Authored by Reem Abdulrahim*,
Abstract
To display an overall review of present literature concerning coronavirus disease and dentistry as it is a matter of global concern, necessitate an alteration in dental and laboratory fields; and suggested sterilization schedules in current issue. Many recommendations have been suggested to handle many prosthodontic measures and effects of currently pandemic on prosthodontic applications, research, and learning. Comprehensive electronic search of literature related to Covid-19 and dentistry was inspected including different database articles. Various guidelines recommended by several international and national institutions and organizations such as World Health organization (WHO), and different Prosthodontics societies were included to gather the required information pertaining to possible source of spread of Covid-19 in Prosthodontics order regarding patient management and clinical strategies. The Covid-19 initiates the need to arrange a balanced program during protecting the dental professionals and treating patients at the same time. Strict application of guidelines and disinfection protocols should be evaluated with risk/advantages ratio assessment to conflict such un-matched pandemic disease.
Keywords: Covid-19; Pandemic; Dentistry; Prosthodontics; Recommendations
Introduction
Covid-19 virus is RNA-based virus that appeared in China in December 2019 as spread pneumonia- liked cases and it was informed to the World Health Organization (WHO) as uncontrolled spreading disease [1,2]. Few months later on March 2020; Covid-19 was announced as pandemic that affect all sections as a public health plague, and due to these attributions dental health workers encountered many clinical include professionals (dentists, hygienists, assistants, and technicians), financial and psychological reflections involving patients too [3,4]. Covid-19 virus primarily transmitted through person-to-person contact, and through exposure to salivation, sweat or any other body fluids making dental community nest for contagion [5,6]. Dental aerosols which considered as part of biological agent in the operating room with high-speed rotation instruments and ultrasound that could remain for several hours on the surfaces, which is a risk factor for both operator and next patients [7-9]. The scenario in dental clinic is very complex and many problems can emerge which are dangerous for the dental practice [10]. Prosthodontist which is a speciality of dentistry that produce many services to different age groups in form of partial and complete removable denture, implant supported prosthesis, crown and bridge to replace missing teeth. The prosthodontist defiance will be more because of many elements; exposure to blood during pre-prosthetic surgery and implant placement, exposure to aerosols during tooth preparation for crown and bridge, and abundent salivary concentration in dentures and measurement trays [11]. All of these mentioned factors with the majority of prosthesis patients who belongs to old age group mainly susceptible to infection easily and long multiple visiting appointments making the prosthodontist in front of distinctive challenge to guarantee dual safety at every appointment and in every step of work [11-15]. Meng, et al. [9] were the first to report on personal protection equipment (PPE) that protected dental professionals during the Covid-19 epidemic in Wuhan, China.
Sekhsaria, et al. [11] made a study to emphasize the influence of Covid-19 virus in changes of prosthodontic clinical practice. Many other scientists along the world from Poland, Germany, India, and other different countries try to find a protocol or guidelines to be followed in dental practices. This article will discuss the available measures that can be adopted by oral healthcare personnel to minimize the risk of cross-contamination in clinical practice generally and in prosthodontic clinical specially during the current COVID-19 pandemic with up-to date digital protocol recommendations.
Coronavirus Spreading
Through patient
Covid-19 virus can spread through asymptomatic, symptomatic, and even pre-symptomatic transmission. It can also spread during the recovery period, and through contact transmission [16,17]. Although this spread can range from limited to super but still should considered in general dental field [18].
Through dental practitioners
Dental physicians at higher risk when considered with other health care members because coronavirus has a high affinity to ACE2 receptors, which are highly expressed in salivary glands than respiratory mucosa, and saliva act as mainly tank for droplets transmission [16,19]. Different droplets sources during dental procedures; splash, spatter with the use of hand piece, dental syringe and ultrasonic scaler all can remain alive for few hours to days depending on the surface and may remain suspended in the air for a few hours, depending on the surrounding atmosphere [20,21].
General Considerations
Recommendations for clinic designing set-up
For the entire clinic set-up it needs to recommend separate areas with sterilization rooms and distributed according to total area available, number of health workers, and number of patients per day; all these precautions should be applied to government hospitals and private clinics (Figure 1) [2, 22]. In the reception zone where the patient submitted to give the basic information according to the clinic protocols. The patient requested to remove accessories and sensitize their hands. Non-contact temperature recording, sensor taps, contactless sanitizer dispensers are essential additions in this zone [23]. glass barrier can be fixed at the reception counter with physical distance should provide to avoid transmission of droplets between patient and the staff [2,24]. Posters can be designed and exhibit to educate patients regarding hand hygiene, respiratory rules. A pulse oximeter for monitoring changes in arterial oxygen saturation, if the oxygen saturation is less than 93%, referral to a physician [25].
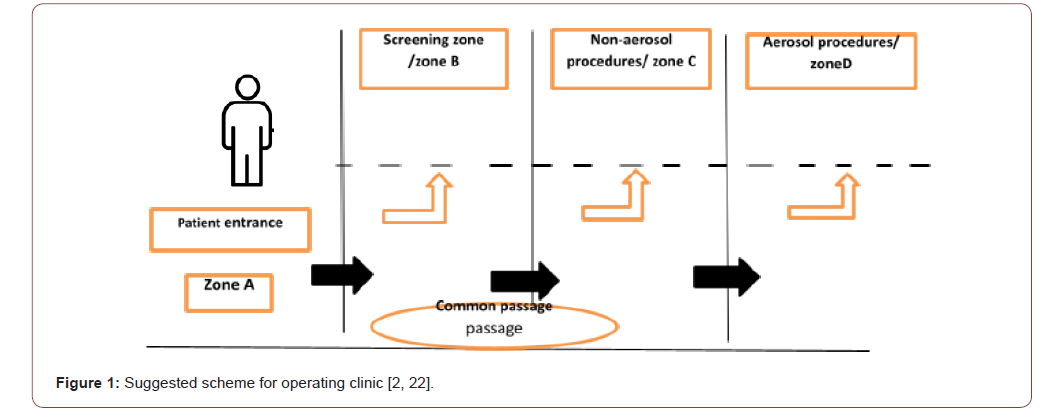
In screening zone where the diagnosis with sterile instruments is done, with the need for x-ray evaluation which is preferred to be done digitally inside the mouth rather than sending the patient to Orthopantomogram (OPG) or other x-ray types outside if it is not necessary [26]. For Zone C where the non-aerosol procedures are accomplished and instead the dentist uses the hand instruments and chemical- based caries removal agents. This area should be protected and environmentally controlled to prevent the spread of infection [27]. the suggestion for using digital workflow is preferred in this area [27, 28]. Zone D where the aerosol procedures are achieved, the use of high-speed handpieces generates aerosols shoes tendency to remain in the air for at least 30min even after the completion of the procedure and can reach up to 2 feet from the dental chair [29]. With the high risk of infection transmission in this area it become essential to adapt the universal precautions guidelines [30]:
-Only major items should be kept in open while maximum material and instruments should be kept in closed lockers.
-Obviate switching on ceiling fans during such procedures, frequent servicing of air conditioners and blocking the return air vents in centrally air-conditioned operators.
-It is generally preferred to conduct such procedures during the latter part of the day or keeping a gap of 2 h before taking up the next patient.
-Eight o’clock chair position should be avoided completely to avoid direct contact with the splatter
-Rubber dams, low-speed anti-retraction hand piece and highvolume suctions rather than chair side suctions are highly advised.
-According to Peng et al., [31] rubber dams are capable of reducing airborne particles by 70% within three feet wide operation.
Recommendations to be followed by patients
We encourage the patients attending dental clinics must carry out hand hygiene using alcohol-based hand rub or soap and water. Patients are recommended to maintain at least a 1m distance in the waiting areas and keep their belongings outside the clinic and wearing over shoes. They should be instructed not to touch their mouth, nose, and eyes with dirty hands [32,33]. Prior to the treatment, we recommend rinsing with a mouth wash to reduce the virus load in saliva prior to beginning dental treatment. Hydrogen peroxide (1-1.5%) or povidone iodine (0.2%) were reported to be most effective [34].
Personal Protective Equipment (PPE)
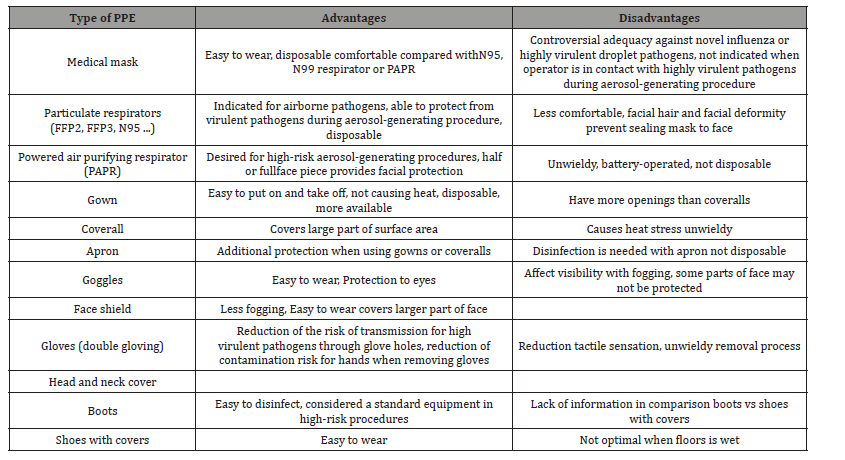
Dental group must conform several precautions to avoid infections; an adequate training and information of the personnel is obligatory in order to control infections in the dental office. The personal protection methods implicate series of fulfillment with the aim to reduce the risks of contamination, unfortunately without being able to eliminate them [35]. adequate personal protective equipment (PPE) must be selected based on a risk assessment and the procedure to be performed and according to the type of procedure and zone classification (Table 1) [36,37].
Table 1: The types of PPE commonly used for high-risk settings are shown with each advantage.
Disinfection protocols for dental clinics and laboratories
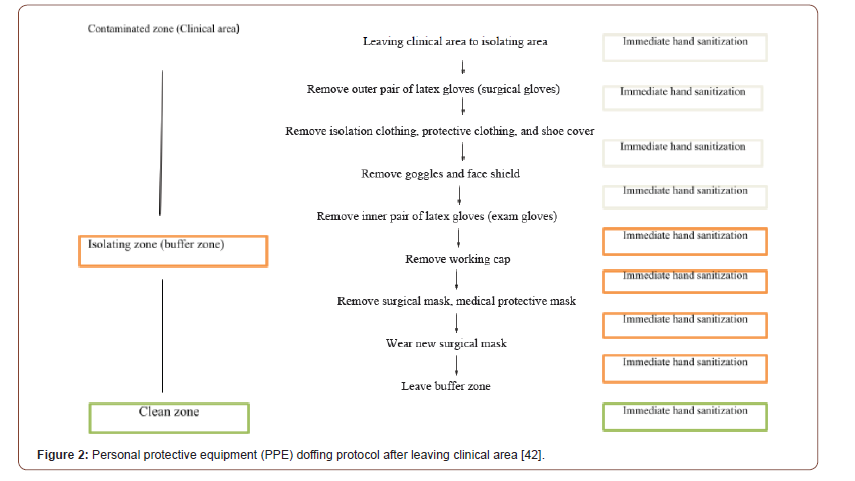
Many fundamental steps should be well applied to prevent cross sectional infection by disinfecting dental clinics and related laboratory fields to keep a pure environment and prevent transmission. Chair side assistants, support staff and laboratory technicians should be trained and enrolled on rotational basis with an aim to keep minimum workforce at a particular time. Continuous observations of staff involved in disinfection and waste disposal should be done to avoid any failure in the protocol [38]. Covid waste should be disposed in double layer bags, used PPEs should be disposed of in yellow bin, biomedical waste management (BMW) should be done in accordance with latest guidelines given in the year 2016 and amended in 2018 [39]. BMW produced during the screening, treatment, management and immunization from Covid-19 patients and healthcare staff working in the dental sections should be detailed effectively [40,41]. Another personal protective equipment (PPE) protocol should also be accomplished by health persons after finishing dental treatments and leaving the clinical area (contaminated zone) through separate rout and exist from the patient rout, which minimize the risk of infection transmission (Figure 2) [42].
Sharp objects safety: All sharps should be carefully handled in dental settings [43]:
●All sharp objects should be considered as contaminated source with the patient blood and saliva as potentially infectious.
●Cautious handling with needles to avoid accidental injections.
●All sharp objects should put suitable puncture resistant bins. Instruments sterilization:
● All instruments must be cleaned with detergent and water before sterilization [7].
● The instruments that penetrate the tissues must be sterilized in an autoclave [43].
● It is advisable to heat sterilize items that touch the mucosa or to at least disinfect them, for example, with the immersion in a 2%glutaraldehyde solution in a closed bid, naturally following the instructions of the producer [43].
●The hand pieces should be able to drain the water for two minutes at the start of the day. Not auto cleavable hand pieces can be disinfected using virucidal agent. After sterilization, all instruments must be kept safely in order to avoid recontamination for a maximum of 30 days, 60 days if closed in double bags [43].
● It is necessary to thoroughly wash and dry all items before sterilizing them as dirt and water can interfere with sterilization [43].
● Steam sterilization cannot be used for all facilities and a possible alternative can be the use of chemical sterilization using ethylene oxide gas, formaldehyde gas, hydrogen peroxide gas, liquid per acetic acid, or ozone [43, 44].
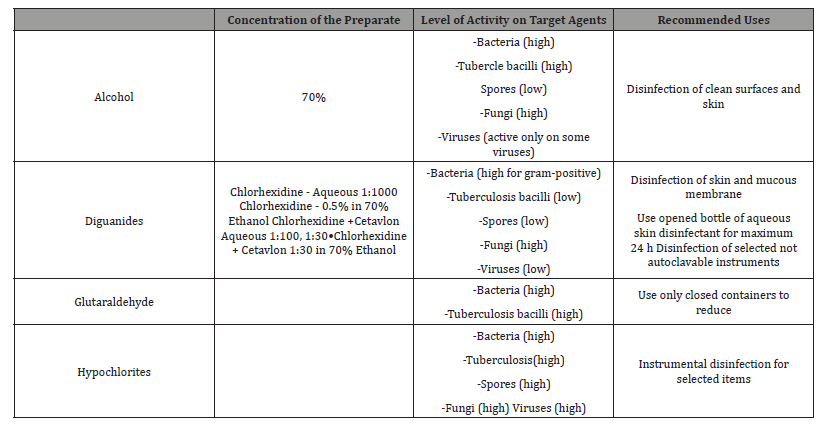
● The action of cleaning and disinfection can be manual or automatized. For example, it is possible to use ultrasonic baths in order to clean complex, articulated, or notched stainless-steel instruments such as cutters [7]. Commonly used disinfectants are described in (Table 2).
Table 2: Commonly used chemical disinfectants.
Prosthodontic Considerations During Covid-19
Based on legal and ethical frameworks, dental treatments have to be provided to all patients in demand or pain during the Covid-19 pandemic. Therefore, we recommend avoiding dental treatments unless they cannot be postponed.
According to Comis, et al. [14] questions to identify urgent treatment needs may include:
1. Do you have pain? Yes/No
2. If yes, where is the pain and from how long? Yes/No
3. Is the pain associated with swelling and limited opening of the mouth? Yes/No
4. Have you taken any medication, like paracetamol/ ibuprofen/Aspirin? If yes, did you find any relief? Yes/No
5. Do you have any underlying medical conditions? If yes, which one.
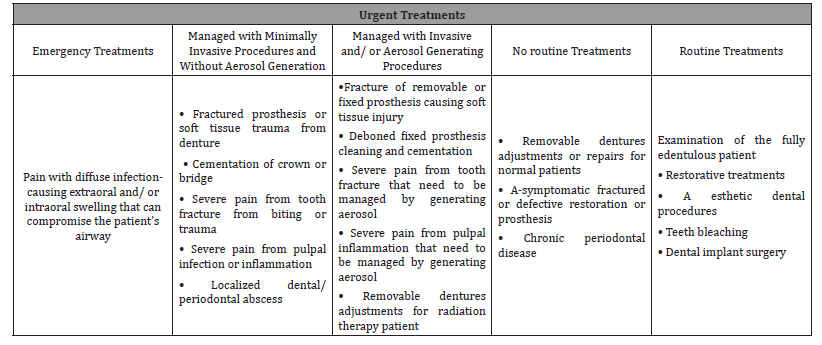
6. The prosthetic dental treatment procedures can be divided into four categories [45] as shown in (Table 3).
Table 3: Common Treatment Urgencies in Prosthodontic Clinical Practice.
Pre-prosthetic precautions
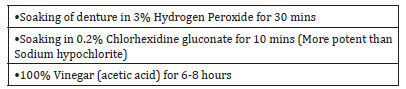
Home care guidance can be expounded over distant consultation. Patients should also be advised to disinfect the dentures at home regularly as well as before sending it to the clinic (Table 4) [11]. Any elderly patient who is a denture wearer, if infected with Covid-19 should immediately discard wearing the denture. Some fundamental testaments for patient at time of his appointment in the clinic; requesting the patients to arrive on time for their appointments, rather than too early to reduce the time spent on the dental treatment, listing appointments to minimize possible contact with other patients in the anteroom, all materials such as (magazines, newspapers, and other objects) should be removed from dental clinic to reduce the contamination [46,47].
Table 4: Methods to disinfect dentures at home.
Vaccinations
The whole dental team must be vaccinated with the newly discovery approved COVID-19 vaccine in order to increase personal protection [48,49]. According to the updating information by the American Dental Association (ADA) and the World Health Organization (WHO) [49,50].
1. Health care workers affiliated with a health care system (hospital, clinic or private practice) or pharmacy.
2. Health care workers with access to a community hospital or pharmacy can seek vaccination.
3. Health care workers without access to these facilitiesincluding those who have started the enrollment process to become a COVID-19 vaccine administration site but have not yet been approved.
Precautions and other protective measures should be followed continuously at least for a while until the 100% effectiveness of vaccine doses improved [48]. Individuals who have already been vaccinated should monitor their levels of immunity over time and make booster shots [49]. Some other researcher suggested that other types of vaccine to be taken by all dental health care professionals: hepatitis B, flu, mumps (live-virus), measles (livevirus), rubella (live-virus), and varicella-zoster (live-virus) also considered as precaution measures [51]. The influenza vaccine is very useful for dental health professionals as they are at risk for respiratory droplets infections by working in close proximity to the patients [52]. As additional infection prevention and healthcare worker measures, rapid tests can be used in dental practices to diagnose Covid-19 before each treatment. This is because, as mentioned above, a patient without symptoms is not necessarily a healthy patient.
During prosthetic workflow
For Complete Denture
●Making of snap impression followed by disinfection with glutaraldehyde.
●Alteration of final impression technique such as single step border molding.
●Virtual face bow records and jaw relation records can be used excelling the conventional technique to reduce chair side time, teeth arrangement and try-in.
●Implementing of try-in followed by denture made with Digital workflow for precise Prostheses [50].
For Fixed Prosthodontic Treatment●The Covid pandemic has changed the pattern for conventional prosthetic treatment concerning fixed prosthodontics as the procedures involve aerosols and Splatter productions that make the dentist susceptible to infection and dental chairs nest of infection.
●Use of laser for tooth preparation without the need for splatter and aerosol procedure to reduce the risk of cross contamination.
●Using high suction to reduce the splatter and aerosol production.
●Using cordless gingival retraction to further reduce the chair side time.
●Recording the digital impression followed by prostheses fabricated by CAD/CAM.
●This digital workflow reduces the chair side adjustments thus reducing the time of appointment thus delivering the prosthesis with continues service to the patients safeguarding the operator [28,51].
For Temporary or Cast Partial Denture●Digital impressions records can be made to reduce contact and chair-time of the patient.
●Virtual face-bow and bite records registrations can be made and prostheses can be fabricated.
●Prosthesis fabricated with CAD/CAM are precise and require lesser chair side adjustments [52,53]. For Implant Prosthodontics
●Guided implant placement with stents to reduce the splatter while surgical procedure.
●Immediate loading technique under proper diagnosis of the existing clinical situation to minimize the number of appointments.
●If immediate loading is contraindicated post uncovering the Osseointegrated implants digital impression can be employed and prosthesis can be fabricated with CAD/CAM and prosthesis can be delivered [54].
For Maxillofacial Prosthesis
●During pandemic time only the repair of function is considered as the dental emergency which with certain changes in the protocol of prosthesis fabrication can help the operator rehabilitate the patient thus restoring the function.
●psychological counseling and motivation for the maintenance of the prosthesis can be done through Teledentistry.
●Recording Impression with conventional or digital technology to reduce chair side time.
●Transfer of bite records on articulators for easy lab approach.
●Fabrication of prosthesis followed by insertion of prosthesis thus restoring the esthetics function and comfort of the patient [51,55].
Dental impression handling
●Dental impressions are a high-risk source of infection transmission. Autoclaved stock trays should be used and material should be loaded carefully to avoid gag reflex [56].
●Impression should be kept under running water to avert direct flow over tissue surface avoiding losing surface details [56].
●Spray disinfectant can be used for chair side disinfection followed by packing in zip lock bags before sending the impressions to laboratory for pouring [57].
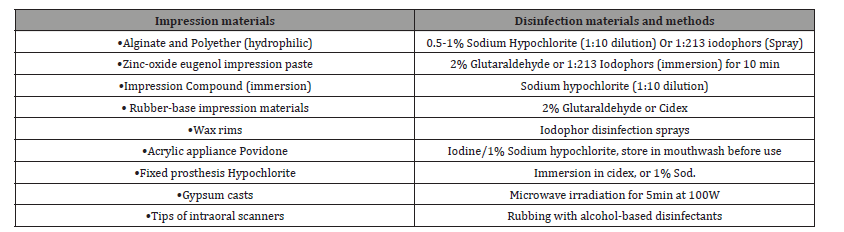
●Recommendations given in (Table 5) should be followed in the dental field for disinfection as per the material. Work authorization forms should be sent in separate zip lock bag [58].
Table 5: Disinfection of various impression and dental materials in a dental setting.
Digital prosthetic workflow
Computer-aided design/computer-aided manufacturing (CAD/ CAM) technology has become highly used among dental staff: It significantly reduces costs and working time and requires fewer steps, and the sources of error are less compared to conventional workflow [59,60]. Moreover, another important side is that the digital prosthetic workflow has many advantages in terms of infection prevention, without requiring impression disinfection [61]. During the COVID-19 pandemic the advantages of a fully digital protocol to overcome and to limit the possible infection risk for dental professionals and patient has been improved itself [62, 63].
Adopting all precautionary measures, the conventional prosthetic workflow involves several steps and procedures, which may lead to cross infection and viral contamination inside and outside the dental office, In the meantime, viruses can survive and professionals involved are extremely susceptible of cross contamination. 61 With a fully digital approach, the infection risk is just limited to the direct contact in the dental office with the patient and contamination can be prevented by the use of PPE, and surface disinfection and sterilization of the scanner tips. 64 Based on many authors opinion, whenever possible, a fully digital approach should be implemented during the Covid-19 pandemic to limit infection risk in prosthodontics (Figure 3) [28].
Future Standpoints for Optional Dental Treatment
We instruct the patients before attending the dental office to take clinical screening and it’s preferred for both dental professionals and patients to take the test rCOVID-19 before dental treatment. Unless COVID-19 test of a patient has been negative, elective treatments should be performed following the infection control measures presented in above recommendations [64].
Conclusion
Advanced prevalence of Covid-19 pandemic is associated with increased potentiality that dental workers will be exposed to Covid-19 infected patients. Therefore it has become more important for dental professionals to be included with all precautions in their daily work and further safety measures treatment of patients should be accomplished. According to the available recommendations, all patients should be considered as potentially infected by Covid-19 and prosthodontics team must use complete personal protection and follow strict procedures, obtaining safe working operations. Beside that the importance of adapting to proper guidelines can also minimize the hospitalization of Covid-19 spread through dental health care facilities. The dental team must reconsider the overall infective risk level of every dental procedure and respect the new operative protocols that are or will be formulated by respective national official committees.
To read more about this article...Open access Journal of Dentistry & Oral Health
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers





No comments:
Post a Comment