Authored by Jebbar Nourddine*,
Abstract
The novel corona virus disease (COVID-19) becomes a major public health. It was declared as pandemic by the World Health Organization on March 12, 2020.Myocarditis and myocardial injury are considered as one of the leading causes for death of COVID-19 Patients. The use of immunoglobulin seems to have an important role in the favorable evolution of these patients with cardiac involvement.
Background
Coronavirus disease 2019 (COVID-19) is a global pandemic. As of March 21, 2020, infected patients were present in 167 countries and region around the world and there were more than 285000 cases worldwide with nearly 12000 fatalities [1].
Besides focusing on the severe condition of pneumonia, the novel coronavirus may attack many important organs and cause multiple organ failure with cytokine storm. The heart is one of these most important organs and it is highly suspicious that viral myocarditis could be involved and even be considered as one of the leading causes of death of COVID-19 patients [2,3].
Case report
47-year old female patient, with chronic urticarial and corticosteroid in self-medication, having a stay in an endemic area (Egypt, 1 week before admission), admit to the emergency department of our hospital on 16th March 2020 for fever with asthenia and dry cough evolving for 8 days before admission. The patient benefited of a complete biological assessment objectifying a lymphopenia, moderate elevated ferritin and lactate dehydrogenase, C reactive protein at 180 mg/l and positive polymerase chain reaction (SARS COV 2).
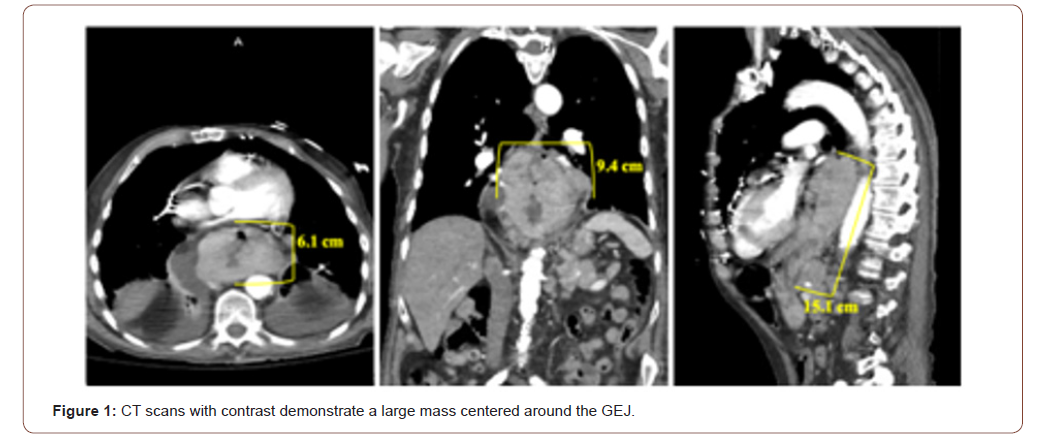
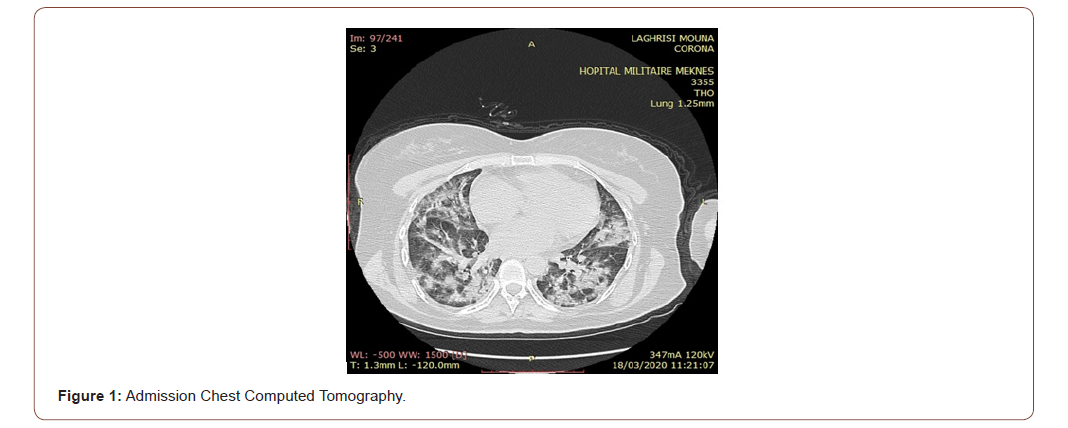
The patient was put on chloroquine, paracetamol, ceftriaxon and ciprofloxacine. 1 day before her admission in the intensive care (ICU) unit (18th March 2020), the patient presented worsening of her respiratory state made of dyspnea, 90% desaturation with a respiratory frequency at 30 cycles per minute and tachycardia at 120/min. Cardiac assessment was normal. Thoracic chest computed tomography (Figure 1) examination indicated a condensation syndrome multifocal affecting more than 60% of the pulmonary parenchyma necessitates an increased need for oxygen and her admission in the ICU. The patient was put on Lopinavir/Ritonavir, omeprazole to inhibit gastric acid and preventive anticoagulation.
The patient was intubated, 2 days after her admission in the ICU, on neurological and respiratory criteria and developed an acute respiratory distress syndrome (ARDS) and put on water restriction and diuretic (furosemide). A biological assessment objectifying a lymphopenia and C reactive protein at 188 mg/l. Blood gas analysis showed a report pao2/fio2 at 130.
8 hours after, the evolution was marked by a hemodynamic instability made of arterial tension at 70/30 mmhg and a heart rate at 130/min requiring the use of vasoactive agents (dobutamine, norepinephrine) with significant improvement under invasive monitoring.
The electrocardiogram showed sinus tachycardia. Echocardiography showed a diffuse myocardial dyskinesia, systolic dysfunction of the left ventricle, mitral annular plane systolic excursion at 7mm with left ventricular ejection fraction (LVEF) estimated to 35%, a small pericardial effusion at 5mm, inspiratory impedance threshold valve (ITV): 6-8cm, no pulmonary hypertension and dilated inferior vena cava. Troponin was at 0,06 μg/l (four times normal) and C reactive protein at 336 mg/l.
The diagnosis of this patient is coronavirus acute myocarditis with cardiogenic shock and ARDS. Treatments include methylprednisolone to suppress inflammation (200mg/day, 4 days), immunoglobulin to regulate immune status (20g/day, 4 days), dobutamine to raise blood pressure, diuretic (furosemide) to reduce cardiac load, prone position to improve the oxygenation and the zinc.
After treatment, the patient’s symptoms improved significantly after 48 hours with improvement in hemodynamic parameters and progressive withdrawal of vasoactive agents. Marker of myocardial injury (troponin) dropped after 4 days and the c reactive protein dropped to 96 mg/l after one day and to 35mg/l two days after.
Echocardiography showed that the function of the heart had returned to normal and the patient was extubated after hemodynamic stabilization and a report pao2/fio2>300. The patient benefited of non-invasive ventilation sessions for severe hypercapnia.
Otherwise, the patient presented confusion after her extubation. We performed a cerebral magnetic resonance imaging returning without abnormality. After one week, the marker of myocardial injury had fully recovered to the normal range.
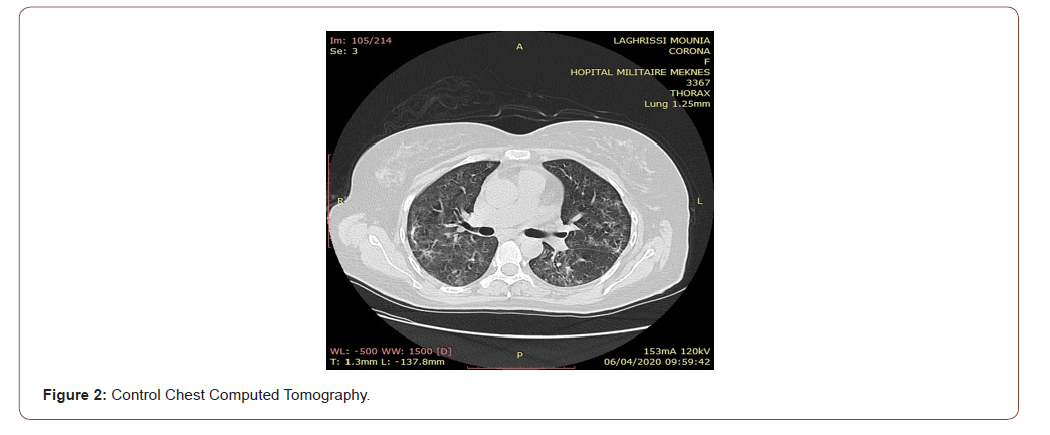
Thoracic chest computed tomography (Figure 2) objectifying an improvement in lung damage.
Then the patient was transferred to the observation ward. Negative PCR on day 27 and left the hospital with full recovery.
Discussion
American Heart Association defined myocarditis [4] by
1. Elevation in cardiac troponin I (over 0.12 ng/ml)
2. Abnormality on echocardiography: LVEF < 50% or segmental wall motion abnormality, or left ventricular wall thickening > 10mm and/or presence of pericardial effusion ≥ 5mm
3. Abnormalities on electrocardiogram (ECG): ST segment elevation/ ST-T changes
During the management of our patient, only one case of myocarditis linked to COVID-19 has been described in the literature before, indeed it is a Chinese article [5] on 37-year old male patient, admitted to hospital on 14 January 2020 with chest pain and dyspnea for three days. His blood pressure decreased to 80/50 mmhg. Chest computed tomography indicated pulmonary infection, enlarged heart and pleural effusion. The ECG suspected ST-segment elevation acute myocardial infraction. An emergency CT coronary angiography revealed no coronary stenosis. Markers of myocardial injury were elevated. Echocardiography revealed an enlarged heart and a decrease in ventricular systolic function. The diagnosis of this patient is coronavirus fulminant myocarditis with cardiogenic shock and pulmonary infection. Treatments include methylprednisolone (200 mg/day, 4days), immunoglobulin (20g/day, 4days), norepinephrine, diuretic, piperacillin sulbactam and pantoprazole. After treatment, the patient symptoms were improved. One week later, echocardiography showed that the size and function of the heart had returned to normal and markers of myocardial injury dropped significantly.
A second case [6] was published on 63-year old male, admitted to the hospital for cough with white sticky sputum, fever and shortness of breath. He had a recent history of travel to Hubei Province, China. Blood gaz analysis showed respiratory acidosis. Markers of myocardial injury were elevated. An electrocardiogram showed sinus tachycardia. Echocardiography showed an enlarged left ventricle, diffuse myocardial dyskinesia with a low LVEF (32%) and pulmonary hypertension. The diagnosis was considered severe pneumonia, ARDS fulminant myocarditis. The treatment regimen was ventilator support, high-flow oxygen, lopinavirritonavir, interferon α-1b, methylprednisolone, immunoglobulin, piperacillin-tazobactam and the ventilator was unable to maintain oxygen saturation, extracorporeal membrane oxygenation (ECMO) was used. After treatment, the LVEF gradually recovered to 68%, the left ventricle returned to its normal range.
A third published case [7] of a 21-year old female patient admitted for fever, cough, diarrhea, and shortness of breath. Markers of myocardial injury were elevated. Electrocardiogram showed nonspecific intraventricular conduction delay and multiple premature ventricular complexes. Echocardiography showed severe left ventricular systolic dysfunction. On the cardiac computed tomography, the coronary arteries were normal, and the myocardium was hypertrophied combined with a subendocardial perfusion defect on the lateral left ventricle. Cardiac magnetic resonance imaging revealed diffuse high signal intensity in the left ventricle myocardium on T2 short tau inversion recovery image and myocardial wall which suggests myocardial wall oedema. Myocarditis combined with COVID-19 was confirmed by multimodality imaging.
Conclusion
COVID-19 patients may develop cardiac complications such as myocarditis. This is the first report of COVID-19 complicated with acute myocarditis in our country. Benefit of troponin dosing and echocardiography for diagnosis. Immunoglobulin can play a very important role in the management of this situation.
To read more about this article...Open access Journal of Anaesthesia & Surgery
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers
To know about Open Access Publishers