Authored by Marcelo Corti*
Introduction
The immunosuppression associated with the human immunodeficiency virus (HIV) and its consequence the Acquired immunodeficiency syndrome (AIDS), predisposes to a large series of opportunistic infections (OI) and neoplasms, such as Kaposi´s sarcoma (KS) and non-Hodgkin lymphomas [1,2]. These clinical complications are named as AIDS-defining diseases. AIDS defining illnesses include a group of pathologies whose incidence in the HIV individuals is much bigger compared with the general population. Oral cavity is a frequent engagement site in all stages of the natural history of HIV infection. The knowledge of these oral cavity clinical manifestations should suggest to the dentist the possibility of HIV infection and to investigate the serological status of the patient. For this reason, oral cavity should be carefully examined in all patients. Oral cavity manifestations of HIV infection should be classified in two groups; nonspecific clinical lesions and those directly related with the progressive immunosuppression.
Unspecific Lesions
Unspecific clinical lesions include the periodontal disease affecting the gums and dental support structures. These diseases have been classified as gingivitis, when limited to the gums, and periodontitis, when they spread to deep tissues. The linear gingival erythema (Figure 1), frequently observed in HIV/AIDS patients, is characterized by a red linear in the gingiva, near the dental arch. In patients with advanced stages of the retroviral disease ulcerative and necrotizing gingivitis can be observed. Clinical manifestations include fetid breath, gingival erosions, enamel alterations and tooth loosening [3]. HIV-infected patients can present different ulcerative lesions in the oral cavity. Recurrent aphthous stomatitis is characterized by single or multiple painful ulcerative lesions on the lateral edge of the tongue, oral mucosa and lips. These lesions can be treated with corticosteroids or thalidomide [4].
Sexually Transmitted Diseases with Oral Involvement
All the sexually transmitted diseases (STD) may have expression in the mouth; the mouth may be the site of frequent location of the syphilitic chancre (extragenital chancre) and the oral cavity can be the site of the secondary syphilis lesions. Mouth syphilitic chancre can be located anywhere into the mouth, including the tongue (Figure 2), the lips, the gums, the pharynx and the tonsils. Generally, syphilitic chancre is a single and painless lesion, but in conditions of immunodeficiency, as the HIV infection, the chancre lesions can be multiple. Symptoms of secondary syphilis include skin rash, swollen lymph nodes, fever and systemic symptoms. Secondary syphilis has multiple manifestations in the oral cavity, as the tongue papular lesions, the lichenoid lesions (opaline syphilis) (Figure 3), lingual depapilation, cracked papule at the lip commissure (Figure 4) and erosions in the oral mucosa [5].
Human Papillomavirus (HPV) is the etiologic agent of the most common sexually transmitted infection, named as genital warts or condylomata. Infection by the human papillomavirus (HPV) can also present intraoral warts (Figure 5) generally located in the oral mucosa [6]. Additionally, HPV is related with the pathogenic of 45% to 90% of oropharyngeal squamous cell carcinoma [7,8]. Generally, these malignancies appear after a long period of HIV infection; previous studies showed that HAART has not reduced the prevalence of HPV infection and has not declined the incidence of high grade anal, cervical or oral squamous epithelial lesions [9]. Gonococcal pharyngitis should be recognized and treated to avoid a reservoir of the Neisseria gonorrhoae.
Acute Primary HIV Infection
Acute primary HIV infection or acute HIV retroviral syndrome is symptomatic in more than 60% of patients. The most common clinical manifestation is a mononucleosis- like-syndrome with fever, headache, malaise, myalgia, arthralgia, a diffuse erythematous rash and a pseudomembranous or erithematous pharyngitis. Cervical symmetrical lymphadenopathy is also frequent. Mucocutaneous oral ulcerations and oral candidiasis have been reported in rare cases [10,11].
Opportunistic Infections of Oral Cavity
OI that can be seen in the oral cavity include bacterial, fungal, viral and parasitic diseases. The most frequent OI related with HIV is the oral thrush. Oral thrush is caused by an overgrowth of the fungus Candida albicans. Candidiasis is a prominent manifestation of HIV disease. This OI can be asymptomatic or produce dysphagia; is characterized by white or yellow patches of bumps on the inner cheeks, tongue, tonsils, gums, or lips (Figure 6); in some cases, oral thrush can affect the esophagus. Oral thrush is a manifestation of immunodeficiency in HIV individuals and should always make the suspicious of HIV status [12]. Same as the oral thrush, the hairy oral leukoplakia is other non-AIDS-defining disease with oral manifestation as a white lesion typically located at the edges and the tip of the tongue (Figure 7). Hairy oral leukoplakia is strongly related with the immunodeficiency of HIV infection and it can be seen in patients with less than 400 CD4 T-cell counts. Oral hairy leukoplakia is a condition related with the Epstein-Barr virus in his pathogenesis [13].
Histoplasmosis is an endemic mycosis caused by a dimorphic fungus, Histoplasma capsulatum. Histoplasmosis is a fungal disease most prevalent in patients with advance HIV/AIDS disease and CD4 +T cell counts less than 100 cells/μL. Acute and subacute disseminated forms of the disease result from reactivation of latent infection and are much more severe in patients with AIDS compared with other immunodeficiencies. The disseminated forms of the disease, affects the immunocompromised patients, especially HIV subjects with a CD4 T-cell count below 200 cell/μL, and may affect multiple organs: lungs, bone marrow, spleen, adrenal glands, liver, lymph nodes, gastrointestinal tract, central nervous system, skin and oral mucosa. In some cases, oral lesions appear to be the only primary manifestation of the disease and may compromise the tongue, palate or the oral mucosa (Figure 8, 9).
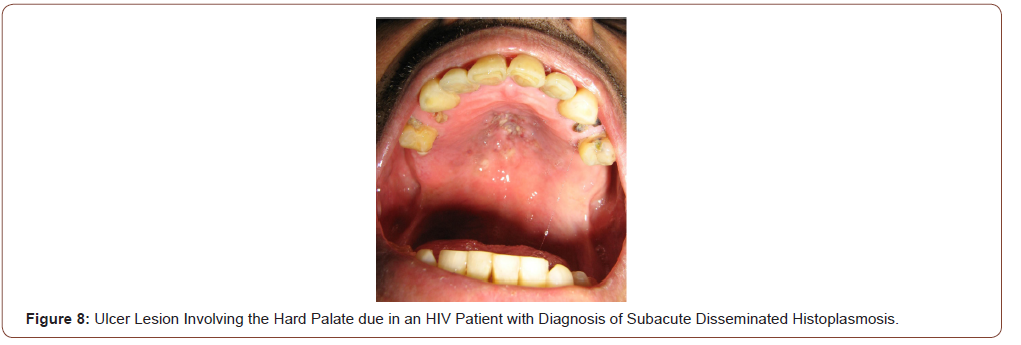
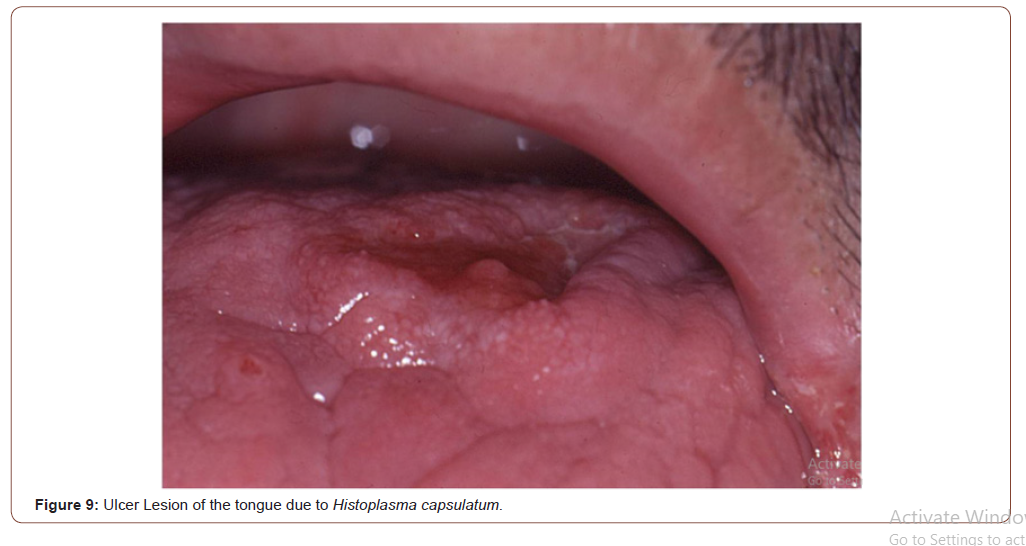
Prolonged fever, bilateral lung involvement, papules and ulcerative cutaneous lesions and frequent oral mucosal lesions are generally observed. Oral cavity lesions can involve hard palate, uvula, tongue, gingival, tonsils and pillars with painful ulcers for several weeks. Diagnosis can be rapidly confirmed by the scarification or the biopsy of these lesions. Histologic findings of histoplasmosis with hematoxylin and eosin stain typically show diffuse lymphohistiocytic infiltrates with fungal elements about 2-4 μm in size detected within the cytoplasm of histiocytes and macrophages compatible with yeats of H. capsulatum. Well-formed granulomas are generally rare in HIV patients. Special stains, such as Grocott methenamine silver and periodic acid-Schiff (PAS) methods are also useful in visualizing the fungal elements and highlight the fungal organism cell wall. The clinical differential diagnosis of oral histoplasmosis is broad and ranging from non-specific ulcers to malignancy [14].
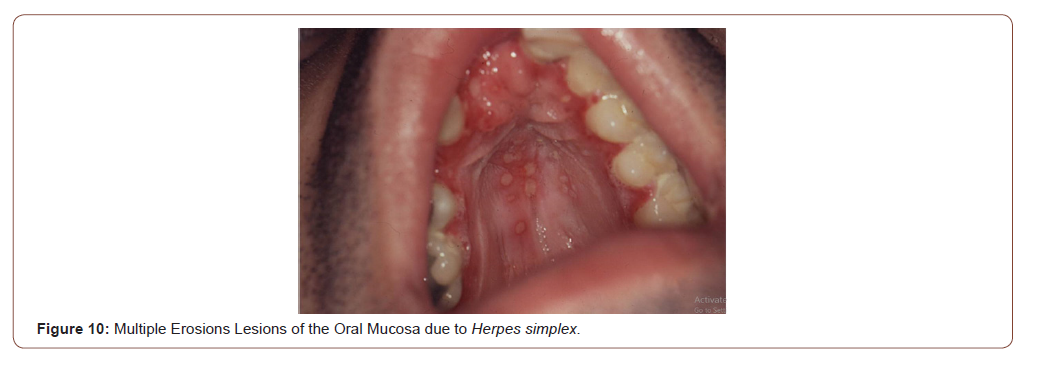
Viral infections such as Herpes simplex type I or II are to be considered in the differential diagnosis of erosive or ulcerative lesions that compromise the oral mucosa (Figure 10). Generally, the Tzanck cytodiagnosis demonstrate classic viral cytopathic effect, known as ballooning degeneration (viral syncics). Tzanck test is a quick and useful method in the diagnosis of different mucocutaneous conditions [15,16]. Bacillary angiomatosis is an unusual infectious disease, with angioproliferative lesions, typical of immunocompromised patients especially advanced HIV/AIDS disease. It is caused by Bartonella quintana and Bartonella henselae, two infectious agents of the genus Bartonella, which a variable clinical manifestations, including cutaneous vascular and nodular or tumor cutaneous violaceous lesions, regional lymphadenopathy, and even a systemic disease with visceral involvement. Purple angiomatous lesions can also locate in the oral cavity and the rhinopharynx (Figure 11). These lesions must be differentiated of the oral KS [17].
Parasitic infections, such as mucocutaneous leishmaniasis, may be rare in HIV patients, but should be investigated to exclude this unusual infection. The Tzanck cytodiagnosis can bring out amastigotes of Leishmania spp within the macrophages [14,16].
Neoplastic Diseases with Oral Involvement
KS is a malignant neoplasm, strongly associated with Human Herpes Virus 8 (HHV-8) in its pathogenesis. Lesions of KS can disseminate rapidly in severely immunocompromised HIV patients, with cutaneous, mucosal and visceral involvement. In advanced HIV/ AIDS disease, KS has a very aggressive clinical course with frequent involvement of lymph nodes, the lungs and the gastrointestinal tract in 50% of the cases. Lungs involvement occurs in 20% of the patients and is the most frequent cause of mortality. In the oral cavity, the most common sites involved by KS are the hard palate and the gums (Figure 12, 13). An intraoral examination generally revealed non-ulcerated, purple nodular lesions [18,19].
To read more about this article.....Open access Journal of Dentistry & Oral Health
Please follow the URL to access more information about this article
https://irispublishers.com/ojdoh/fulltext/oral-cavity-and-hiv-infection.ID.000556.php
To know more about our Journals...Iris Publishers





No comments:
Post a Comment