Authored by Albena Momchilova*,
Abstract
Our purpose is to describe the effects of plasmapheresis on the ophthalmological status of patients with relapsing-remitting multiple sclerosis (RRMS) during remission and of one patient with neuromyelitis optica (NMO), and to seek a correlation with parameters of oxidative stress. Two male and three female patients with RRMS and one female patient with NMO were treated with plasmapheresis with subsequent measurement of the levels of immunoglobulins and oxidative stress parameters. Previous treatment included interferons for all patients. We evaluated 4 ophthalmological parameters including: best corrected visual acuity (BCVA), ophthalmological status with biomicroscopy and funduscopy, visual field and peripapillary retinal nerve fiber layer (RNFL) thickness. The follow up period was 24 months for the patient with NMO and an average of 13.6 months for the patients with RRMS. The status of all patients was improved according to the Expanded Disability Status Scale (EDSS) after the treatment, and they were free of relapses during the follow up period. Reduction of both immunoglobulins and reactive oxygen species (ROS) was observed after the plasmapheresis in all patients. Neither progression, nor worsening of the BCVA and the visual field-testing results were detected. The RNFL thickness showed thinning in the patient with NMO and thickening in one of the patients with multiple sclerosis (MS). The thinning of the RNFL in the NMO patient, however, could be due to her comorbidity of primary open-angle glaucoma, treated with triple antiglucomatous drops. The mean RNFL thickness in the rest of the patients remained stable. Plasmapheresis is demonstrated as a safe treatment option for patients with RRMS and NMO not only for the steroid- resistant acute episodes, but also as a basic one during remissions of the RRMS and non-acute episode of NMO as shown by the stability of the studied ophthalmological parameters.
Keywords:Plasmapheresis; Immunoglobulins A,G,M (IgA,IgG,IgM);Multiple sclerosis (MS);Neuromyelitis optica (NMO);Oxidative stress;Reactive oxygen species (ROS);Retinal nerve fiber layer (RNFL);Best corrected visual acuity (BCVA); Optical coherence tomography (OCT)
Introduction
Multiple sclerosis (MS) is a neurodegenerative disease characterized by axonal injury in the central nervous system (CNS), leading to progressive neurologic deficits. Evidence indicates that axonal damage occurs in the early stages of the disease, and axonal degeneration is directly related to permanent functional disability [1,2]. Axonal damage in patients with MS can be detected and quantified at the level of the retinal nerve fiber layer (RNFL) using ocular imaging technologies, such as optical coherence tomography (OCT) [3,4].Neuromyelitis optica (NMO) is an inflammatory demyelinating disease (IDD) of the CNS and probably the most common IDD apart from multiple sclerosis [5,6].
In the recent years was accumulated scientific knowledge, practical experience and clinical results created by the application of plasmapheresis for separation of human polypeptides. In our previous paper we reported significant benefits of plasmapheresis application to patients with neurological pathologies [7,8]. In MS disease with complex pathogenesis reactive oxygen species (ROS) could serve as a biomarker of oxidative stress that reflects only one of many ongoing pathogenic processes.
Accumulating evidence suggests that oxidative stress plays a major role in the pathogenesis of multiple sclerosis. ROS, which, if produced in excess, lead to oxidative stress, are implicated as mediators of demyelination and axonal damage in both MS and the corresponding animal models [9].The aim of the present study was to investigate the application of plasmapheresis in the treatment of certain neurological diseases such as multiple sclerosis and neuromyelitis optica.
Material and Methods
Patients
All patients have signed informed agreement before the performance of plasmapheresis.
Methods
The method of therapeutic apheresis – plasmapheresis, has been introduced in Bulgaria in 2013 [7,10,11]. For the period 2013- 2016 in Clinic of Neurology, in the Medical University of Sofia were performed 377 plasmaphereses on 30 women and 42 men [12]. The patients who underwent plasmapheresis in the Department of Intensive Treatment of Neurological Diseases “TsaritsaYoanna - ISUL” Sofia, had multiple sclerosis (16), polyneuropathy (7), myasthenia gravis (7), neuromyelitis optica (3), amyotrophic lateral sclerosis (6) and Charcot-Marie-Tooth (1) etc. All patients diagnosed with multiple sclerosis and neuromyelitis optica (Devic’s disease) underwent a full ophthalmic examination. Determination of ROS in blood plasma from patients before and after plasmapheresis was carried out in the Institute of Biophysics and Biomedical Engineering, Bulgarian Academy of Science, Sofia.
Therapeutic plasmapheresis
Therapeutic plasmapheresis is a method approved by the American Society for Apheresis (ASFA) for therapeutic apheresis [13]. The whole therapeutic procedure was performed by catheterization of a single peripheral vein, which makes this approach low-invasive and safe for the patient.
Method principle - processed with anticoagulants blood passes under pressure through a semi-permeable membrane (with different pore size) that transmits plasma and retains the shape elements (cells) which are returned into the bloodstream. Cascade plasma is obtained by a sequential arrangement of semi-permeable membranes, which are characterized with different pore size. This is a more recent form of treatment in which pathologic constituents of the plasma are separated, and the rest is returned to the circulatory system in humans. The filtering efficiency of protein and other molecules depends on:
• transmembrane pressure;
• the set size of pores of the membrane;
• effective surface area of the membrane in m2.
During the membrane principle of apheresis the anticoagulanttreated blood passes under pressure through a semi-permeable membrane (with different pore size) which transmits plasma and retains the cells which are returned into the bloodstream. The exact mechanism of the applied method of plasmapheresis is explained elsewhere [7].
After separation of about 0.7 liters of plasma from the intravascular space occurs a rapid reduction in the level of abnormal plasma proteins - pathological antigens, autoantibodies and antigen-antibody complexes. Through the semi-permeable separation membrane pass protein molecules and their complexes, which cause autoimmune diseases or are a result of pathological processes in the blood circulation upon tissue damage.
During the performance of therapeutic plasmapheresis it is very important that the type and volume of the replacement fluids (crystalloids, colloids or protein solutions) are correctly chosen, so that the intravascular volume of the circulating blood is properly maintained. The most frequently used fluid is physiological saline, which has the lowest cost and is with no adverse complications.
Optical coherence tomography
Optical coherence tomography (OCT) is a noninvasive, noncontact imaging system which provides high resolution crosssectional images of the retina, vitreous and optic nerve. Imaging of the anterior segment is also possible. OCT is analogous to B-scan ultrasonography but uses light instead of sound waves. Measurements were performed by directing a beam of light and measuring the echo time delay and magnitude of reflected or backscattering light using low coherenceinferometry. Crosssectional images are generated by scanning the optical beam in the transverse direction, thus yielding a two-dimensional data set that can be displayed as a false color or greyscale image [14].
Determination of ROS concentration
The level of ROS was assessed by spectrofluorimetric analysis, using dichlorodihydrofluorescein diacetate, which reacts with ROS to produce the highly fluorescent dihydrofluorescein. Fluorescence was measured at 485 (excitation beam) and 525 nm (emission beam). The level of ROS is presented as fluorescence intensity per mg protein.
Result
In this study we present two male and three female patients with relapsing- remitting form of Multiple Sclerosis with mean age 43.2 years [35-56] and one 50-year-old female patient with Neuromyelitis Optica, who were referred for an evaluation of the ophthalmological status. The patient with NMO has a duration of the disease of 5 years and a comorbidity with primary open angle glaucoma. The mean duration of the disease of the patients with MS was 14.8 years [8-27] and previous treatment included interferons for all patients and disease modifying therapy in one patient.
All patients were treated with plasmapheresis. For the patients with MS an initial course of 3 procedures within a week was performed. For the patient with NMO the first three procedures were performed within five months with interval of 2 and 3 months, respectively. The rest of the procedures were performed according to the treatment response of the patients.
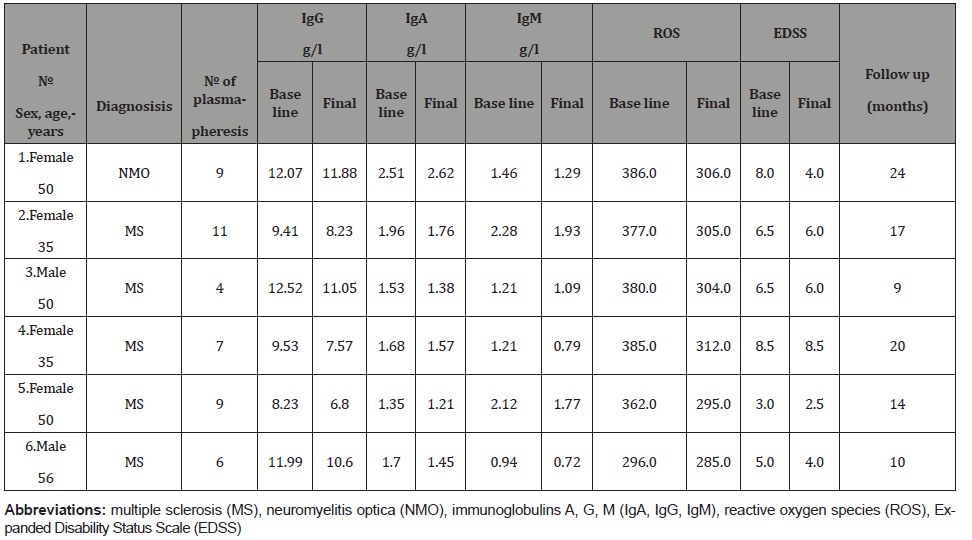
The neurological status was evaluated by neurologists and the disability of the patients was measured according to the Expanded Disability Scale Score (EDSS). MRI was performed in the patients for control of the disease activity.The plasma levels of immunoglobulins and of parameters of the oxidative stress like reactive oxygen species were measured before and after the plasmapheresis procedures (Table 1).
Table 1: Levels of the parameters of the oxidative stress before and after the first 3 plasmapheresis ROS and EDSS score before the treatment and after the last procedure.
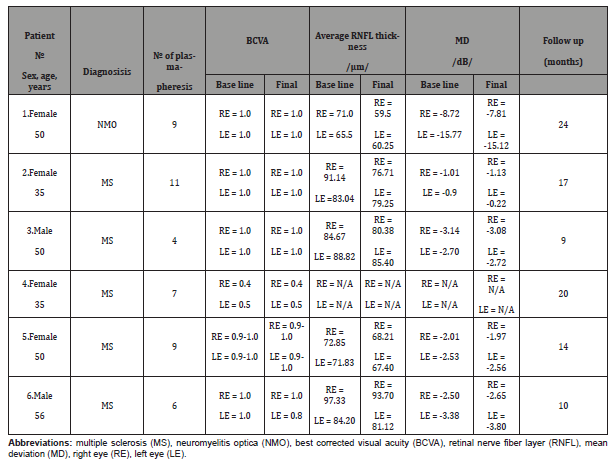
Five ophthalmological parameters were evaluated before and after plasmapheresis including: best corrected visual acuity (BCVA) and intraocular pressure (IOP), ophthalmological status with slitlamp biomicroscopy and fundoscopy, visual field testing (Humphrey Carl Zeiss, Jena, Germany) and optical coherence tomography (OCT) scanning (Stratus OCT, Zeiss Jena GmbH, Jena, Germany) of the peripapillary retinal nerve fiber layer (RNFL) thickness. OCT and visual field were not tested in one patient because of severe tremor.The primary endpoints were BCVA, average peripapillary RNFL thickness and mean deviation (MD) on the visual field testing after the initial plasmapheresis course in the patients with MS and after the third plasmapheresis in the patient with NMO.
There was a reduction in the levels of the immunoglobulins and reactive oxygen species in all patients after the plasmapheresis. Improvement in the neurological status regarding EDSS was observed after the treatment.
The BCVA, MD and RNFL thickness (Table 2) showed no significant changes with only a statistically significant thinning of the RNFL in the right eye of the patient with NMO. Eye pressure was in normal limits (14-17 mm Hg), during the follow up period, one patient with NMO was on triple antiglaucomatous treatment (Latanoprost, dorzolamide hydrochloride and timolol maleate) before treatment and during the follow up period.
Table 2: Changes of the ophthalmological parameters after treatment with plasmapheresis.
Although the patients were not experiencing an acute episode of the disease, they had residual deficit after previous relapses, which improved after the treatment. The observed reduction of the parameters of oxidative stress after the procedures corresponds with the improvement of the neurological status regarding EDSS. This beneficial effect is also in congruence with the reduction of the immunoglobulin levels. The greatest improvement that was detected in the patient with NMO could be explained by one of the possible mechanisms in the disease’s pathogenesis – IgG antibody against Aquaporin 4 and the seropositivity of the patient for this AQP4 – IgG.
The lack of significant RNFL thinning in the patients with MS indicates stability of the disease process. This was confirmed by the performed MRI scans. On the contrary, there was a significant reduction of the RNFL thickness in the right eye of the patient with NMO. The thinning of the RNFL in this patient, however, is less likely to be caused by a disease progression as the greatest improvement in the neurological status according to EDSS was observed in this case. The thinning is rather caused by the patient’s comorbidity with primary open- angle glaucoma. The patient had significant glaucomatous thinning of RNFL, before iniciate the treatment.
Limitations of our study are the little number of patients, the comorbidity of the patient with NMO with primary open angle glaucoma and the possible natural course of the disease as a reason for the stability of the studied ophthalmological parameters. Plasmapheresis treatment can be used with good results in patients with relapsing- remitting form of Multiple Sclerosis in remission, and with some residual neurological deficit in patients with Neuromyelitis Optica, while not experiencing an acute episode of the disease. The stability of the RNFL thickness in addition with that of the BCVA and the lack of changes on the visual field testing indicate the safety of this type of treatment.
We carried out a course of 4 sessions of plasmapheresis with subsequent performance of 1 procedure each month, with a very favorable result for the patient.Plasmapheresis was carried out in accordance with the sixth revised edition of the “Guidelines on the Use of Therapeutic Apheresis in Clinical Practice-Evidence-Based Approach from the Writing Committee of the American Society for Apheresis” [13], and the rules developed for plasmapheresis in Bulgaria [15]. After the last (fourth) procedure was observed an apparent clinical improvement, which was assessed according to the international scale of Kurtzke EDSS.
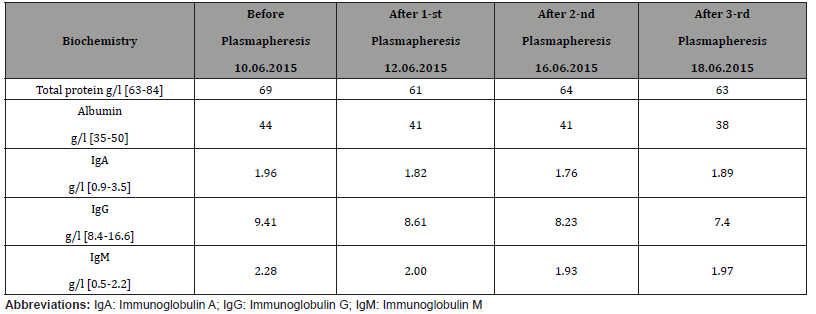
The values of total protein, albumin and immunoglobulins in plasma after the plasmapheresis procedures are shown in (Table 3)for a patient with multiple sclerosis. As evident from the table, the level of albumin, IgG and IgM were gradually reduced after each subsequent procedure.Plasmapheresis sessions were well tolerated without complications or side effects. After the procedure our patient was able to stand from the wheelchair and to start walking. She had no complains and her eye status remained stable.
Table 3: Alterations in the level of proteins and immunoglobulins before the initiation of the procedures and after each separate plasmapheresis (patient with multiple sclerosis).
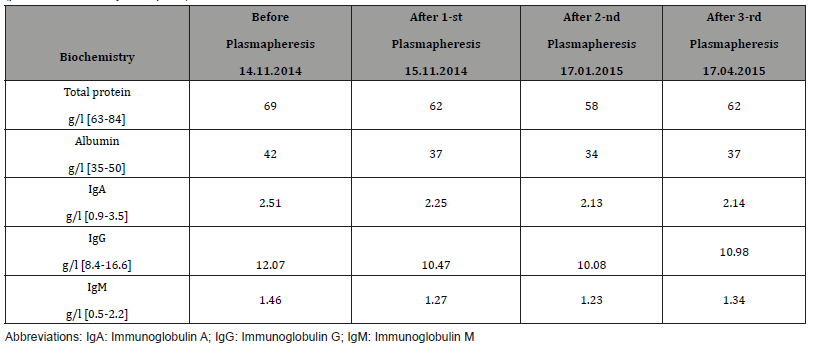
The values of total protein, albumin and immunoglobulins in plasma after the plasmapheresis procedures are shown for a patient with neuromyelitis optica in Table 4. As evident from the Table 4, the protein content, expressed as grams per liter (g/l) was reduced gradually with each next procedure, and was elevated slightly after the last (third) session. The same pattern was valid for the alterations in the content of blood plasma albumin, as well as for the three types of immunoglobulins: A, G and M (Table 4).
Table : Alterations in the level of proteins and immunoglobulins before the initiation of the procedures and after each separate plasmapheresis (patient with neuromyelitis optical).
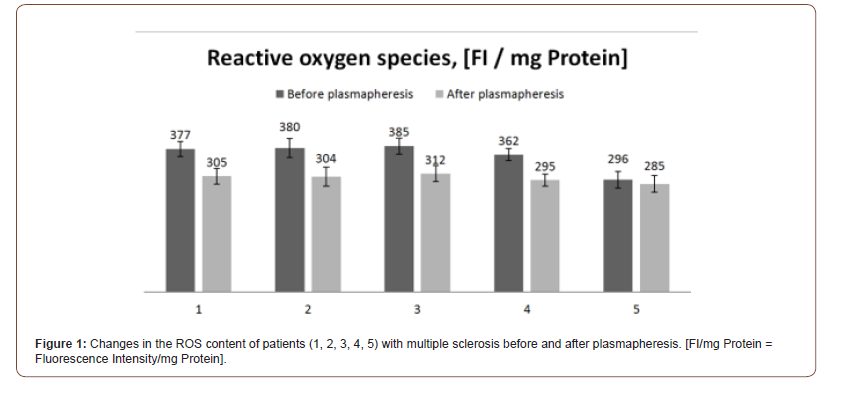
The levels of the parameters of immunoglobulins (IgG, IgA, IgM) before and after the plasmapheresis and EDSS values before the treatment and after the last procedure are shown in Table 1.Oxidative stress was also assessed in the treated patients because it is considered as pathogenic factor in the development of neurodegenerative diseases. The degree of oxidative stress was estimated by measuring the content of ROS, which are accepted as relevant markers for development of oxidative stress. The changes in the level of ROS of the patients with multiple sclerosis, are presented in (Figure 1). The results show that the performance of plasmapheresis was accompanied by a reduction of the level of ROS, indicating that each procedure induced a decrease in the overall degree of oxidative stress of the patients with multiple sclerosis.
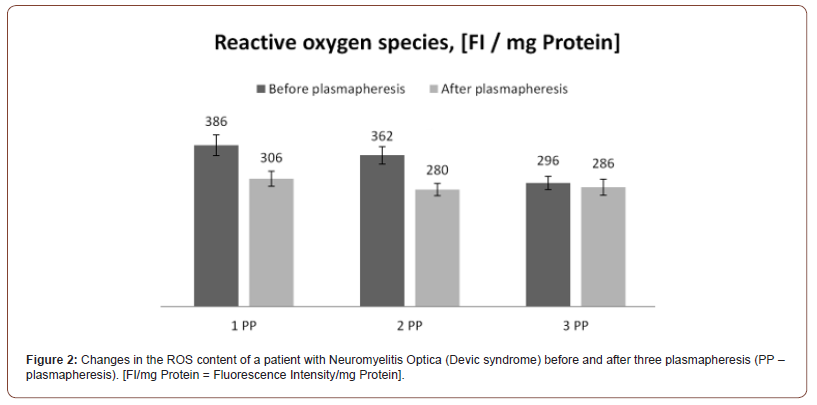
The changes in the level of ROS of the patient with neuromyelitis optica, are presented in Figure 2. The results show, that the performance of each session of plasmapheresis resulted in reduction of the level of ROS, indicating that each procedure induced a decrease in the overall degree of oxidative stress of the patient with neuromyelitis optica.
Ophthalmological examination
The results from the ophthalmological examination of the patient with neuromyelitis optica showed that the best corrected visual acuity (BCVA) was 1.0 of both eyes before and after the plasmapheresis procedures. The IOP was between 14 and 17 mmHg in both eyes and the patient had thin central corneal thickness (CCT): 520 microns in both eyes, which is an independent risk factor for glaucoma.
There was a thinning of the retinal nerve fiber layer (RNFL) in both eyes (significant thinning in the inferior quadrant in both eyes and borderline thinning in the superior and nasal quadrants in the right eye) (Figure 3 c,d, patient with neuromyelitis optica). The Cup/Disc ratio of the right eye was 0.7 and 0.8 of the left eye. The computed perimetry shows glaucomatous paracentral and superior-nasal scotoma in the right eye (Figure 3a) and an upper arcuate defect with peripheral breakthrough in the left eye (Figure 3b-3d).
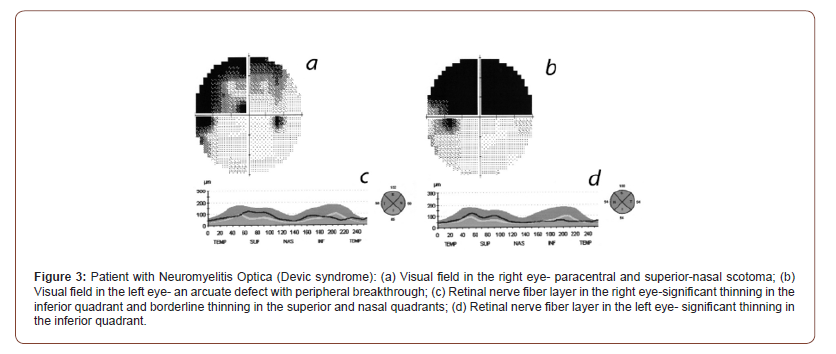
The alterations in the ophthalmological parameters after treatment with plasmapheresis are presented in Table 2.At this point it is difficult to differentiate whether the changes in the eyes are caused by Devic’s disease or by the glaucoma as both diseases affect the optic nerve. However, optic nerve damage is caused mainly by glaucoma because thinning of the RNFL is in the inferior part (typical sighs of ISNT rules in glaucoma patients) and the specific changes found on the specialized eye examinations. Still, the progression of the RNFL thinning in both eyes suggests that there could be additional damage due to Devic’s disease (bearing in mind that the intraocular pressure is well maintained with topical therapy).
Discussion and Conclusion
The reported results suggest that therapeutic plasmapheresis can be used successfully for maintaining treatment of MS and most importantly, it does not induce the side effects like most of the currently used therapeutic approaches. The obtained results give us grounds to recommend this method as a reliable component in a complex MS therapeutic approach besides medications, physiotherapy and diet.The data reported in this study imply that the application of therapeutic plasmapheresis to a patient with neuromyelitis optica induces reduction of blood plasma levels of immunoglobulins and ROS as well as improvement of the patient’s ophthalmological status. Thus, the presented evidence in this work suggests that the use of plasmapheresis will contribute for elevation of the effectiveness of the therapeutic approach applied to autoimmune diseases, such as neuromyelitis optica.
Optical coherence tomography is a sensitive technique for detecting optic nerve injury. OCT may reflect subclinical disease or progressive axonal attrition in the clinically unaffected eye [16]. Retinal nerve fiber layer (RNFL) atrophy in patients with MS is a structural marker for axonal injury in the afferent visual pathway. OCT-measured RNFL values are reduced in patients with MS with and without a history of optic neuritis (ON), but the RNFL atrophy tends to be greater in ON-affected eyes [17-18]. With the technological adjustment and the availability of the new spectral domain OCT apparatus, a more detailed differentiation and analysis of the retinal layers is possible. Using these new technologies, a thinning of all retinal layers except the inner limiting membrane in patients with multiple sclerosis was demonstrated. More serious changes in the inner retinal layers are found in eyes, which were affected by optic neuritis. Ganglion cell/Inner plexiform layer (GCIP) thinning is more indicative of the severity of the systemic disease than RNFL thinning. Macular GCIP thinning is more closely associated with radiologic and clinical measures of MS progression than is RNFL thinning. Hereafter, it would be reasonable to state that GCIP thickness could predict axonal damage in patients with MS and may become the preferred method of monitoring MS progression in the eye [19-20].
Since there is evidence in the literature suggesting that oxidative stress plays a significant role in the pathogenesis of neurodegenerative pathologies, including multiple sclerosis, we assessed the effect of plasmapheresis on the patients’ oxidative status by measuring the plasma ROS level before and after the performance of the corresponding procedure. Oxidative stress leads to accumulation of free radicals, which are highly reactive molecules and, when interacting with other molecules, induce their oxidative destruction. Free radicals interact with cellular lipids, proteins and nucleic acids, thus changing the structure and functional activity of native cellular components, and very often turning them into free radicals. In this way, a free-radical-forming chain reaction is created that adds real chaos to the structure and functions of the cells and tissues of the body.
Figure 1 shows the levels of ROS in blood plasma of a patient with MS after three subsequent procedures of plasmapheresis. The results show that the performance of each plasmapheresis is accompanied by a decrease in the level of ROS, which means that each procedure induces a reduction in the overall degree of oxidative stress of the patient.
Similar results have been observed for the patient with neuromyelitis optica (Figure 2) after three subsequent plasmaphereses. Thus, the observed results gave us grounds to suggest, that the performance of plasmapheresis procedures to patients with neurodegenerative problems reduces significantly the level of oxidative stress.
These changes in the patient’s oxidative status are favorable for the particular neurodegenerative disease as well as for the patient’s general condition. Since it is believed that elevated levels of oxidative stress are the cause of the onset and development of pathologies such as inflammation, neoplastic processes, etc., the reduction of the parameters indicative of oxidative stress is a basis for a more favorable prognosis for each pathological condition. Since, according to one of the theories of pathogenesis of a wide range of neurodegenerative pathologies, oxidative stress can play a role both in the initiation and development of the disease itself, limiting this type of stress at the organism level can contribute to the management of symptoms and preventing further development of the corresponding pathology.
In conclusion, the presented results clearly show that performance of plasmapheresis induces a marked reduction of the plasma level of ROS of patients with neuromyelitis optica and MS. Thus, we suggest that the application of plasmapheresis in the therapeutic practice can provide good clinical results and could contribute to improvement of the blood plasma biochemical parameters of patients with neurodegenerative diseases.
To read more about this article....Open access Journal of Biomedical Engineering & Biotechnology
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers





No comments:
Post a Comment