Authored by Nayab Mustansar
Abstract
Prostate Cancer is one of the common cancers in the world. It could
primarily disseminate to the bone and can lead to death. In order to
address
its life-threatening distant metastasis, it is important to diagnose it
earlier for timely treatment. Bone metastasis is usually diagnosed
deploying
bone scan imaging. However, interpretation of the bone scans is a
tedious procedure for the physicians and often leads to
misinterpretation either
as overestimation or underestimation of the metastasis. To minimize the
risk of misinterpretation, one of the accurate methods is quantitative
analysis of the bone scans in order to ascertain, whether a metastatic
lesion is present or not. There are several methods to-date which can be
used
to analyze the extent of such lesions. The aim of this study is to use
%PAB (quantitative parameter) on a baseline bone scans. Moreover, an
improved
methodology is introduced by comparing the results with PSA levels. 141
patients with histopathologically proved prostate cancer were chosen to
implement the % PAB on individual baseline bone scans. After which, for
the calculation of risk of progression or regression of disease and
survival
rate, 40 patients were chosen from the same dataset. A serial follows up
scan was performed to calculate 2-years survival rate. The dataset was
again analyzed using the same quantitative parameter and the cut off
were calculated as % PAB: 0.5. It was found out that the % PAB method is
a
good prognostic indicator in baseline scans. Moreover, the prostate
cancer patients with the cut off % PAB > 0.5 showed increase risk of
disease
progression and less survival.
Keywords: Prostate cancer; Tumours; Cancer; PAB; Carcinoma
Keywords: Prostate cancer; Tumours; Cancer; PAB; Carcinoma
Introduction
The skeleton
The adult human skeleton has a total of 213 bones, excluding the sesamoid bones. The appendicular skeleton has 126 bones, axial skeleton 74 bones, and auditory ossicles six bones. Each bone constantly undergoes modelling during life to help it adapt to changing biomechanical forces, as well as remodeling to remove old, microdamage bone and replace it with new, mechanically stronger bone to help preserve bone strength [1]. The four general categories of bones are long bones, short bones, flat bones, and irregular bones. Long bones include the clavicles, humeri, radii, ulnae, metacarpals, femurs, tibiae, fibulae, metatarsals, and phalanges. Short bones include the carpal and tarsal bones, patellae, and sesamoid bones. Flat bones include the skull, mandible, scapulae, sternum, and ribs. Irregular bones include the vertebrae, sacrum, coccyx, and hyoid bone. Flat bones form by membranous bone formation, whereas long bones are formed by a combination of endochondral and membranous bone formation. The skeleton serves a variety of functions. The bones of the skeleton provide structural support for the rest of the body, permit movement and locomotion by providing levers for the muscles, protect vital internal organs and structures, provide maintenance of mineral homeostasis and acid-base balance, serve as a reservoir of growth factors and cytokines, and provide the environment for haematopoiesis within the marrow spaces [2]. The long bones are composed of a hollow shaft, or diaphysis; flared, cone-shaped metaphyses below the growth plates; and rounded epiphyses above the growth plates. The diaphysis is composed primarily of dense cortical bone, whereas the metaphysis and epiphysis are composed of trabecular meshwork bone surrounded by a relatively thin shell of dense cortical bone. The adult human skeleton is composed of 80% cortical bone and 20% trabecular bone overall. Different bones and skeletal sites within bones have different ratios of cortical to trabecular bone. The vertebra is composed of cortical to trabecular bone in a ratio of 25:75. This ratio is 50:50 in the femoral head and 95:5 in the radial diaphysis.Bone tumors
Bone tumors develop when cell in the bone divide without control, forming a mass of tissue. Most bone tissues are benign and they don’t spread. However, they may still weaken bone and can lead to fracture and cause other problems. Bone cancers may destroy normal bone tissues and can spread to other parts of the body called as metastasis.Benign bone tumors
They are more common than the malignant tumors. Following are the most common benign tumors.
1. Osteochondroma
2. Osteoid Osteoma
3. Giant cell Tumor
4. Osteoblastoma
5. Enchondroma
Metastatic cancer :The metastatic bone cancer is the one in which primary is present somewhere else in the body whereas it metastasizes to bone. Even though it spreads to the bone it is not considered as the bone tumor because the primary is present elsewhere. Cancers that commonly spread to the bones are:
1. Breast Cancer
2. Prostate Cancer
3. Lung Cancer
The axial skeleton, the primary site of active marrow, is the most common distribution of metastatic spread for patients with prostate cancer. At this time, there is no standard means by which osseous lesions can be directly visualized or quantified; thus, there is no qualified imaging biomarker for prostate cancer. Bone scintigraphy is commonly used to assess disease burden and treatment effects, but it is an imperfect modality for quantifying disease or for demonstrating treatment effects. Bone scans do not specifically identify cancer, can paradoxically worsen in the face of response (“flare”), and frequently improve only slowly if at all, despite patients ‘receiving active treatments [3].
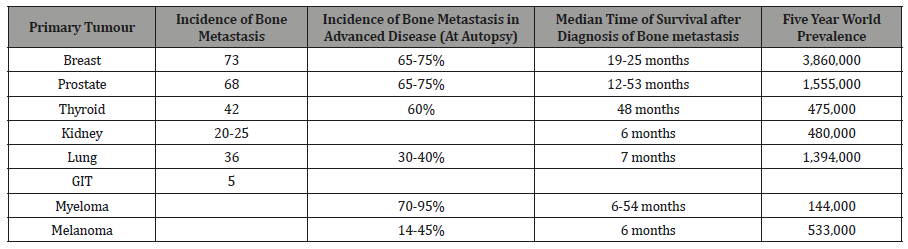
The skeleton is the most common organ to be affected by metastatic cancer and the site of disease that produces the greatest morbidity. Skeletal morbidity includes pain that requires radiotherapy, hypercalcemia, pathological fracture, and spinal cord or even nerve root compression. From randomized trials in advanced cancer, it can be seen that one of these major skeletal events occur on an average every 3-6 months. Additionally, metastatic disease may remain confined to the skeleton with the decline in quality of life and eventual death almost entirely due to skeletal complication and their treatment. The prognosis of metastatic bone disease is dependent on the primary site with the breast and prostate cancer associated with a survival measured in years compared with lung cancer, where average survival is only a matter of months. Additionally, the presence of extraosseous disease and the extent and tempo of the bone disease are powerful predictors of outcome. The latter is best estimated by measurement of bone-specific-markers, and recent studies have shown a strong correlation between the rate of bone resorption and clinical outcome, both in terms of skeletal morbidity and progression of the underlying disease [4]. Bone is the third most common site for the metastatic cancer after lung and liver cancer .It is estimated that skeletal metastasis develops in 14-70% of all the tumor patients and autopsy-based studies report the occurrence in 70% patients with carcinoma Breast and Prostate. In addition to ca prostate and ca prostate, many other tumors like lung, thyroid, kidney and melanoma have predilection for skeletal metastasis. From all the randomized trials in advanced cancer, it is estimated that one of these major skeletal events occurs on average every 3-6 months [5] (Table 1).
Table 1: Incidence of bone metastasis, Prevalence and Survival [6].
Vertebrae are most frequently involved (L>T>S>C). 38% of the metastatic disease involves the Thoraco-lumbar spine. Other bones involved in the order of the decreasing frequent are Pelvis, Ribs ,Sternum ,femur, humerus, Skull and hands. Ca Prostate specifically involves spine, femur, pelvis, skull, ribs and sternum while the one in breast carcinoma involves spine, pelvis, proximal femur, skull, ribs and mid-humerus Bone metastasis is clinically very important in prostate and breast cancer because of the prevalence of these diseases. By worldwide screening used worldwide e-g PSA levels for the prostate cancer and mammography for the breast cancer [7].
Aims and Objectives
To determine Prognostic Implication of Positive Area on Bone Scan (%PAB- Quantitative Parameter) in Bones of Patients with metastatic Prostate cancer.Materials and Methods
The study was conducted at N.O.R.I (Nuclear Medicine Oncology and Radiotherapy Institute, Islamabad) from October 2013 to April 2014. The synopsis was approved by P.I.E.A.S, Ethical Review Committee N.O.R.I hospital.Patient’s demographic data
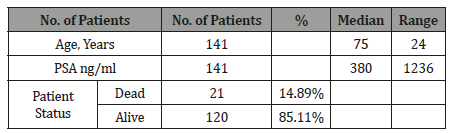
Total 141 patients with baseline bone scans were included in the study. The characteristics of the study population are depicted in the Table 2 (Table 2).Table 2: Patient’s Demographic Data (Baseline bone scan).
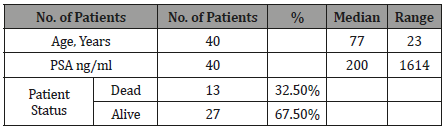
The patients with both baseline and follow up scans were 40 in total with median age of 77 and median PSA level of 200. The demographic data is given in the Table 3 (Table 3).
Table 3: Patient’s Demographic Data (Baseline and follow up scans).
1. Study design: Cross Sectional Study.
2. Place of study: Nuclear Medicine department of NORI
3. Duration: Six months.
4. Sampling Method: Nonprobability purposive sampling method
5. Sample size: 141 Patients with histopathologically proved Prostate Cancer.
(Baseline and Follow up scan of 40 patients with hormonal treatment).
Sample selection
Inclusion criterion:
1. Histological confirmed prostate cancer patients referred for evaluation of osseous metastasis within three months of diagnosis.
2. Written informed consent.
Exclusion criterion:
1. < 18 years.2. Patients in which PSA levels was not available
3. Patients having other co-morbids.
Every patient included in our study underwent Bone Scintigraphy and later the quantitative parameter was applied on the bone scan. % BSI (Bone Scan Index) was applied to the scans for the evaluation of bone metastasis.
Patient preparation and procedure:Whole procedure was explained to the patients regarding bone scintigraphy and unless any contraindication patients were well hydrated and were instructed to drink two or 8 oz glasses of water between the time of injection and the time for delayed imaging. The patients were directed to micturate immediately before delayed image and were directed to drink plenty of water for at least 24 hours of radiopharmaceutical administration.
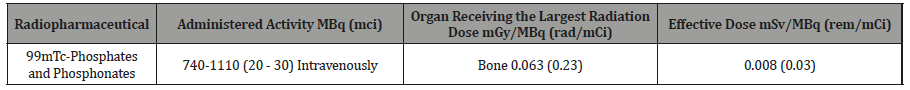
Radiation dosimetry in adults
The dose for the bone scintigraphy is given in the table 4 (Table 4).
Table 4: Radiation Dosimetry in Adults [8].
Then the following quantitative parameter was applied on the baseline bone scans.
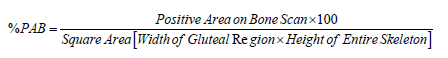
%PAB (Positive area on bone scan): Positive area on bone scan is a quantitative method in which the osseous metastasis is considered as the positive area. The same method was applied to the dataset of patients using the formula given below:





No comments:
Post a Comment