Authored by Mahmathi Karuppannan*,
Abstract
Pharmacists’ role has been diversified from dispensing medications to patient care. At present there is no collation of such information related to Malaysian pharmacists. This review explores the scope of involvement of pharmacists in pharmaceutical care (PC) services in Malaysia and the outcomes achieved. Articles published between 1990 - Feb 2017 were searched from Science Direct, MEDLINE (PubMed and Ovid), The Cochrane Library and Google Scholar. From 62 records, 17 articles met the selection criteria. Nine articles reported studies related to diabetes mellitus (DM); DM medication therapy adherence clinic, home medication review, patient education program and PC model. The most common services provided by the pharmacists were patient education or counselling and assessing patient’s medication adherence. In 9 studies which were conducted among diabetes patients, pharmacists’ intervention caused significant decrease in HbA1c, fasting blood glucose and/or lipid profile values. While medication adherence was reported to be significantly improved in 10 studies. Pharmacist’s interventions were also found to have improved patients knowledge and quality of life as reported in 5 studies. In addition 4 studies reported significant positive economic outcomes. This study revealed that Malaysian pharmacist’s involvement had positive impacts in clinical, humanistic and economic outcomes. Many studies focussed on one particular medical condition – diabetes mellitus. More studies should be conducted involving pharmacists from other settings and in different patient populations.
Pharmaceutical care; Malaysia pharmacists; Medication therapy adherence clinic (MTAC)
Background
Pharmaceutical care (PC) is defined as the responsible provision of drug therapy via collaboration of a clinical pharmacist with the patient, as well as other members of the health care team, in designing, implementing, and monitoring a therapeutic plan that will produce specific outcomes [1]. This includes identifying potential and actual drug-related problems, resolving current drugrelated problems, and preventing future drug-related problems. The roles of pharmacist in health care have expanded from product care to patient care [2]. World Health Organization (WHO) in conjunction with the International Pharmaceutical Federation (FIP) promoted an expanded role of pharmacists for the purpose of improving patient care and drug therapy outcomes [3]. Unlike decades ago, pharmacists are stepping in the front line to have direct contact with patients. The involvement of pharmacists in the health care has seen positive impacts [2]. One of the recent study indicated that the intervention of pharmacist in providing counselling to patients had positive impact on adherence towards medication and quality of life [4]. In addition, pharmacists’ intervention was found to reduce errors and improve the quality of services at health institutions [5]. In developing countries, pharmacists were identified as the predominant source of evidence-based drug information [6]. The scope of pharmacists in PC in Malaysia is quite ambiguous even though the role of pharmacists begin to change and expand from dispensing and compounding drugs to providing pharmaceutical care in the late 1990s [1]. In many cases, the possibilities of the pharmacist are not used optimally. Many studies have been done to evaluate the services or strategies pharmacists use to provide PC. To date no studies have collated all this information. The purpose of this study was to systematically review the literature on PC services provided by Malaysian pharmacists and the impact from these services.
Methods
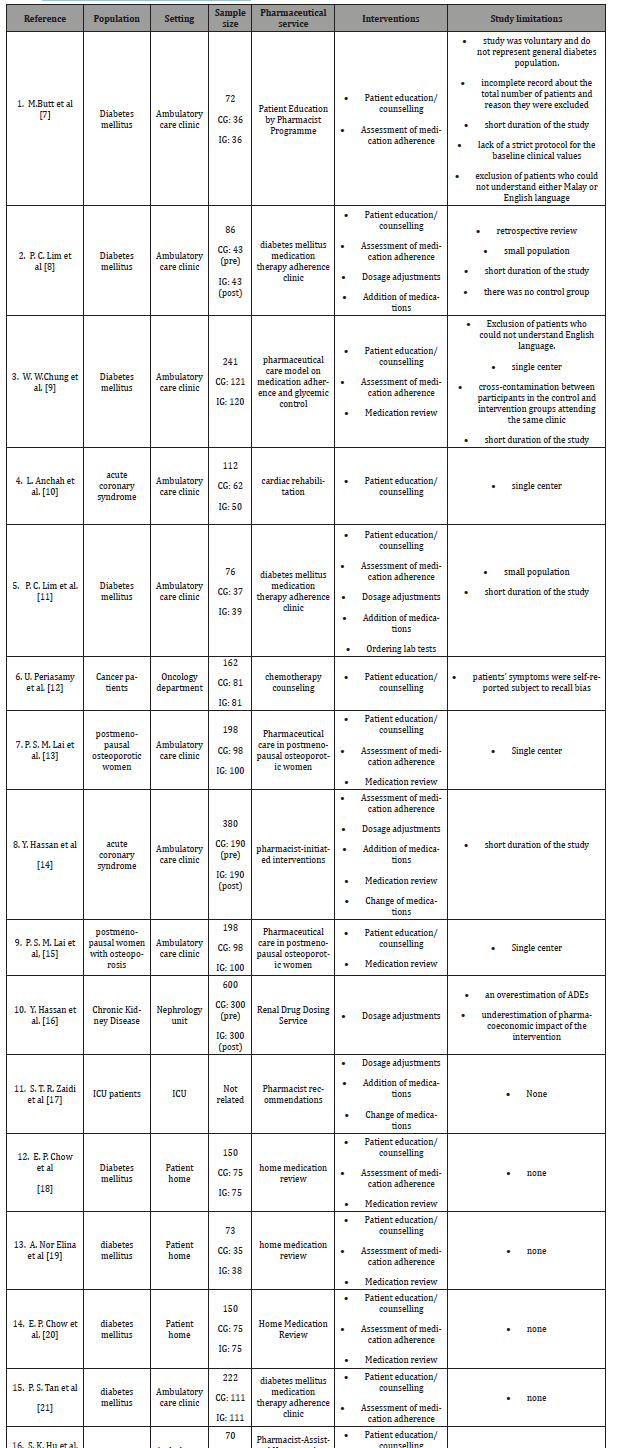
The systematic searching in Science Direct, MEDLINE (PubMed and Ovid), The Cochrane Library and Google Scholar was conducted to identify articles published in 1990 to February 28, 2017. Reviews and meta-analyses, as well as reference lists of selected articles, were searched for relevant studies. Conference proceedings were also searched. Variety of key words were used as search term such as ‘pharmacists’, ‘pharmacist roles’, ‘pharmacist responsibilities’, ‘pharmacist involvement’, ‘contribution of pharmacist’, ‘pharmacist intervention’, ‘pharmaceutical care services’, ‘pharmacist service’, ‘outcomes’, ‘benefits’ , ‘medication therapy adherence clinic (MTAC)’, ‘medical therapy management (MTM)’ and ‘Malaysia’. All the potential citations were reviewed by title and abstract and only relevant citations were retrieved. Two reviewers independently screened the title and abstract of all the articles to identify potentially relevant articles based on inclusion and exclusion criteria. If the abstract clearly showed that the study did not match our inclusion criteria, the study was excluded. If there was uncertainty about inclusion criteria, a full copy of the article was obtained. The primary author then reviewed the final selection of articles for completeness. The summary of the study included in this review are summarized in Table 1. The considered inclusion criteria for studies included in this review are as follows: (i) the studies published in English language; (ii) full-text articles or conference proceedings; (iii) study involved comparison groups: control group or pre-intervention (CG) and intervention group or post-intervention (IG); (iv) studies reported the measured outcomes (Table 1).
Table 1: Characteristics of Studies on Pharmaceutical Care.
Result
The literature search yielded 62 articles. From these 62 citations, 2 studies were removed due to duplication and 24 studies were excluded after screening the title and abstract (Figure 1). 19 studies were excluded after full text screening because they did not meet the inclusion criteria for example the intervention was conducted by non-pharmacist, the study was conducted outside Malaysia and the outcome was not reported. 17 studies met the inclusion criteria and were therefore selected for analysis. The 17 studies included in this review were published between 2003 and 2017 [7-23]. There were 11 full journal articles [7-17] among the 17. Pharmacists were found to be involved in PC services related to diabetes mellitus (DM) more commonly compared to other medical conditions. DM medication therapy adherence clinic (MTAC) [8,11,21,23], home medication review [18-20], patient education program [7] and PC model [9] involving type 2 DM patients were the most common services provided by Malaysian pharmacists. Other services provided by pharmacists involved patient population with acute coronary syndrome [10,14], cancer [12], postmenopausal osteoporosis [13,15], chronic kidney disease [16], ICU [17] and hypertension [22]. In these services, pharmacists play major role in educating patients [7-11,13,15,18- 23]; assessing their medication adherence [7-9,11,13,18-20,22,23] and conducting medication review [18-20]. In terms of practice settings, 14 studies were conducted in hospital settings [7-17,21- 23] whilst 3 were conducted in patient homes [18-20]. Sample size ranged from a minimum of 70 patients [22] to a maximum of 600 [16] and 6 studies [7, 8,11,19, 22,23] had sample sizes smaller than 100. All articles evaluated many outcomes that were classified as Clinical: HbA1c (9 studies) [7-9, 11,18-20,22,23], FBS (6 studies) [7-9,11,19,20] lipid profile (5 studies) [7,8,11,19,20], BP (2 studies) [19,22], body mass index (2 studies) [7,11], bone turnover makers (BTM) (1 study) [13]; Humanistic: medication adherence (10 studies) [7-9,11,13,18-20,22,23], quality of life (QoL) (4 studies) [7,10,15,19], patient satisfaction (2 studies) [15,20], knowledge (5 studies) [12,15,18,20,22], self-esteem (1 study) [12]; and Economic (5 studies) [16,17,20,21,23] (Figure 1).
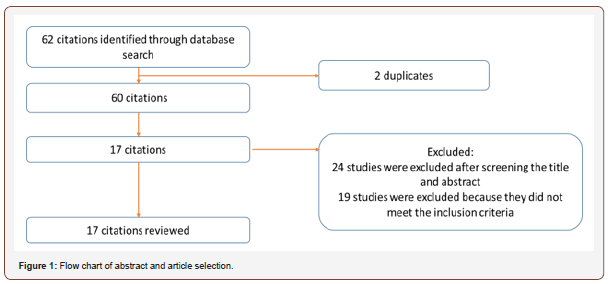
Table 2: The impact of pharmacists’ intervention.
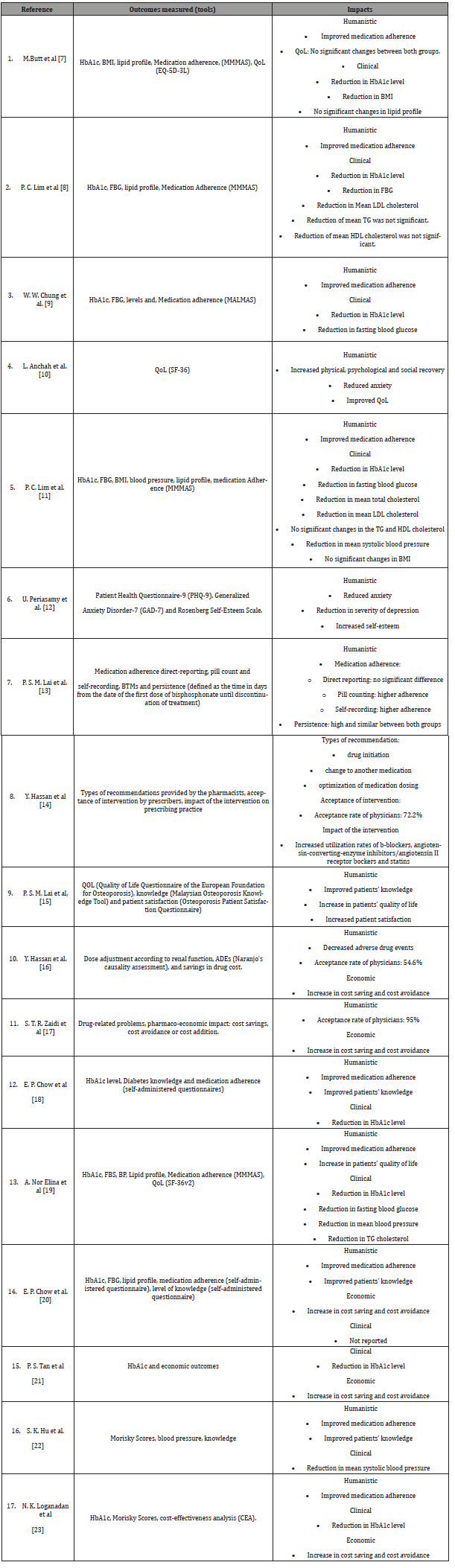
The 10 articles which evaluated medication adherence utilized the Modified Morisky Medication Adherence Score (MMMAS) [7,8,11,19], Malaysian Medication Adherence Score (MALMAS) [9], Morisky score (no mention of the tool) [22,23], self-administered questionnaire (no mention of the tool) (2) [8,20] and combination of patient direct reporting, pill counting and self-recording [13]. All studies reported improvement in the adherence except the study by Lai et al (2011) [13]. In this study when direct-reporting was used, no significant differences were found between control and intervention group. However significant differences were found when pill-counting and self-record were taken into account. Since pill counting was only able to determine if the patient took the medication within that week or month and not on a particular day, researcher applied results from self-recording for subsequent analyses. Clinical outcomes in majority of the articles were found to have decreased: HbA1c [7-9,11,18-20,22,23] and full blood glucose (FBG) [7-9,11,19,20]. More details are shown in Table 2. However the outcomes on lipid profile showed mixed results [7,8,11,19]. All humanistic outcomes showed improvement except no changes seen in QoL in a study by Butt et al (2016) [7] and economic outcomes showed increase in cost saving and cost avoidance [16,17,20,21,23]. In studies where pharmacists provided recommendation on drug treatments [14,16,17], the acceptance rate of physicians ranged between 55% and 95%. The types of recommendation given by pharmacists were drug initiations [14,17], change to another medication [14,17], and optimization of medication dosing [14,16,17] (Table 2)
Discussion
This is the first review to examine the impact of Malaysian pharmacists’ involvement in PC. Our results indicated that there are few studies on this topic, with most of them being published from 2010. The concept of PC was first introduced in 1990 [1]. Only after more than a decade did studies in Malaysia were published. Besides, MTAC was first initiated in 2004 [24,25]. The first being post-renal transplants MTAC, while DM MTAC was first introduced in 2006. The number of MTACs gradually increased and saw an escalation in 2010 (187 in 2009 versus 390 in 2010) and 2011 (561 MTACs). To date there are 839 MTACs all over Malaysia [25]. Initiation of these clinics offered opportunities for pharmacists to provide PC to patients and explains the continuous publication of articles related to MTAC after 2010.
PC in Malaysia seems to be focusing on one type of medical conditions. About half of the articles involved type 2 DM population (52%). DM is a global problem. The prevalence of DM in Malaysia is in a rising trend, from 11.6% in 2006 to 17.5% in 2015 [26] causing an alarm to all health care providers. Thus, more programs are introduced to help DM patients to manage their conditions. Yet, the prevalence of hypertension, cardiovascular diseases, decline in mental health and other conditions are also on the rise [26]. Patients from these populations should also be considered for PC as their QoL may also be affected by these diseases and further add to the health care burden. In addition to that, pharmacists should also be involved in promoting health especially in community pharmacy, which is a conducive setting for patient-pharmacist communication [27]. Most studies in this review were conducted in the ambulatory care clinics. PC are usually successful in this setting because there is better communication between health care professionals, leading to better patient outcomes [28]. Pharmacists in these settings are able to work closely with physicians and a multidisciplinary team is an effective approach. A systematic review on the effects of pharmacists’ interventions showed that pharmacists ensured continuity of care by having on-going relationships with other health care professionals and served as a ‘bridge’ between these health care professionals and the patients [29]. In addition, pharmacists provided recommendations to patients and their health care professionals to optimize therapeutic outcomes. Another review indicated that pharmacists working in partnership with other health care professionals or in a collaborative-practice model were able to contribute to improved patient outcomes [30].
One of the criteria pharmacists should have before providing PC is “to develop relationships with the patient and other healthcare providers that are needed in the provision of PC’.[1]. This may not be the case in community pharmacy settings especially in Malaysia where community pharmacists work independently and hence are underutilized. Nevertheless, efforts should be taken to increase the acceptability of pharmacists role in primary setting [31] and to initiate collaboration between community pharmacists and general practitioners. A study conducted in Malaysia showed that community pharmacists are providing some services related to PC [32] but further investigation is needed to evaluate the effectiveness of these services [33]. Despite that barriers to implementing PC in community pharmacy do exist - lack of skills, time, staff and motivation [34,35] which could hinder pharmacists from providing PC services. The involvement of pharmacists showed significant improvement in clinical, humanistic and economic outcomes. Beneficial reductions was seen in modifiable risk factors, most notably glycemic control [7-9,11,18-21,23] and blood pressure [11,19,22]. Participation of the pharmacists also had a positive impact on medication adherence [7-9,11,13,18-20,22,23] and QoL [10,15,19]. On top of that, pharmacists’ involvement produced significant cost savings and cost avoidance [16,17,20,21,23]. Similarly a comprehensive PC program (consisting of patient education and advice on medication adherence, metabolic control and life style) delivered by a clinical pharmacist over a 12-month period in United Arab Emirates revealed significantly improved glycaemic control and health-related quality of life [36]. Other studies have also reported positive outcomes with the involvement of pharmacists [4,37,38]. It is without doubt that pharmacists are essential healthcare professionals who enhance patient care and promote wellness.
Implementation of a large-scale study still appears to be lacking, despite the positive outcomes of most studies. Results on the effectiveness of health services must be based on long-term follow-up as the sustainability of an intervention on long-term needs further investigations. Most of studies had smaller sample size and recruited by the researcher. A larger study involving multidisciplinary team and blinding the recruitment process could provide a better picture of the effectiveness of PC services in Malaysia. As mentioned by Helper and Strand [1], PC involves a teamwork and a two-way communication with patients. Thus, multidisciplinary approach in PC should be encouraged. For PC to be successful in the community setting, community pharmacists should be encouraged to play their part. Although PC may be practiced in Malaysia, little is known of its effectiveness in the producing positive outcomes. It is also important to know if the community pharmacists are ready in terms of skills, staff and facilities to implement PC. These could be an area for future studies. All the studies in this review supported patients who have chronic, uncontrolled medical conditions. Newly diagnosed population, who upon diagnosis may feel confused and at denial, needs the support from health care professionals. Tackling their issues at early stage may reduce the severity of the medical conditions. PC services can be implemented in this patient population and how these services prevent further worsening of the medical conditions should be investigated.
Limitations of the Study
There are some limitations in this research. Search was limited to studies published in English and, hence, studies conducted in other languages might be overlooked. Moreover, the patient populations varied greatly between the studies and some of the studies had small sample sizes which may affect the outcomes. Selection bias may have occurred during article searching as the keywords used are more to positive words such as ‘benefit’ and ‘contribution’. In spite of these limitations, this study gives an overview of the PC activities conducted by pharmacists in Malaysia and provides suggestions for future area of research.
Conclusion
This review highlighted numerous roles of Malaysian pharmacists in pharmaceutical care and showed that pharmacist intervention resulted in various positive outcomes. Clinical, humanistic and economic outcomes were mostly seen to have improved with the involvement of pharmacists. The common site of study was hospital and more study should be encouraged in other settings especially the community pharmacy. Diabetes mellitus was the main focus in many study suggesting future studies to be enhanced in other populations.
To read more about this article...Open access Journal of Pharmacy & Pharmacology Research
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers