Authored by Raed Madhi*,
Abstract
Coronavirus disease 2019 (Covid19) is a viral-provoked respiratory disease that affects many patients worldwide. Clinical manifestations start with mild flu-like symptoms and progress to acute respiratory distress syndrome (ARDS), the trigger of which has been underpinned as cytokine storm. Neutrophil-derived neutrophil extracellular traps (NETs) greatly contribute to development of Covid19 severity. It has been hypothesized that nebulized lidocaine could be used to attenuate the severity of Covid19, however, the mechanism by which this may occur not completely clear. This review addresses the possibility of using nebulized lidocaine as a therapeutic approach for targeting Covid19-induced NETs formation.
Keywords: Covid19; Cytokines; Neutrophil; Neutrophil extracellular traps; Lung damage; Nebulized lidocaine
Abbreviations: Covid19-Coronavirus disease 2019; ARDS-Acute Respiratory Distress Syndrome; NETs-Neutrophil Extracellular Traps; SARSCoV- 2-Severe Acute Respiratory Syndrome Coronavirus 2; ACE2-9-Angiotensin Converting Enzyme 2; G-CSF-Granulocyte Colony Stimulating Factor; MCP1-Monocyte Chemoattractant Protein 1; STAT3-Signal Transducer And Activator of Transcription 3; CF Cystic Fibrosis; NE-Neutrophil Elastase
Introduction
The WHO (World health organization) has declared that coronavirus disease 2019 (Covid19) is a disease of pandemic proportion that causes severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) [1]. It well known that lung is the most common organ infected by Covid19 and this could be due to high expression of angiotensin-converting enzyme 2 (ACE2) receptor in lung tissue [2,3]. The severity of Covid19 has been shown to be associated with elevated viscus mucus secretions in the airways, pro-inflammatory cytokine production, leukocyte recruitment and extreme lung damage. Because of the difficulty in management of this disease at late stage, it has induced fatality a large number of patients [4-6]. Serval studies have observed neutrophil infiltration increases in the lungs during Covid19 infection [7,8]. And it has been suggested that neutrophilia are a source of excess NETs and the hallmarks of acute infection of Covid19 [6]. In this review, I hypothesize that targeting Covid19-induced NETs by nebulized lidocaine could be a useful strategy for reducing the severity of Covid19 in patients and for decreasing the overall associated mortality rate.
NETs and Cytokines Production
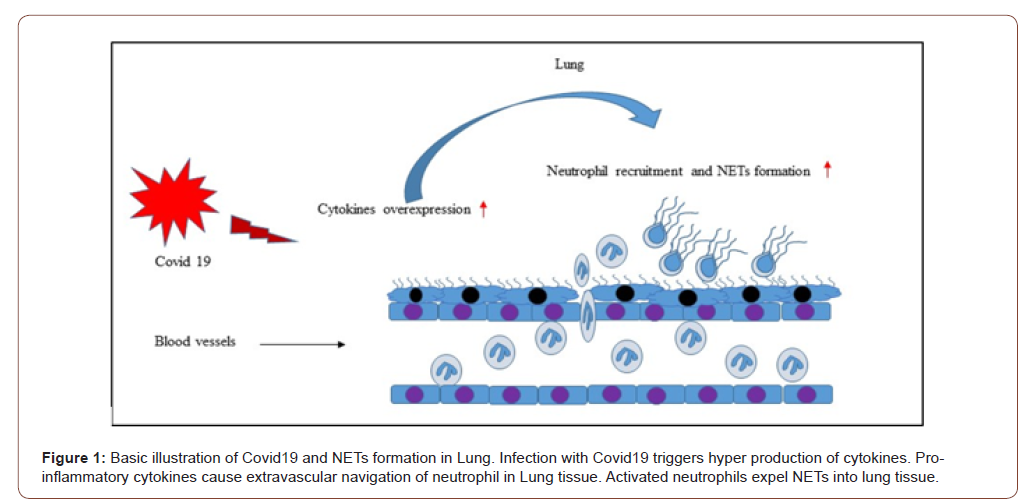
The severity of Covid19 has been shown to be associated with cytokine production. For instance, it was observed that levels of TNFα, MCP1, G-CSF, IL17, IL10, IL8, IL7, IL2, IL1β are elevated in the plasma of patients with Covid19 [9-13]. In fact, these cytokines serve as inflammatory mediators that mediate neutrophil activation and chemoattractant production. Neutrophil extravasation into inflamed tissue has also been documented to be mediated by these chemoattractant [14,15]. NETs can activate macrophages to secrete TNFα, which in turn, enhances the release of NETs in different diseases, including lung inflammation and arthritis [16]. Indeed, infection with Covid19 has been shown to increase the levels of TNFα [17] and it has been suggested this may lead to accelerated formation of NETs (Figure1). A recent study has found that NETs can regulate transcription factors such as signal transducer and activator of transcription 3 (STAT3) [18]. This transcription factor has been found to control the expression of a verity of genes involved in onset of cytokine storm which is capable of exuberating pulmonary injury. Moreover, it was reported that NETs formation is associated with increased levels of plasma IL-6 [19]. This proinflammatory cytokine was found to mediate STAT3 activation [20]. Taken together these findings strongly suggest targeting these pro-inflammatory cytokines (TNFα and IL-6) could be involved in decreasing NETs formation in severe Covid19.
NETs and Leukocyte Recruitment
During their activation, neutrophils have been observed to expel extracellular traps against invading pathogens [21]. However, disorder of NETs clearance or excessive NETs formation have been found to participate in tissue damage in both non‐infectious diseases and infectious diseases [14,22]. The direct role of NETs in leukocyte recruitment has not examined, however, numerous studies have shown indirect evidence in which inhibiting or disintegrating NET formation was found to reduce the recruitment of inflammatory cells in models of inflammation [15,22]. Leukocyte extravasation is a gradual multistep process mediated by adhesion molecules expressed on both leukocytes and endothelial cells [23]. Accumulating data report that the selectin family of adhesion molecules (P, E, and L‐selectin) provide a crucial support of leukocyte rolling via binding with their glycoprotein ligands [24, 25]. A study by Wang Y, et al. [26], has shown that NETs stimulate neutrophil rolling, adhesion, and extravasation in the microvasculature of cremaster tissue. The authors found that immunoneutralization of selectins, such as P-selectin, greatly attenuated NET-triggered neutrophil rolling and emigration [26]. Indicating that NETs cause self-amplifying loop via increase neutrophilia and chemotaxis. Indeed, Covid19 has been documented to elevate NETs formation in sera of patients with Covid19. Moreover, a recent study has been observed that incubation of healthy neutrophil with Covid19 patients’ sera results in triggering NETs release form control neutrophil [27]. And NETs formation has been shown to positively provoke neutrophilia and neutrophil extravasation into lung tissue [28].
NETs in Pulmonary Damage
Accumulating data have reported that NETs formation is extensively linked to pulmonary diseases. Lingtao Luo et al. [22], have observed that NETs control pulmonary extravasation of neutrophil and tissue damage via regulating pro-inflammatory compounds in septic lung injury [22]. A previous study has found that NETs cause direct damage to epithelial and endothelial cells possibly via histone proteins, a major component of NETs [29]. Indeed, it was documented that levels of NETs are increased in the plasma of patients with acute respiratory distress syndrome (ARDS) [30]. Moreover, extracellular histones have been observed to increase in both plasma and bronchoalveolar lavage fluid of patients with ARDS [31]. Experimental studies have shown that NETs are involved in the development of ARDS and that either preventing production of or destruction of the same may protect against lung damage and increase survival [30,32-34]. Yongzhi Wang, et al. [35], found that NETs are dependent on thrombin formation and that dissolution of NETs formation antagonized sepsis-induced thrombin generation [35]. It has also shown that ARDS, sepsis, and multi-organ dysfunction syndrome are the most common complications of Covid19 [36,37], and thus targeting NETs is a potentially novel therapeutic strategy for attenuating the severity of Covid19.
Nets in Cystic Fibrosis
The severity of cystic fibrosis (CF) is attributed to accumulation of mucous purulent secretions in the airways. A previous study has observed that viscosity of these purulent secretions increases greatly in the presence of large amounts of extracellular DNA, a major component of NETs. The authors found that disintegration of extracellular DNA in purulent sputum of patients with CF reduced the viscosity and transformed the sputum from the gel-like structures to flowing liquid within minutes [38]. Neutrophil elastase (NE) has been shown to be one of the most granular proteins that constitutes NETs [39]. Overexpression of NETs with increased NE can elevate the viscosity and mucus thickness of purulent secretions in the airways of cystic CF fluid. Accordingly, mucus secretions have been reported to impair gas exchange as well as facilitate bacterial colonization in the lungs [40]. Consequently, colonization of bacteria can further stimulate neutrophil extravasation and recruitment as well as NET formation, and this in turn may increase the viscosity of secretions in the airways and cause respiratory dysfunction. Indeed, patients with Covid19 have been found to have mucous secretions in the airways of the lungs [41] and these secretions seem to be similar to those seen in patients with CF. Therefore, if the secretions of Covid19 patients contain NETs, then it is possible they play a similar role in this disease to that which they play in CF (i.e. encourage/induce respiratory dysfunction and facilitate bacterial colonization in the lungs).
Lidocaine and Covid19-induced NETs formation
Lidocaine or xylocaine is a chemical compound that causes local anesthesia via blocking nerve signals. Consequently, neurons consistently become unable to transmit signals to the brain. This medication was first introduced in 1946 as an anesthetic which can be administrated via many differing approaches, e.g. intravenous, subcutaneous, topical, and oral. Lidocaine can provide sedation starting- within minutes and lasting for up to several hours [42].
Indeed, lidocaine has recently been used to treat patients with acute asthma. It has been shown that nebulized inhalation of lidocaine can greatly reduce bronchial hypersensitivity in patients with acute asthma [43]. Caracas HC, et al. [44], have reported that lidocaine has a potential anti-inflammatory role in infectious and non-infectious diseases [44]. Moreover, a previous study has investigated the effectiveness-of lidocaine on leukocyte recruitment in surgical wounds in animal models. The authors have observed that treatment with lidocaine greatly attenuated the migration of leukocytes in surgical wounds [45]. Pro-inflammatory cytokines have been shown to stimulate the recruitment of leukocytes into the inflamed sites [46,47]. In fact, an experimental study has found that administration of lidocaine through both inhalation and intravenous injection resulted in a significant reduction of IL-6, TNF-α and IL-1β in lung tissue [48]. Moreover, it was also documented that intravenous administration of lidocaine greatly increased levels of the anti-inflammatory cytokine IL-10, in mechanically ventilated animal lungs [49]. In addition, clinical studies have found that receiving lidocaine can attenuate levels of pro-inflammatory cytokines [50,51]. Thus, the anti-inflammatory effect of lidocaine on cytokine production could in part explain the inhibitory effect of leukocyte migration.
It is well established that mucus clearance is an important mechanism for lung health and that disorder of this mechanism may led to disease of airway. Healthy mucus secretion is characterized as secretion of a gel-like substance of low viscosity and elasticity which can easily be transported through ciliary action. However, it has been demonstrated that in certain pulmonary disease pathologies the viscosity and elasticity of mucus is increased, and this leads to a subsequent decrease in mucus clearance that is debilitating for pulmonary function [52,53]. Moreover, it has been shown that the mucus of cystic fibrosis patients contains infiltrated neutrophils with high concentrations of neutrophil-derived extracellular DNA and actin filaments [54-56]. Another study has also documented that NETs formation represents the essential extracellular component of CF [40] and a recent study in a murine model of asthma has found that nebulized lidocaine attenuates airway inflammation and peribronchial fibrosis as well as mucus overproduction [57]. In addition, Elena et al, 2020 have been found that administration of lidocaine greatly attenuated NETosis in patients with breast cancer [58]. Importantly, the severity of Covid19 has been shown to be characterized by elevated neutrophil infiltration and mucous secretions in the airways of the lungs [28]. Furthermore, it was found that NETs formation increased in the sera of patients with Covid19 and that NETs can be used as a marker for the severity of Covid19 [27].
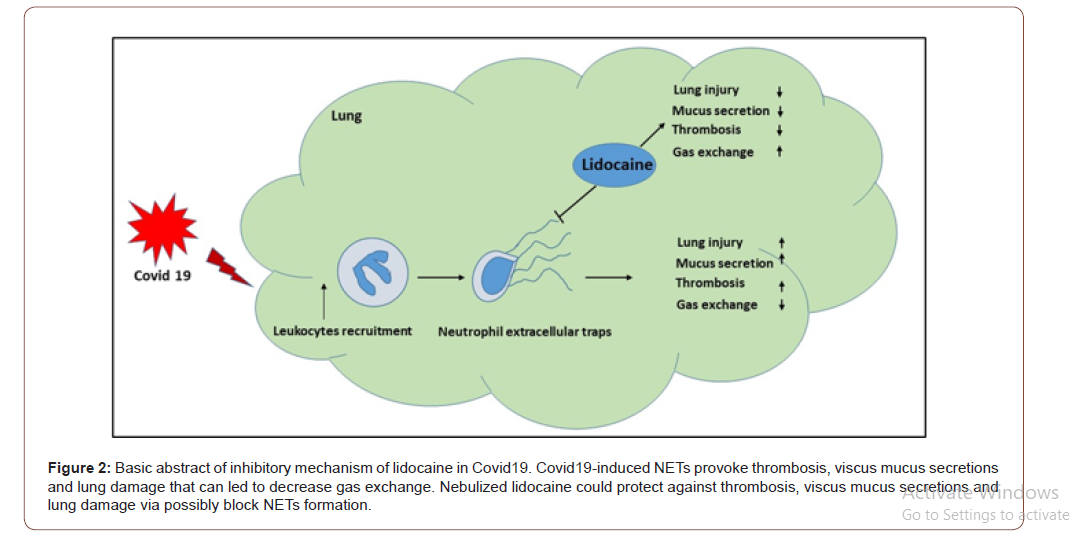
In this review, I highlighted that in addition to providing a local sedation, nebulized lidocaine could potentially be used as a future therapeutic approach for targeting Covid19-induced NETs formation and by this means protect against viscus mucus secretion and airway inflammation to protect/enhance lung function in Covid19 patients (Figure 2). Thus, future studies are warranted to investigate the possibility of nebulized lidocaine in targeting Covid19-induced NETs in patients with Covid19.
To read more about this article...Open access Journal of Anaesthesia & Surgery
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers
To know about Open Access Publishers





No comments:
Post a Comment