Authored by GL Khandanyan*,
Abstract
Background: In this study, the outcome of uvulopalatopharyngoplasty combined with radiofrequency of the tongue base reduction was investigated in patients with obstructive sleep apnea syndrome with both palatal and retrolingual obstruction.
Patients and methods: A retrospective cohort study was performed in patients with mild to severe OSAS. Forty-two patients with OSAS who underwent RFTBR combined with UPPP took part in this study Surgical success was defined as AHI<20 with more than 50% reduction in AHI and a response rate considered as reduction of AHI between 20 and 50%. The overall response rate was defined as more than 20% reduction in AHI.
Results: BMI was not changed significantly before (28.64±5.14kg/m2) and after surgery (28.41±5.21kg/m2). Mean AHI decreased from 49±7.23/hour to 12.63±5.72/hour (p<0.05) and mean reduction rate of AHI was 74.43±7.25% for all 42 patients, 78.9±5.14% in patients with Friedman’s anatomical stage II and 69.9±7.13% in patients with stage III (p<0.05 for both). The mean snoring sound decreased significantly from 3.35±0.67 to 1.25±1.03 at the 6th post-operative month (p<0.05). The mean value for ESS was significantly decreased from 12.6±2.17 to 5.3±1.217 at the 6th post-operative month (p<0.05).
Conclusion: Single-session RFTBR combined with uvulopalatalpharyngoplasty is an effective treatment for reducing symptoms and AHI in OSAS patients with multilevel obstruction.
Keywords: Sleep apnea; Snoring; Uvulopalatopharyngoplasty; Tongue base; Radiofrequency
Introduction
Obstructive sleep apnea syndrome (OSAS) is a very frequent and increasingly recognized major health problem [1]. OSAS may result in cardiovascular diseases, quality of life deficits and performance deficits from loss of alertness [2-5]. Nasal continuous positive airway pressure (CPAP) is considered the gold standard for the primary treatment of moderate to severe OSAS [6]. However, the therapeutic use of nasal CPAP is seriously limited by low long-term compliance [7]. The surgical approach is still the most common OSAS treatment method and varieties of surgical techniques have been well-described in managing OSAS. Uvulopalatopharyngoplasty (UPPP) and radio frequency-induced thermotherapy (RFITT) of the soft palate have been widely used for the treatment of velopharyngeal obstruction in OSAS [8,9]. Tissue volume reduction of the tongue base with RFITT was first introduced as a minimally invasive technique of sleep disordered breathing in 1999 by Powell, et al. [10]. In this study, we present our results of single-session radiofrequency of the tongue base reduction (RFTBR) combined with UPPP for the treatment of OSAS patients with multilevel obstruction.
Materials and Methods
The study was conducted collaboratively at the Department of Otorhinolaryngology of «Erebouni» medical center and Sleep Laboratory of the Institute of Cardiology between 2014 and 2017. Forty-two patients with OSAS (both with velopharyngeal and retro lingual collapses) were involved in the study (age ranging from 28 to 61 years (mean age±SEM: 47±6.27), 30 men and 12 women). None of the patients had previous velopharyngeal or lingual surgery. Patients were evaluated preoperatively and 6 months postoperatively by history taking, physical examination, fiberoptic nasopharyngoscopy and polysomnography. Retropalatal and retrolingual obstructions were determined by physical examination and observed by sleep endoscopy with midazolam. All patients with multilevel obstruction underwent one-stage RFTBR combined with UPPP. The study was approved by our institutional review board.
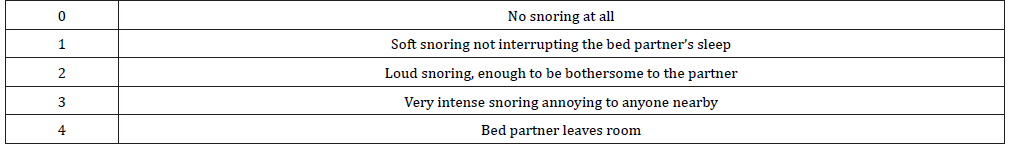
Selection criteria for the proposed treatment included significant symptoms of snoring, excessive daytime somnolence, and an apnea/hypopnea index (AHI) greater than 15. UPPP combined with RFTBR was applied only for patients with OSAS stage II or III. Patients with OSAS stage I were excluded from the examination, because they have a higher than 80% success rate when treated with UPPP only [11]. All of the preoperative examinations and the measurements including the BMI, visual analogue scoring system (VAS) for snoring (0-4) (Table 1), Epworth sleepiness scale (ESS) and polysomnography were repeated 6 months after surgical intervention. As the most important parameter for determination of OSAS, we chose the AHI during sleep. The overall response rate was defined as more than 20% reduction in AHI.
Table 1: Snoring VAS.
UPPP was carried out according to Ichiro Komada’s technique plus RFVTR of middle part of soft palate, along the uvula [12]. RFTBR was performed using the Ellman Surgitron Dual-Frequency IEC-II 4MHz (USA). Because the initial procedure was combined with UPPP, general anesthesia was required. All patients received antibiotics intravenously for 2 days postoperatively and then orally for 1 week. Oral painkillers and steroid were administered routinely. Patients were usually discharged after 2 days of surgery. After operation, the patients continued using CPAP for at least 8 to 10 days after surgery with the help of a nasal mask.
Statistical analysis
Dispersion analyses with parametric and nonparametric criteria using the GRAPH PAD PRISM5 were used in this study. Results of independent experiments were used to calculate mean values±standard errors of means (SEM), and differences were defined as statistically significant by Student’s t-test, P≤0.05. UPPP was carried out according to Ichiro Komada’s technique plus RFVTR of middle part of soft palate, along the uvula [12].
Results
Out of the 42 patients who underwent RFTBR combined with UPPP and completed the study, two had tongue base ulcerations that resolved after 1 week and one patient had complaints of slight difficulty of swallowing that lasted for one-week post-operation. Two patients complained of parageusia which resolved within 2 to 2.5 months. No postoperative complications including infections, abscesses, hematomas or airway obstruction were recorded. None of the 42 cases showed stenosis of the nasopharynx, dysphagia or Globus sensation. BMI did not change significantly before (28.64±5.14 kg/m2) and after surgery (28.41±5.21kg/ m2). Objective assessment was carried out preoperative and 6 months after operation. 30 patients were classified as stage II and 12 patients as stage III according to the Friedman staging system (Table 2).
Table 2: Outcome for 42 patients as classified by Friedman’s anatomical stage.
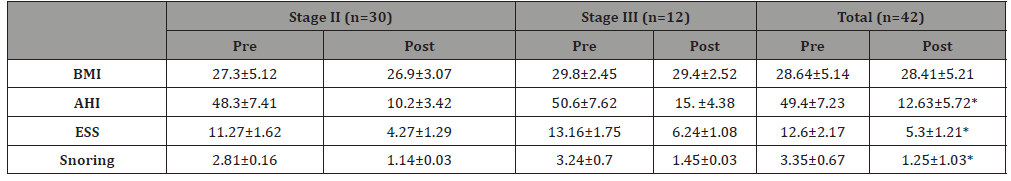
Objective success defined as a reduction of AHI by±50% and AHI<20 was obtained in 38 of the 42 patients (90%). Mean AHI decreased from 49.4±7.23/hour to 12.63±5.72/hour (p<0.05) (Table 2) and mean reduction rate of AHI was 74.43±7.25% for all 42 patients, 78.9±5.14% in patients with Friedman’s anatomical stage II and 69.9±7.13% in patients with stage III (p<0.05 for both). Significant differences were observed within each group. The mean snoring sound decreased significantly from 3.35±0.67 to 1.25±1.03 at 6th month after operation (p<0.05) (Table 2). The mean value for ESS significantly declined from 12.6± 2.17 to 5.3±1.217 after 6 months’ post-operation (p<0.05) (Table 2).
In the patients with Friedman’s anatomical stage II group the mean snoring sound decreased significantly from 2.81±0.16 to 1.14±0.03 at the 6th month (p<0.05) (Table 2). In the patients with Friedman’sanatomical stage III group the mean VAS for snoring in patients of that group was 3.24±0.7 preoperatively and 1.45±0.03 (p<0.05) in the last visit (6 months post-operation) (Table 2). Postoperative ESS values were significantly reduced after treatment for both stage II and III patients. The ESS index decreased from 11.27±1.62 to 4.27±1.29 in patients with Friedman’s anatomical stage II, and from 13.16±1.75 to 6.24±1.08 in patients with stage III (p<0.05 for both) (Table 2).
Discussion
There is great importance in evaluating the level of airway obstruction and assessing multilevel pharyngeal surgery for overcoming collapse at multiple levels of the pharyngeal airway. The study we conducted shows that combined treatment of UPPP and RFTBR for patients with both palatal and retrolingual obstruction is highly effective in eliminating symptoms that most often make the patients seek treatment. To be more exact, 88.4% of the patients included in the study had significant reduction of snoring levels whereas all the participating patients noted subjective reduction of daytime somnolence. Sher, et al. [13] reported previously that a patient population without tongue-based obstruction demonstrated a 42% UPPP success rate. The success rate was 5% in patients with tongue base obstruction [13].
Nelson combined two subsequent RFTBR with UPPP in patients with multilevel obstructison for which he obtained an improved response rate (50% success rate) [14]. According to our results, objective success, as evaluated by a reduction in AHI of±50% and AHI<20, was obtained in 38 of the 42 patients (90%). Friedman, et al. [15] reported that UPPP exhibited a success rate of 37.9% in Friedman stage II patients and 8.1% success rate in stage III patients. In stages II and III patients treated with UPPP and RFTBR, success rates were 74.0 and 43.8%, respectively [15]. Among these patients, 59.3% were operated on with a one-time tongue base radiofrequency reduction, while the others received a maximum of six procedures. In our study, the success rate was 81% and 70% in stage II and III patients, respectively.
Most frequent complications after UPPP in OSAS patients are velopharyngeal insufficiency, dysphagia, persistent dryness, Globus sensation and nasopharyngeal stenosis. All these side effects are reportedly seen from 10% to 58% of OSAS patients postoperatively [16-19]. The most important concept in our method of surgery is to preserve the uvula and leave the middle soft palate intact. In this study, no one of patient displayed nasopharyngeal stenosis, velopharyngeal insufficiency, dysphagia, persistent dryness and globus sensation in 6 months follow-up period after surgery. The lateral pharyngoplasty described by Cahali preserves the middle soft palate, and it established a 53% success rate in 15 patients. Mean AHI decreased from 41.6 to 15.5 after surgery [20]. Because of the implementation of UPPP combined with RFTBR techniques in our study, we achieved a high post-operative success rate (90%).
Conclusion
Single-session RFTB combined with uvulopalatopharyngoplasty is an effective treatment method for symptom and AHI reduction in OSAS patients with multilevel obstruction. It is also considered safe because of the minimal postoperative morbidity and complication rate. The presented a method of the UPPP for the surgical treatment of OSAS patients, is a new concept for the creation of separate right and left scars, leaving the middle soft palate intact. The intact middle soft palate and separated scars create a widened pharyngeal space while preserving the pharyngeal functions.
To read more about this article....Open access Journal of Otolaryngology and Rhinology
Please follow the URL to access more information about this article
https://irispublishers.com/ojor/fulltext/one-stage-multilevel-surgery-for-the-treatment-of-obstructive-sleep-apnea-syndrome.ID.000581.phpTo know more about our Journals...Iris Publishers





No comments:
Post a Comment