Authored by Maaroufi Ayoub*,
Abstract
The first recorded military anesthesia took place in 1847 during the Mexican American War. Despite the harsh conditions, the military anesthesiologist aims to provide a level of care comparable to that expected in civilian practice, and military practice must adhere to the guidelines and recommendations of regulatory bodies. The Moroccan medico-surgical field hospital deployed by the Royal Armed Forces (FAR) of Morocco in Anfgou aims to come to the aid of the populations of these regions facing the rigors of winter by providing the necessary care in the various specialties. Medical and paramedical staff includes nearly 10 specialties in addition to a radiology department, a laboratory for medical analyzes and a pharmacy which offers drugs free of charge. Our work aims to study the organization and functioning of the operating theater, as well as the demographic and pathological characteristics of the patients treated.
Keywords:Anesthesia; Companion hospital; Humanitarian mission; Military
Methods
Retrospective study, monocentric, spread over a period of three months and 10 days, from 11/27/2019 to 03/08/2019, in the first Moroccan medical-surgical field hospital, located in Anefgou in Morocco, for the benefit of the local population whose access to health establishments is difficult, aggravated by the harsh climate.
Result
During this period, the operating room received 235 patients (141 men and 91 women, i.e., a sex ratio M / F = 1.58, the average age was 46 +/- 16 [range: 4-85]. 88 patients (29%) were taken care of by the ophthalmologist for cataract and pterygium treatment (68 and 22 respectively), visceral pathology came second (26%) with 44 cases of hernias (inguinal, umbilical and cases of recurrence), 16 cases of gallbladder lithiasis (15 women and 1 man), 15 cases of proctological pathologies (fissures, fistulas, and anal abscesses), 2 cases of hydatid cysts and one case of appendicular peritonitis. 37 cases (16%) benefited from gestures relating to the Otorhinolaryngol sphere: cervicectomies, cyst of the thyroid gland, lipomas, warts, and cysts. 27 patients (11%) were operated on for superficial pathologies (cysts, lipomas). 2 cases (1%) of varicocele. An emergency caesarean section. A case of reduced elbow dislocation. On the anesthetic level, 20 procedures (9%) were performed under general anesthesia. 54 procedures (23%) under spinal anesthesia. 2 cases under locoregional anesthesia (1%). 87 procedures (37%) under local anesthesia combined with sedation. 66 procedures (28%) under local anesthesia. 6 procedures (3%) under sedation alone.
Discussion
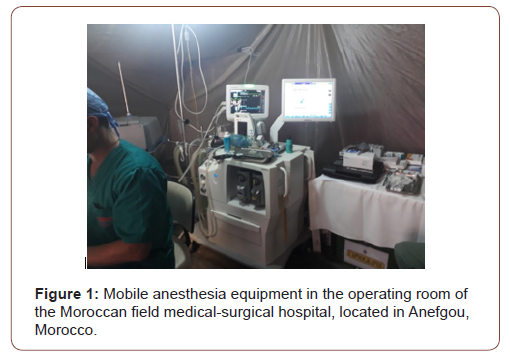
The field hospital deployed in Anefgou had 16 military doctors of different specialties, including a visceral surgeon, an anesthesiologist, an otolaryngologist, an internist, an ophthalmologist, a gynecologist, a pediatrician, and a dentist, as well as five general practitioners. The paramedical staff of this hospital unit consisted of 19 members, including six nurses, a midwife, a laboratory technician, and a pharmacy technician, with an emergency service open 24 hours a day, material, medical equipment, and drugs intended for the mission. The hospital was organized in several tents, some are shared by two specialties for the ergonomics of space. A tent was dedicated to postoperative monitoring consisting of 6 beds and containing a respirator, a scope and two nurses for monitoring. Another tent contained the operating theater, equipped with a ventilator, a scope for intraoperative monitoring, a defibrillator, anesthetic equipment, and a suction system (Figure1).
The supply of anesthetic drugs included thiopental sodium, propofol, ketamine, fentanyl, roccoronium, prostigmine, vasoactive and emergency drugs, and local anesthetics. The volatile drugs included sevoflurane and isoflurane, but not NO. Spinal anesthesia kits and equipment (syringes, extension tubing, and beveled needles) were available for spinal anesthesia. Oxygen supplementation was provided by an oxygen extractor and oxygen cylinders reserved as needed in the event of failure or insufficient oxygen flow obtained. Heating was provided by diesel generators and sterilization of the operating room was daily after the end of the operating program. Two ambulances equipped with a respirator, an oxygen cylinder (lightweight aluminum-aramid cylinder) and resuscitation equipment for possible medical evacuation. Patients seen by specialists and candidates for surgery are referred the same day for a pre-anesthetic consultation, the objective of which is above all to help the patient understand the surgical act, the preoperative medical evaluation, and the ‘optimization of overall medical and surgical care.
Following the pre-anesthetic consultation, an appointment is given to the interested party according to the order of admission and according to the urgency of the procedure to be considered. The telephone number of the person concerned or of the representative of the law of the region where the person lives is noted in the register in order to contact him later. It was essentially based on the assessment of the land; associated comorbidities; cardiovascular evaluation, in particular functional capacity and the stage of dyspnea according to the NYHA classification, while looking for the concept of angina on exertion, possibly supplemented by an ECG; the respiratory evaluation was based on the clinic (pleuropulmonary examination with possibly a chest x-ray) and finally the evaluation of the VAS. A biological assessment can be requested if necessary. The risk associated with the surgery was low and patients who were heavy due to their co-morbidities or else requiring surgery with a high risk of bleeding were referred to the nearest hospitals for more “safe” treatment.
During this period 235 gestures were performed, there was a clear male predominance with a frequency of 61% (many women did not respond to their appointment out of fear or modesty, especially if the pathology was not very disabling), the average age was 47 years with a clear predominance of the (30-60) yearolds (69%) explained by the large number of patients admitted for cataract cures and hernial pathology which were often neglected this which exposed them to morbidities not to mention the social handicap linked to the decline in visual acuity with its psychological repercussions (Figure 2,3).
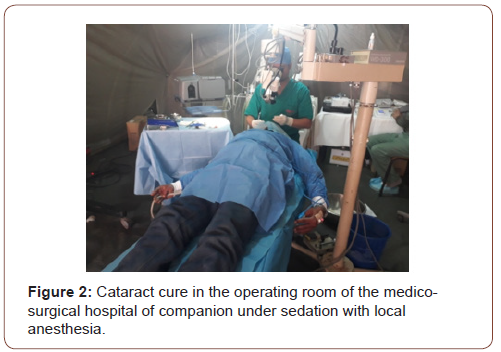

Almost all cholecystectomies for gallstones were performed in women (15 for a man) with an average age of 40 years, explained by the high incidence of lithiasis pathology in women [1]. Proctologic pathology represented an important part of the operative program dominated by fissures, fistulas, and anal abscesses (45%, 36%, 18% respectively). The pathologies encountered were most often neglected and operated on at a late stage. The current anesthetic control was sedation with local anesthesia (68% of procedures) since it was mainly cataract cures and superficial surgeries. Spinal anesthesia (23%) was preferred to general anesthesia whenever possible, thus reducing complications related to general anesthesia (9% of procedures), in particular the difficulty of managing the upper airways, the absence of a nasal fibro scope. which could be requested in the event of difficult intubation (presence of the Eschmann mandrel), and the absence of monitoring of the depth of anesthesia and of a curarometer. Intraoperative monitoring consisted of ECG leads, non-invasive blood pressure monitoring, precordial stethoscope, pulse oximetry, capnography, and monitoring of respiratory volumes and pressures. Antibiotic prophylaxis was performed according to the recommendations of the SFAR. Other factors have limited the use of a “more invasive” general anesthesia, and the practice of “heavy” surgeries, with a high risk of bleeding and requiring very careful postoperative follow-up with multimodal analgesia falling within the framework of early postoperative rehabilitation are : namely the limited reserve of O rhesus negative red blood cells and the unavailability of CT on site, thus allowing an earlier and more precise diagnosis of complications arising from surgery and / or anesthesia. The oxygen supply was provided by a mobile oxygen concentrator, bulky, limited in output and dependent on an alternating current supply.
Steel cartridges containing compressed oxygen were available to compensate for a drop in the flow rate supplied with oxygen hindering the work of the respirator which requires a minimum oxygen flow rate of 2.5 mbar, or in the event of failure of the oxygen extractor. The environmental factor was also a limiting factor: heat, cold, dust and humidity directly influence personnel, equipment, and medicines (treatment is carried out under improvised cloths). The language and the level of education represented a handicap since almost all the local population spoke only the local dialect “Tamazight” and the educational level of the great majority was low or even total illiteracy. We did without this problem by learning a few words and expressions necessary to carry out the anamnesis during the pre-anesthetic consultation, during the installation of the patient in the operating room, as well as to evaluate the awakening in the operating room, operative and post-operative analgesia.
Conclusion
The deployment of these medico-surgical hospitals aims to improve the health services provided to the populations of these remote areas and to improve their access to basic health services, especially during this period marked by a sharp drop in temperatures. The interest of our work is to take stock of the medical staff during this humanitarian mission and in particular the work of the operating room, the working conditions and the type of pathologies encountered in these mountain areas to have a better affinity during the next missions, and knowing how to overcome the limits of the current mission. After our mission, we recommend increasing this kind of humanitarian missions while waiting to have enough medical and paramedical staff and to develop the adequate infrastructure.
To read more about this article...Open access Journal of Anaesthesia & Surgery
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers
To know about Open Access Publishers





No comments:
Post a Comment