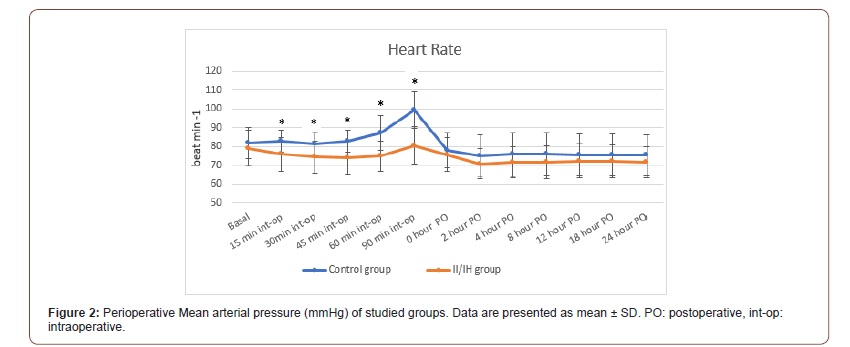
The secondary outcome measures were heart rate (HR) and mean arterial pressure (MAP). These parameters were measured before induction of anesthesia (basal value), after skin incision (approximately 15 min after the block), 30, 45, 60 and 90 minutes intraoperatively. In the post-surgical care unit, the above parameters were recorded at 0, 2, 4, 8, 12, 18, and 24 hours post-operative. Other secondary measures including postoperative complications (nausea, vomiting and itching) and duration of surgery were also recorded.
Statistical Analysis
The determination of the sample size was based on a pilot study on 10 patients (5 in each group) depending on the total dose of fentanyl consumption in the first postoperative 24 hours (123±53 versus 88±31) as a primary end point. The total required sample size was 70 patients (35 in each group) to obtain a power of 95%, and type I α error of 0.05. The total number of patients was increased to 80 to avoid 10 % dropped out cases.
The statistical analysis of data was done by using Statistical Package for Social Science (SPSS) program version 22. To test the normality of data distribution, Shapiro-Wilk test was done. Unpaired student-t test was used for comparisons between the means of two groups for quantitative data. Mann-Whitney U test was used for nonparametric data (VAS). Chi square test was used for the analysis of categorical data. The description of data done in the form of mean (±SD) for quantitative data, frequency, and proportion for categorical data and median (range) for nonparametric data. Any difference or change showing probability (P) less than 0.05 were considered statistically significant at confidence interval 95.
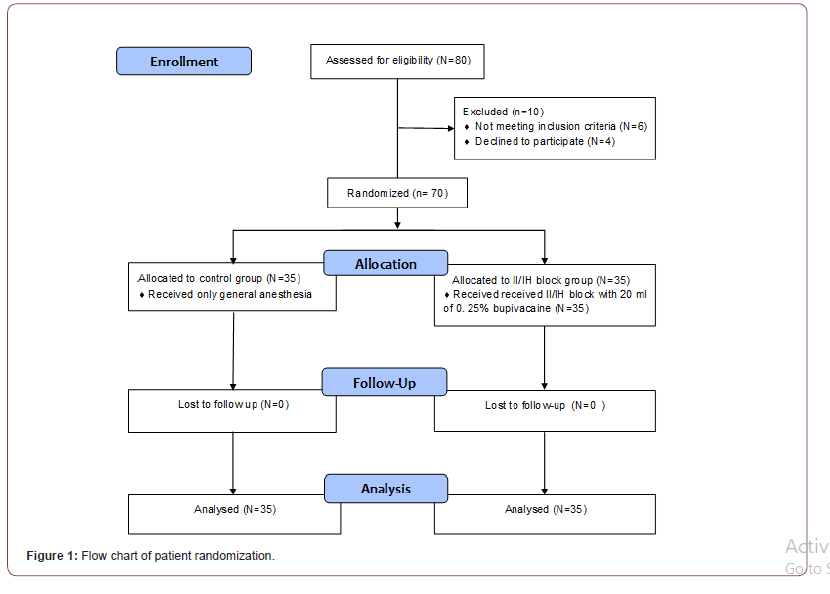
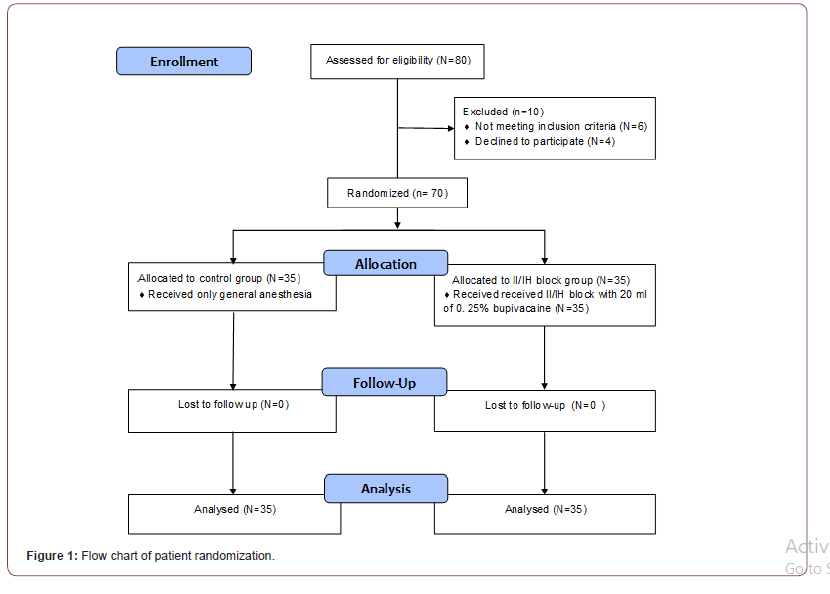
As shown in Figure 1, a total of 80 patients were included in this prospective, randomized, double blind controlled study and 10 patients were excluded or discontinued the intervention. A final of 70 patients were studied, 35 patients in the control group and 35 in the II/IH block group (Figure 1).
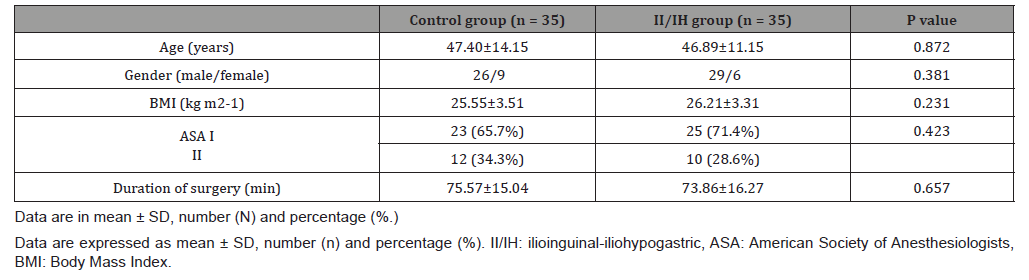
There were no statistically significant differences between the studied groups as regard: age, gender, BMI, ASA status, and duration of surgery (Table 1).
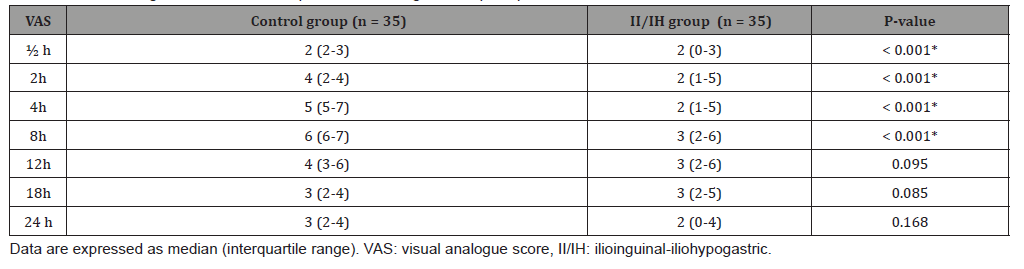
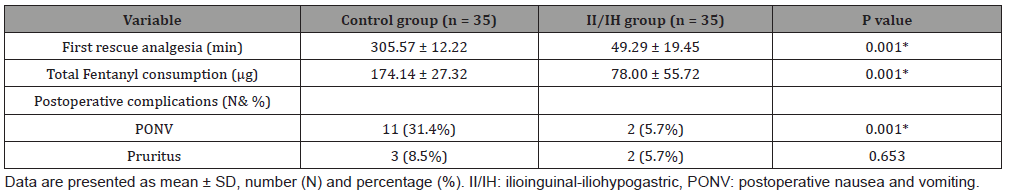
As regard the primary outcome parameters, VAS was significantly lower in the II/IH group at 0,2,4, 8 hours postoperative when compared to the control group with P value < 0.001 but no statistically significant differences were detected between the two studied groups at 12, 18 and 24 h postoperatively (Table 2). The total post-operative fentanyl consumption in the first 24h was statistically significantly lower in the II/IH group (78.00 ± 55.72 μg) than the control group (174.14 ± 27.32 μg) (Table 3). The time to the first request of analgesia showed statistically significant longer in the II/IH group (305.57 ± 12.22 min) than the control group (49.29 ± 19.45min) (Table 3).
Table 1:Demographic data of studied groups.
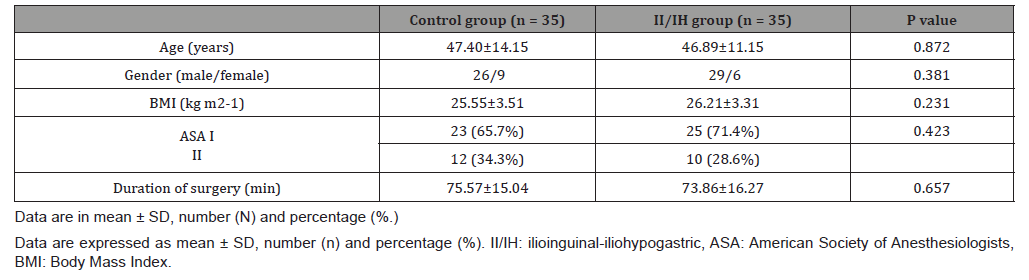
Table 2:Visual analogue score for visceral pain at rest during the first postoperative 24 hours.
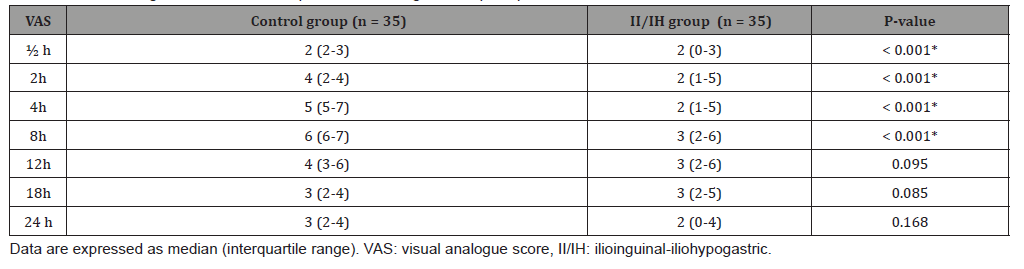
Table 3:First request of analgesia, total post-operative fentanyl (μg) consumption in the first 24 h and complications.
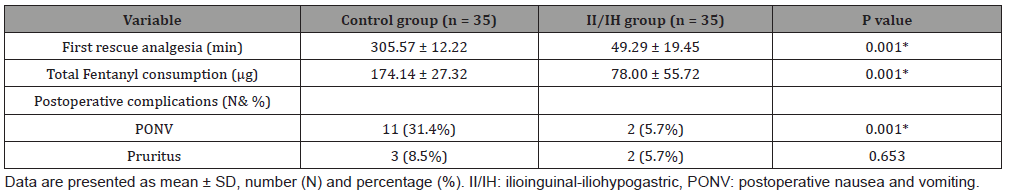
The heart rate and the mean arterial pressure showed statistically significant difference between the two studied groups intraoperatively at 15m, 30m, 45m, 1h, 1.5h. However, the heart rate and mean arterial pressure showed no statistically significant differences between the two studied groups at 0, 2h, 4h, 8h, 12h, 18h, 24h postoperative (Figure 2&3). The incidence of postoperative nausea and vomiting (PONV) was statistically significantly higher in control group than II/IH group (31.1% versus 5.7% respectively). However, there was no statistically significant difference between both studied groups as regard the Pruritus (Table 3).
Discussion
Acute postoperative pain following open inguinal hernia repair is maximum during the first 24 h period. Various modalities have been adopted to reduce this pain which includes parenteral opioids, non-steroidal anti-inflammatory drugs (NSAID), central neuroaxial analgesia and regional techniques. Among all these techniques, ultrasound guided ultrasound guided II/IH nerve block and transversus abdominis plane (TAP) block is effective and easy to perform with least complications [8].

This study was done to evaluate the efficacy of adding ultrasound guided II/IH nerve block to general anesthesia in cases of unilateral inguinal hernia repair surgery. It was found that adding the block was effective in prolonging the time of first analgesic request, decreasing the total dose of fentanyl analgesics required in the first 24 hours postoperative and providing better postoperative pain scores (VAS) and lower complications like PONV.
The present study demonstrated that the total analgesic consumption of fentanyl during 24 h postoperative was statistically significantly decreased in the study group (78.00 ± 55.72 μg) when compared to the control group (174.14 ± 27.32μg). Also, there was statistically significant prolongation of the time of first analgesic request in the study group (5.09 ± 0.2h) in comparison to the control group (0.82 ± 0.32h). This coincides with the study of Toivonen J, et al. [9] who evaluated the effect of pre-incisional ilioinguinal and iliohypogastric nerve block using 10 ml of 0.5% plain bupivacaine on postoperative analgesic requirement in patients undergoing herniorrhaphy under spinal anesthesia [9]. It demonstrated that the mean number and the total dose of supplementary analgesics was smaller in II/IH nerve block group (15 ± 25 μg) than the other group (50 ± 59 μg). Also, the average time latency was higher in block group 8.1 (0.9-54.7) h than the other group 4.3 (0.4-20.6) h. Also, our results are parallel with the study of Al Dehayat and Al Momany [10] who examined if there was difference in morphine requirements and pain scores in patients undergoing caesarean section, with and without ilioinguinal - iliohypogastric nerve block. They concluded that the quantity of morphine administered in 24 hours was 10mg (range 10-45mg) in bilateral IL and IH nerve block group and 30mg (range 0-25mg) in no block group [10].
However, these findings were in contrast with a previous study by Ding and White, 2010 who evaluated the effect of an ilioinguinalhypogastric nerve block with either saline or bupivacaine on the postoperative analgesic requirement in patients undergoing inguinal herniorrhaphy and found that a similar percentage of patients in the two groups required parenteral opioid analgesic medication in the early postoperative period and also the total dose of the fentanyl showed no statistical difference between the two groups [11]. This may be attributed to their blind technique increasing block failure rate and small sample size of only thirty patients.
In this study pain scores were statistically significantly decreased in the II/IH block group than the control group at 0, 2, 4 and 8 h. This findings are coincides with the study of Al Dehayat and Al Momany [10] who examined morphine requirements and pain scores in patients undergoing caesarean section, with and without ilioinguinal-iliohypogastric nerve block and found that Mean (SD) pain scores for block group were lesser than no block group (p<0.05) at 1, 4, 8 and 24 h [10]. The longer duration of this study may be attributed to the higher bupivacaine concentration 0.5%.
Moreover, Radhakrishnan and Kumar, 2017 who evaluated postoperative pain analgesia with ilioinguinal and iliohypogastric nerve block with 10 mL of 0.75% ropivacaine following repair of inguinal hernia surgery and time of discharge with spinal anesthesia and demonstrated that VAS at rest during different post-operative periods at 3 h, 6 h, and 12 h was assessed and found that they were significant statistically which is parallel to this current study [2].
The result of the current study revealed that heart rate and mean arterial blood pressure in II/IH block group were significantly lesser than control group intraoperatively, which may be attributed to the more effective analgesia produced by the ilioinguinal- iliohypogastric nerve block leading to more abolishing of the stress response to pain result in reducing both heart rate and blood pressure [12]. While the post-operative heart rate and mean arterial blood, pressure showed no significant statistical difference in the two groups mostly due to lower pain intensity and adding of rescue analgesia on patient demand.
The study done by Fekry DM, et al. [13] who compared Ultrasound-guided ilioinguinal- iliohypogastric, and genitofemoral nerve block with 25 mL of 0.5 % bupivacaine versus spinal subarachnoid blockade for inguinal hernia repair [13]. Both the heart rate and mean arterial blood pressure were the same without variations intra and post-operative that is parallel to our study. While the spinal anesthesia group showed decreased blood pressure at 5, 15, 30, and 45 min after spinal anesthesia.
The study done by Fekry DM, et al. [13] who compared Ultrasound-guided ilioinguinal- iliohypogastric, and genitofemoral nerve block with 25 mL of 0.5 % bupivacaine versus spinal subarachnoid blockade for inguinal hernia repair [13]. Both the heart rate and mean arterial blood pressure were the same without variations intra and post-operative that is parallel to our study. While the spinal anesthesia group showed decreased blood pressure at 5, 15, 30, and 45 min after spinal anesthesia.
Conclusion
This study proved that ultrasound guided Iliohypogastric/ ilioinguinal nerve block in open unilateral inguinal hernia repair under general anesthesia is effective in providing better quality of analgesia with prolonged time of first analgesic request, decreasing the total dose of fentanyl analgesic consumption, improving postoperative VAS values and decreasing incidence of postoperative complications as nausea and vomiting.
To know about Open Access Publishers