Authored by M Beghdad*,
Abstract
Neoplasms of the parapharyngeal space are extremely rare and represent 0.5% of all tumors of the head and neck. The majority of the mare benign and originate in the salivary gland region. Pleomorphic adenoma is the most common salivary glandular benign tumor. We report the case of a 44-year-old woman presented with the complaint of a dysphagia and swelling of the left soft palate. Cervical computed tomography showing very limited mass in the left parapharyngeal space. The patient was operated on and total excision of the lesion was carried out using a trans-oral approach. Histological examination revealed a pleomorphic adenoma. No post-surgical complications were noted. No recurrence was noted during the 2 years of follow-up.
Keywords: Pleomorphic adenoma; Para-pharyngeal space
Introduction
Para-pharyngeal space neoplasms are rare, although they can be account for 0.5% of all tumors in the head and neck [1,2]. 70 to 80% are benign tumors with 40 to 50% originating in the salivary glands. The pleomorphic adenoma is the most frequent histological type [3,4]. Pleomorphic adenomas of the salivary glands can develop at any age, most frequently within 4 to 6 decades. It can grow at the expense of the accessory salivary glands or the deep lobe of the parotid gland. The Clinical Symptomatology is poor, correlated the mass effect of the tumor on the structures adjacent [5,6].
Case Report
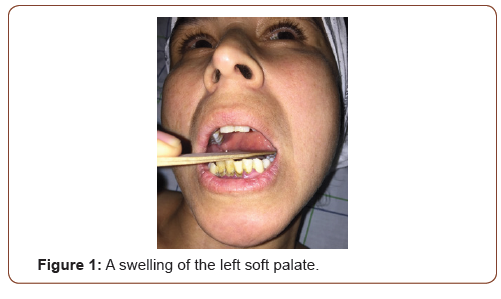
A 44-year-old female was referred to our ENT department complaining with a dysphagia evolving since 9 mounth, associated with snoring night and a rhinolalia without dyspnea or dysphonia. She had no fever and denied having a throatache. The intra-oral examination of the patient was conducted by a firm of swelling of the left soft palate and the left lateral pharyngeal walla cross the midline and pushing the uvula to the right side (Figure1).
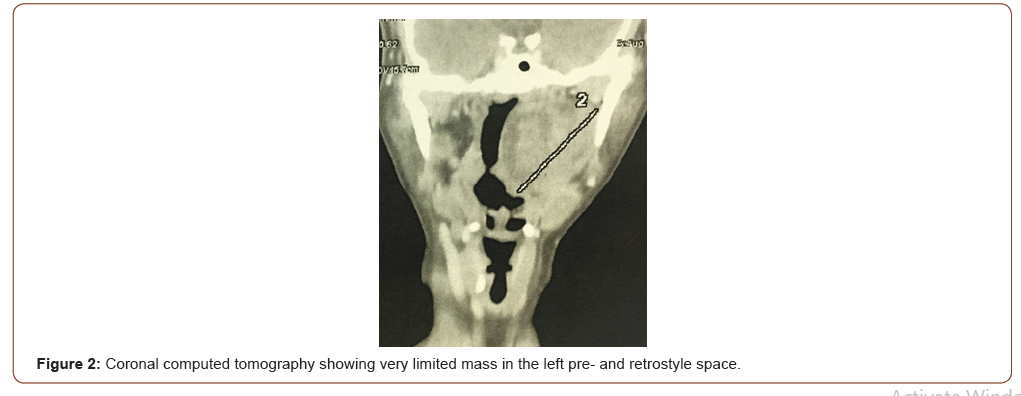
Clinical examination did not detect any cranial nerve involvement. And there was any palpable cervical lymphadenopathy. Cervical CT scan showed a very limited tissue mass of 5cm long axis, in the left pre- and retrostyle space, separated from the deep lobe of the parotid gland by a fatty border. This mass is enhanced heterogeneously after injection of contrast. There was no bone lysis (Figure2).
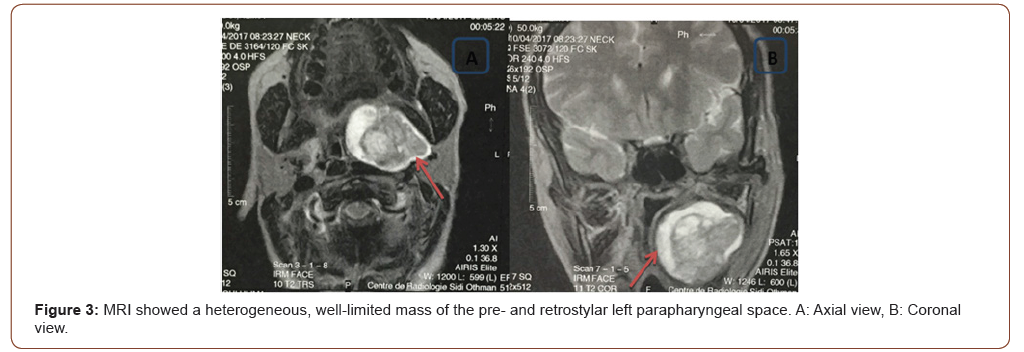
MRI showed a heterogeneous, well-limited tissue mass of the pre- and retrostylar left parapharyngeal space, iso-signal T1 and hyper-signal T2 measuring 51*34*44mm with a heightening intense after injection of Gadolinium. this mass is in hyper signal diffusion with ADC at 2.03. it is in intimate contact with the deep lobe of the parotid gland with a border of separation. It comes forward in contact with the base of the tongue without any sign of invasion. It pushes the left paraphaygeal wall inwards (Figure 3).
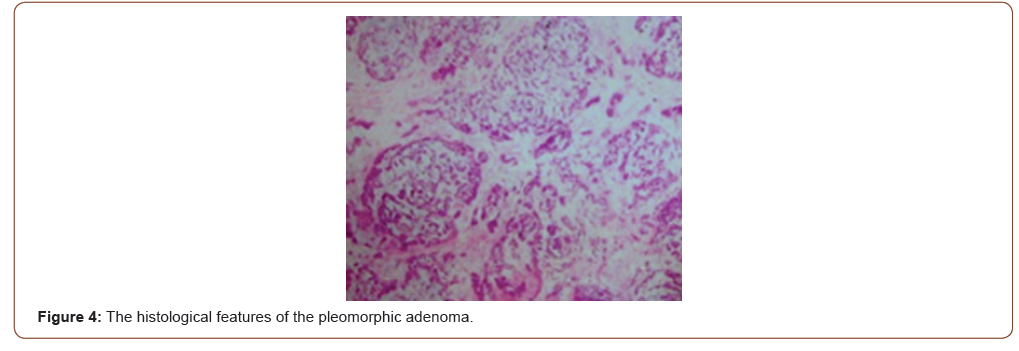
The diagnosis of a benign tumor was made. Surgery has been indicated. The patient was operated on by trans-oral, after a vertical incision in front of the anterior pillar extending from the right hemipalate to the pelvilingual sulcus. After exposure of the mass, the delivery of the tumor was easy, and the excision was complete. The postoperative follow-up was simple. The final anatomopathological examination concluded that a pleomorphic adenoma was found (Figure 4).
Discussion
Tumors of the para-pharyngeal space are characterized by a large histological diversity due to a great histological diversity explained by the different structures within this space [7]. Tumors of the retrostyllial space are dominated by Nerve tumors (schwannomas, neurofibromas), while the prestylian space is dominated by tumors of the salivary glands. The pleomorphic adenoma is the most common histological type [5,7]. Clinical expression is tardive due to its deep localization. The delay of consultation is 9 months on average in the literature [8], Tumors of the parapharyngeal space are found most often in front of an intraoral mass, or cervical. The other signs found are correlated with the effect of mass caused by the tumor on adjacent structures such as dysphagia, pharyngeal discomfort, rhinolalia, and snoring. Sleep apnea syndrome has been also described. The physical examination is poor. Usually a non-beating intra-oral mass covered of a smooth mucous membrane pushing back the tonsil by inside [3,9,10].
Parapharyngeal space tumors often pose a diagnostic problem. Imaging was essential for topographical diagnosis and for guide the etiological investigation. Computed tomography is the first-line exam. It allows the study of the the relationship of the tumor to the base of the skull, to study the vascularization and to determine its pre or retrostylial origin. The sensitivity of the MRI in the topographic diagnosis of salivary tumors in parapharyngeal space varies between 95% and 100%. The typical aspect of the pleomorphic adenoma at the MRI is a mass in isosignal T1, hypersignal T2 with a festooned contour [2,11].
The treatment of parapharyngeal tumors is surgical. Multiple approaches have been described. The choice depends on the size of the tumor, its site, its relationship to the tumor. with the surrounding vasculo-nervous structures and the surgeon’s experience. The best approach must allow for good exposure in order to identify and protect the vasculo-nervous structures while ensuring the following complete removal of the tumor [12]. The elective approach is the trans-parotid cervical approach [8]. The Trans-Oral route is reserved for small independent tumors of the parotid gland [9]. For our patient, we opted for the transoral approach, considering the benign aspect of the tumor and its location extra-parotidian. The only inconvenience was the size of this one. The operation was complete. The prognosis is usually good but is marked by a highrisk of recurrence after surgery and carcinomatous degeneration needing early surgical management and regular follow-up.
Conclusion
The parapharyngeal space is a complex anatomical region. Resection of tumors in this region can be difficult. Management of pleomorphic adenoma of the parapharyngeal space needs a complete radiological check-up. The distinction between tumors of the accessory salivary glands and tumors of the deep lobe of the parotid gland is necessary to guide the choice of the approach to adopt.
To read more about this article....Open access Journal of Otolaryngology and Rhinology
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers





No comments:
Post a Comment