Authored by Omar El-Mowafy*,
Introduction
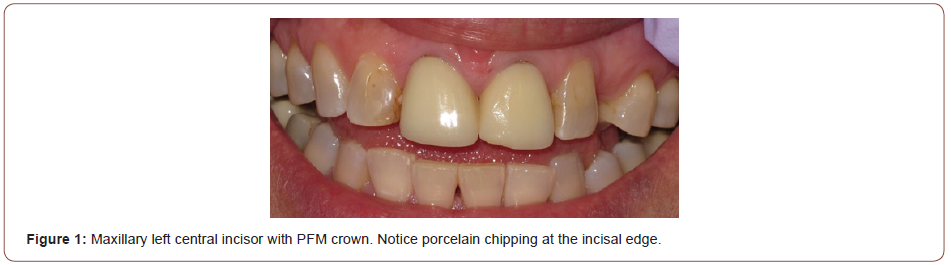
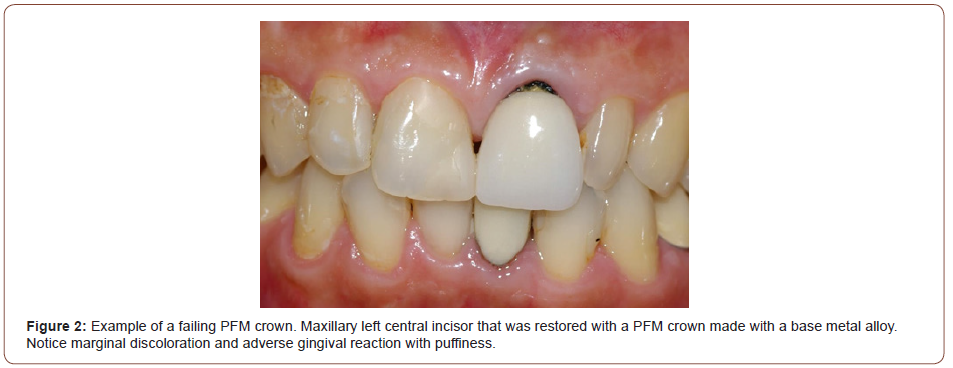
Over the past few years, dentists’ utilization of the traditional porcelain-fused-to-metal (PFM) crowns has dramatically dwindled and the utilization of metal-free crowns has swiftly increased. This is due to a new high-precision manufacturing technology, CADCAM, and new reliable materials that emerged on the horizon. PFM crowns combine the strength of the underlying metallic coping with the esthetics of the veneering porcelain to produce esthetically-pleasing crowns. However, PFM crowns have inherent drawbacks. They are fabricated made following an ailing lost wax technique, used in dentistry for 70 years, to cast a metal coping to which veneering porcelain is manually added by a skilled ceramist, a process fraught with inadvertent incorporation of small voids in the porcelain mix. These compromise the structure and may lead to crack formation s and eventual chipping of the veneering porcelain under forces of mastication (Figure 1). Furthermore, the underlying metallic core can be made from several types of alloys including noble, semi-precious and base metals. While all metal alloys may cause some level of gingival inflammation around the margins of the crowns, base metal alloys, in particular, can lead to significant staining and discoloration around the crown margins (Figure 2). In addition, metal copings interfere with the light transmission through the crown which contributes to an undesirable level of high opacity.
In contrast, when using the CAD-CAM technology, the manual skills of a skilled ceramist are not needed. A digital impression using an intra-oral scanner or Scanning of an impression or stone model of a tooth prepared for crown creates a virtual digital model. This rendering is used to design the restoration with digital software and communicate with the milling hardware. on which a virtual crown can be designed form virtual crown formats already available in the system. The An attached milling machine is capable of milling a restoration crown out of a partially-crystallized, in the case of lithium-disilicate glass-ceramic (LDGC), or partiallysintered, in the case of zirconia, block of the material of choice. This milled restoration is further subjected to a programmed thermal cycle in a furnace for full crystallization or sintering. Therefore, when restoring anterior teeth with crowns, dentists currently have a range of reliable materials (glass-ceramic, zirconia and high-translucency zirconia, and arrangements (monolithic and bilayered) to choose from unlike in the past where the only option was PFM crowns.
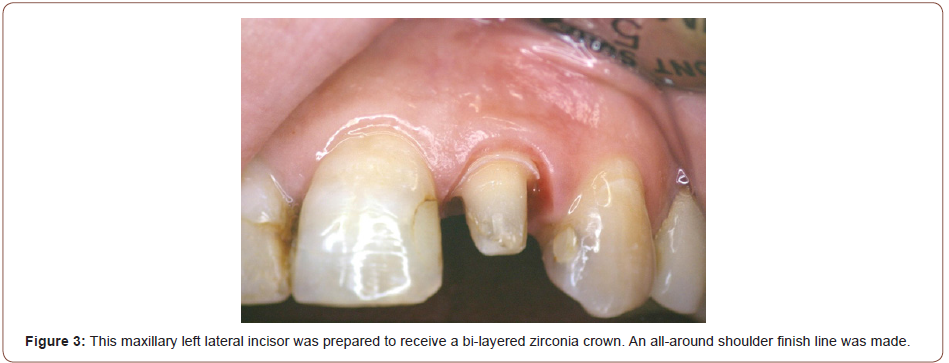
Both LDGC and high-translucency zirconia are typically used in the monolithic mode in anterior teeth as they lend themselves well in such applications. The main advantage of the monolithic restorations mode is lack of a joint linking a coping to veneering porcelain, thus eliminating the possibility of veneering porcelain chipping or delamination. However, monolithic crowns are typically made from a uniform translucency block with characterization achieved through surface shading at the glazing stage. The bilayered arrangement permits addition of veneering porcelain of varying different translucencies that may enhance the overall esthetic outcome (Figure 3&4).
CAD-CAM crowns also offer the advantage of manufacturing restorations chair-side when an in-house milling system can also be directly manufactured chair-side if a scanner/milling system is available. The ability to provide same-day restorations eliminates the need to fabricate provisional restorations. This have much more advantages over the indirect method including elimination of the need for fabrication of a provisional crown. However, chair-side systems can be are costly and maintaining up-to-date equipment can pose a challenge as CAD-CAM technology is rapidly and everevolving.
Dentists must weigh the cost against the expected return. Moreover, chair-side systems tend to get outdated fairly quickly with new improvements in software constantly made.
Case Details
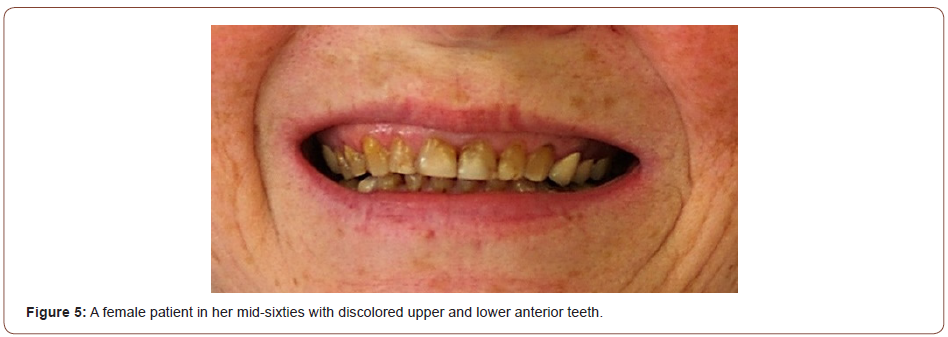
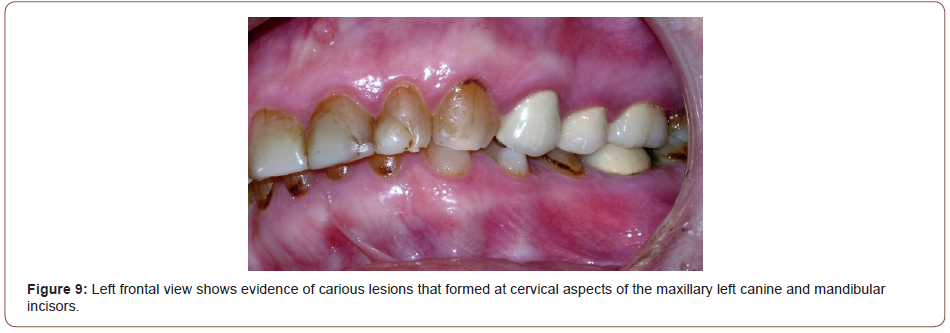
A 64 year-old female presented with the chief complaint of dark anterior teeth. She was interested in receiving treatment to improve the color of her anterior teeth. The patient’s medical history was non-contributary. CA clinical examination revealed that the maxillary anterior teeth were dark in color and heavily restored (Figure 5-9). Her lower anterior teeth were also dark in color, had incisal restorations and cervical carious lesions. Occlusion analysis revealed that the posterior teeth were in group function with excessive anterior overbite.

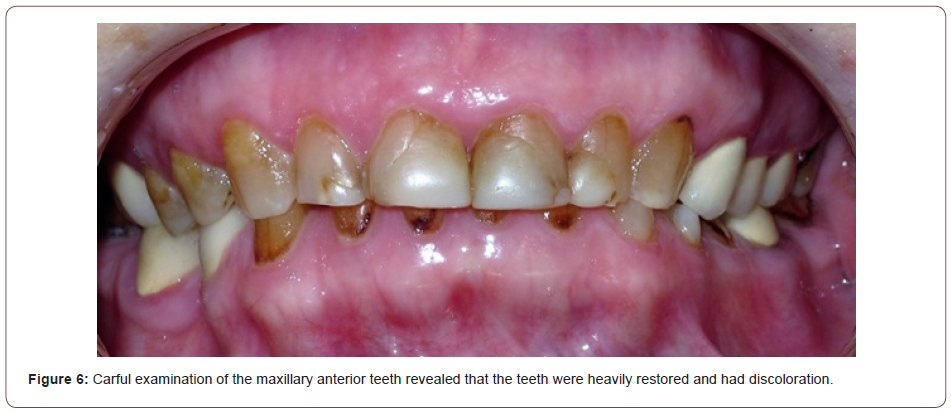

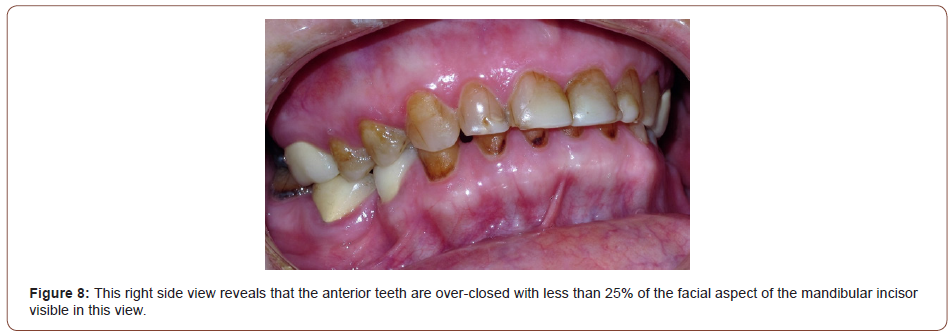
Periodontal probing of the maxillary and mandibular anterior teeth revealed that pocket depths were as within normal limits. A survey of a set of radiographic images of upper and lower anterior teeth revealed no abnormalities with bone level that was within normal limits. Vitality of all anterior teeth was verified with an electric pulp tester. All anterior teeth tested vital. A diagnostic wax mock-up of both dental arches was made. This was used to communicate the shape, size and form of the planned restorations. discuss with the patient the shape and size of the crowns to be made. It would also be used to fabricate silicone indices used for the fabrication of provisional crowns once the teeth were prepared.
The proposed treatment plan included providing all maxillary and mandibular anterior teeth with monolithic lithium disilicate glass-ceramic crowns fabricated using made with CAD-CAM technology blocks. When discussing shade selection, Shade selection was made at this point and the patient indicated her desire to have restorations made that she was interested in having her crowns made with shade a to match the lighter side of the spectrum of the shade guide. The patient was given a choice between two shade tabs, 1M1 and bleached shade, ultimately the patient elected to proceed with shade 1M1. She was unable to make her mind right away, therefore, she was given the two tabs to take home and decide at her convenience. At the next appointment, the patient indicated that she wished to proceed with shade 1M1. As part of the informed consent process, the patient was then explained that the procedure of providing crowns to vital teeth is associated with a small risk, less than 5%, of loss of vitality. The patient understood and agreed to proceed with the proposed treatment.
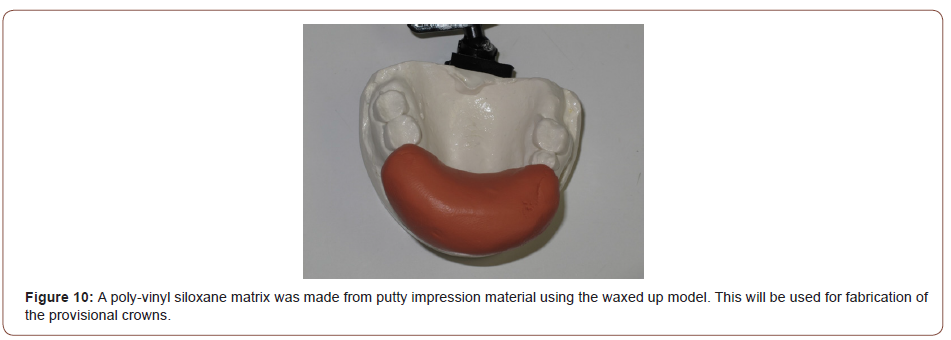
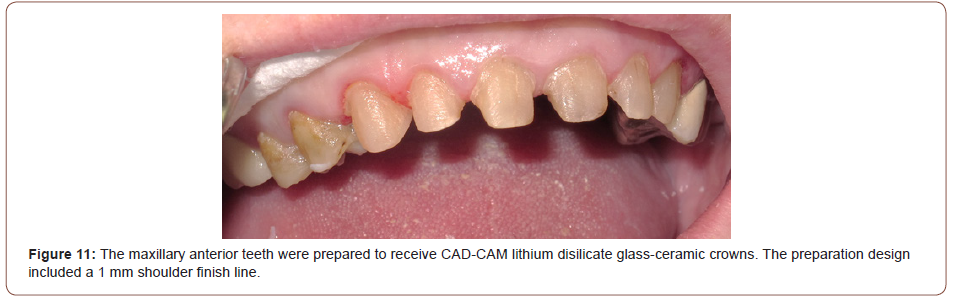
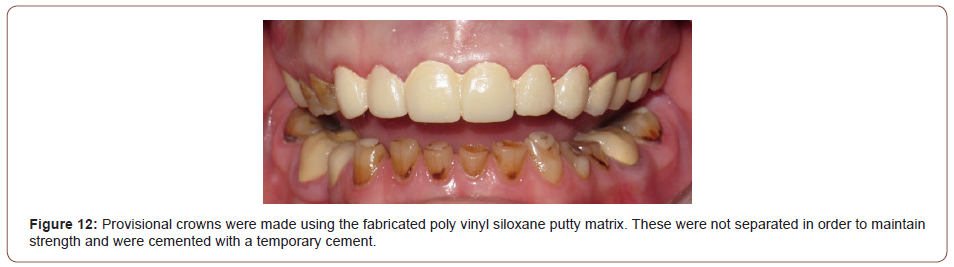
In one long appointment, all six maxillary anterior teeth were prepared to receive LDGC crowns. The preparation included an all-around 1 mm wide shoulder finish line that was located equigingival (Figure 10). The This would provide adequate support to the LDGC crowns. Incisal reduction was limited to 1.5 mm. A poly vinyl siloxane (PVS) impression was taken in a stock tray using a putty and/light body combination (Express, 3M/ESPE). A PVS putty VS index matrix of the for maxillary anterior teeth was fabricated from the diagnostic made with PVS putty from the waxed up wax-up cast model (Figure 11). The index matrix was loaded with temporary crown material using an auto-mixing device (Protemp, 3M/ESPE). After initial setting, the provisional crowns were retrieved from the matrix and excess flash was removed with a finishing disc. No attempt was made to separate the crowns this is in order to maintain their integrity. The provisional crowns were tried-in, finished and polished and luted cemented with a temporary cement (Temp-Bond, Kerr). Figure 12 shows the maxillary anterior teeth after cementation of the provisional restoration temporary crowns.
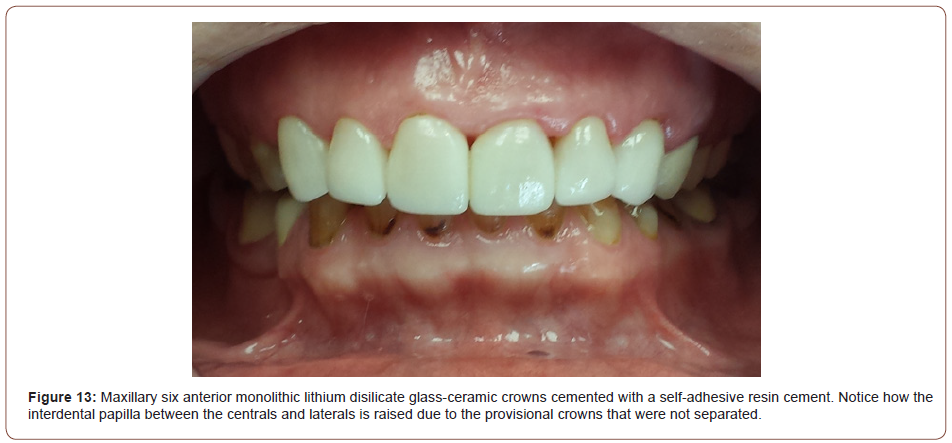
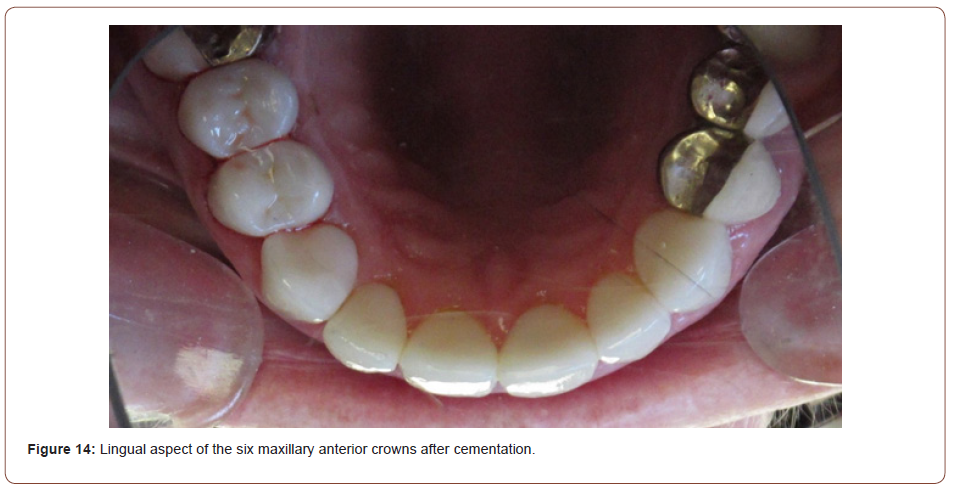
Six monolithic CAD-CAM LDGC crowns were fabricated made by at a commercial dental laboratory. The crowns were milled out of e.Max LDGC blocks (Ivoclar-Vivadent) before they were fullycrystallized in a furnace. The crowns were only glazed without any staining shading. The intaglio surfaces of the crowns were etched with a hydrofluoric acid gel before being treated they were coated with a layer of a silane coupling agent. The hydrofluoric acid etches the glass particles and provides a microscopically rough surface that enhances bonding. The silane coupling agent bonds well to the treated intaglio surface of the crown on one side and to the resin cement used for cementation of the crowns on the other side. At the next appointment, the provisional crowns were removed and the LDGC crowns were tried-in. All restorations were inspected and deemed acceptable with respect to marginal integrity, occlusion and proximal contacts as well as confirmed satisfactory esthetics with the patient. The restorations all fitted well and were cemented one pair at a time beginning starting with the two central incisors. A dual-cure self-adhesive resin cement was used for this purpose (Rely-X Unicem, 3M/ESPE). The inter-dental papillae between the centrals and laterals were slightly receded lifted as a result of the splinted due to the fact that the provisional crowns were not separated (Figure 13&14). However, they would heal to their normal position over a short period of time as can be seen in photos subsequent photos subsequently taken.
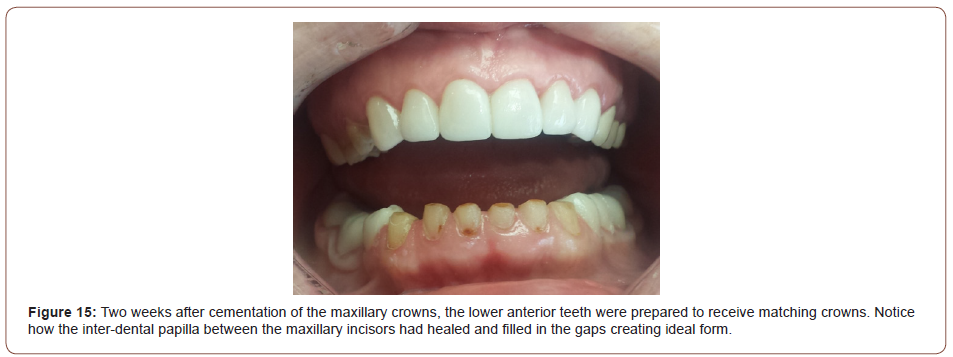
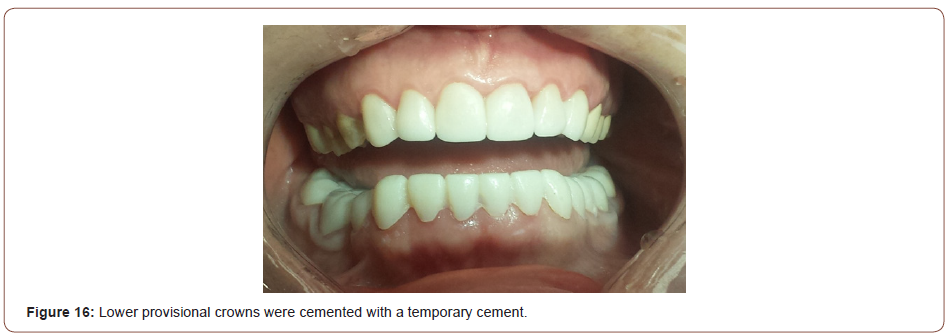
At the next appointment, the mandibular six anterior teeth were prepared for LDGC crowns (Figure 15). No attempt was made to restore the cervical carious lesions that existed in some of the teeth as these were shallow and were eliminated during in the crown preparation procedure. The final impression of the prepared abutments was carried out taking following the same procedure as described previously. Splinted provisional restorations were again fabricated based off of the diagnostic wax-up and were luted with followed and provisional crowns were made and cemented as for the maxillary teeth from a matrix that was made from the waxed up lower model. Provisional crowns were not separated and were cemented with a temporary cement (Figure 16). Six CAD-CAM LDGC crowns were fabricated by made at the same commercial dental laboratory. The final restorations were tried-in, treated and were cemented following the aforementioned protocol as above (Figure 17).

Conclusion
In conclusion, the monolithic LDGC crowns utilized in this case provided a simple yet very effective esthetic result. The fact that they were each milled out of a CAD-ACM e.Max block with optimum mechanical properties is assurance for their long term survival without fracture or chipping.
To read more about this article...Open access Journal of Modern Concepts in Material Science
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers
To know about Open Access Publishers





No comments:
Post a Comment