Authored by David A Dominguez Medina*,
Abstract
During the last two decades a new technology appeared called platelet rich plasma preparations (PRP) [1], suggesting the main benefit in both hard and soft tissue wound healing for surgical use in regenerative medicine [2], as well as aiding in decreasing: rate of postoperative infections, pain and blood loss [3]. The PRP clinical applications include periodontal surgery, Oral and Maxillofacial surgery, aesthetic plastic surgery, spinal fusion, heart by-pass surgery, treatment of soft tissue ulcers, etc. [3]. However in the recent times there have been described different types of PRP concentrates and different clinical indications for every of them. The aim of this review is to enlist and describe the different types of PRP concentrates and their current clinical use in Dentistry and Oral and Maxillofacial surgery.
Keywords: Platelet rich plasma (PRP); Plasma rich in growth factors (PRGF); Oral and maxillofacial surgery.
Introduction
There has been an evolution in the development and use of concentrates, the first ones: the fibrin glues (40 years ago) widely used in plastic surgery for skin healing that became popular in daily practice, then the platelet concentrate was first described in two publications in 1988 and 1990 (both from Knighton, et al) for the treatment of skin ulcers, and quickly its applications extended to the Oral and Maxillofacial surgery field, and with Marx and Whitman et al. publications (1998 and 1997) these concentrates were englobed with the common name of Platetet Rich Plasma (PRP) [2].
There are four families of Platelet Rich Plasma concentrates: Pure Platelet Rich Plasma (P-PRP), Leukocyte and Platelet Rich Plasma (L-PRP), Pure Platelet Rich Fibrin (P-PRF) and Leukocyte and Platelet Rich Fibrin (L-PRF) [2], there are also 2 subcategories of L-PRF: Advanced Platelet Rich Fibrin (A-PRF) and Injectable Platelet Rich Fibrin (i-PRF) [4]. There is another platelet derived concentrate: Platelet Rich in Growth Factors (PRGF), developed by Anitua, et al. (2015) by eliminating the white blood cells form PRP [5, 6].
The Physiology behind this preparation, is that PRP influences the protein expression of bone matrix during early stages of bone regeneration, the increase in bone formation occurs two weeks after its placement. The PRP preparation has to be activated with Ca2+ so that the growth factors (GF) can be released after activation [1, 3]. These PRPs GFs main role in tissue regeneration occurs by promoting osteoblasts mitosis, collagen production and cell differentiation [1, 3]. Bone regeneration is proportionally related to the concentration of platelets, this concentration has to be between 300% and 600% above the baseline to achieve optimal bone and soft tissue healing [3].
The main variables involved for a good quality PRP preparation are:
1) Blood extraction with the correct anticoagulation,
2) The PRP obtention method (directly influences the cell content of the final concentrate): the automatic methods are more reproductible compared with the manual methods; both automatic and manual methods were effective in producing a mean platelet increment of 469.75%. Studies claim that the best results in bone regeneration are obtained with mean platelet concentration of 4 times the blood baseline concentration or 400% of platelet increment,
3) The coagulation and the concentration of growth factors such as VEGF, PDGF, IGF-1 and
4) The form of application of the coagulated extracted PRP that can be applied in four formats: alone, with autologous bone, with bovine bone or with bone substitutes [1].
P-PRP and L-PRP can be used in liquid or gel form; P-PRF and L-PRF are dense fibrin materials that only exist in solid form [2]. The objective of supplementing the tissues with platelets preparations is to connect different elements of the tissue (matrix and cells) and to accelarate angiogenesis within the tissue and its remodelling [2]. PRPs induce proliferation but does not induce cell differentiation. PRFs stimulate both proliferation and differentiation of cells [2].
Description and Clinical applications of Platelet Concentrates (PCs)
PRPs applications in Oral and Maxillofacial Surgery (OMFS), Periodontal, dentoalveolar surgery and endodontics.
The introduction of PRP in OMFS has completely changed the surgical approach both large bone reconstructions in atrophic maxillas and mandibles for global rehabilitation with dental implants [3]. L-PRP and P-PRP are most tested products within the Oral and Maxillofacial surgery field, being L-PRP the most tested of both [2].
The clinical situations which these concentrates are most used are:
1. Dental extractions (such as third molar surgery) and dental avulsions where the sockets will be rehabilitated with dental implants, in this cases the application of PRP gel alone or mixed with bone substitute into the post-extraction sockets constitute an alveolar preservation technique [2, 3].
2. Another situation is in dental avulsions in patients with local pathologies that interfere with bleeding or healing [2]. 3. PRPs are also utilized when the exeresis of maxillary cysts is needed, as they amplify the natural process of coagulation after the exeresis [2].
4. Furthermore, they are used in post dental avulsion bone defects where the concentrate is mixed with bone substitute or biomaterial to fill the defect [2].
5. Both PRP gels and PRF have been described in the treatment of periapical inflamatory lesions [2, 5]. Concept of Regenerative endodontic procedures (REPs): Advanced- PRF (A-PRF), could be used in permanent teeth with closed apexes with periapical lesions, treated endodontically with the supplementation use of PRF. Although this procedure did reduce considerably the size of the periapical lesions, it is impossible to state how PRF affected the activity of the apical papilla stem cells and how these contributed to the healing of the periapical lesions 9, therefore it was not possible to assess the real effectiveness of PRF suplementation in this kind of REP [4, 7].
6. PRP could be employed to coat an avulsed tooth before its reimplantation into the post-avulsion socket [2].
7. Concept of Natural Tissue Regeneration (NTR): requires to fill the periodontal intrabony defect with L-PRF, most of the times associated with a bone substitute as a solid space maintainer, and then to cover the filled intrabony defect with L-PRF membranes to protect the grafted area and to improve the soft tissue healing above the defect. There is also Guided Tissue Regeneration (GTR) and the concept is to regenerate the ligament and all the periodontal tissues around a periodontically compromised tooth [2].
8. In gingival surgery (covering of gingival recessions and root coverage): L-PRF membranes are easily handable as if they were soft tissue grafts that can be bended and sutured. These membranes promote impregnation and cell induction phemomena [2].
9. Guided Bone Regeneration (GBR): the concept is to regenerate a bone volume through the protection of the blood clot within the bone compartment (often also filled with bone material) under a resorbable or non-resorbable membrane [2].
10. Concept of Natural Bone Regeneration (NBR): It is based in the same principle of NTR with the main difference that it only regenerates the bone (not the periodontal tissues and gingival attachment on the teeth) by amplification of natural healing independently of the clinical situation. NBR is often used in combination with metronidazole solution to avoid bacterial contamination. In NBR the regeneration of both bone and gingival compartment is synchronized. It is possible to regenerate bone and soft tissue after a failed GBR with the principles of NBR after cleaning and decontamination of the affected site [2].
11. The statins (treatment for hypercholesterolemia) such as Simvastatin promote the expression of BMP-2 (bone morphogenetic protein) which is the most potent protein with osteoinductive capacity and promotes the differentiation of stem cells to osteoblasts [1]. Studies have confirmed that the combination of PRP, PRGF and Simvastatin has a favorable effect in bone regeneration, measured in histological parameters as it maintains the osteoblastic activity in animal models with induced periodontitis [8].
PRPs in Oral and Maxillofacial Surgery: Bone grafts, Implant and Reconstructive surgery
Clinical situations:
1. Sinus lift is one of the most frequent procedures in Implantology and the most studied related to the platelet concentrates. This procedure already has a high rate of success without PRP supplementation 9. However studies show good and consistent results by combining PRP and various bone biomaterials (such as allografts, hydroxyapatita and bone mesenchymal stem cells - BMSC) [9].
2. L-PRF in combination with allograft (FDBA), accelerates the sinus lift graft healing, studies suggested a survival rate of the implant placed into the sinus lift of 100% after 5 years of a global dental rehabilitation [9].
3. The use of L-PRF as a sole filling material in the subsinus cavity with simultatneous implant placement promoted large bone regeneration around the implants, proven both hystologically and radiologically. L-PRF is no longer considered as a surgical adyuvant to a bone material, it is both a living tissue and a true solid biomaterial able to fill by itself significant volumes [9].
4. For the treatment of periimplant defects, L-PRF glue promotes more contact at the interface bone-implant and gives more strength to the periimplant bone healing compared with PRP [9].
5. L-PRPs are useful in local infections, inflammatory reactions and soft tissue dehiscences regeneration in compromised situations like the risk of tissue necrosis [9].
6. Both PRP and PRF have been used to favour the healing of complex surgical procedures such as: split-crest bone expansion for implant placement, distraction osteogenesis for atrophic mandibles and reconstruction of atrophic maxillas with block bone grafts, although this benefit probably comes more from the improved soft tissue healing that prevents dehiscences and contamination of the surgical site [9].
7. General applications in Maxillofacial surgery: PRP has been used as bone grafts supplementation in large reconstructive surgeries such as: alveolar cleft, reconstruction of bone defects after Malignant tumors resections, extended odontogenic cysts and Fibrous dysplasia [9].
8. Platelet concentrates reduce the risk of delayed healing of both bone and soft tissues in compromised patients using biphosphonates minimizing the risk of BRONJ, long-term anticoagulated patients, irradiated patients needing bone reconstruction. PRP also stimulates nerves healing such as the facial nerve [9].
9. In ENT field, L-PRF can used as filler of cavities after tumoral resection like Parotidectomy, alone or combined with fat graft [9].
10. Injectables PRPs are used for chronic articular pain treatment in sports medicine 9 and in TMJ dysfunction through closed arthrocentesis or arthroscopy.
Plasma Rich in Growth Factors (PRGF)
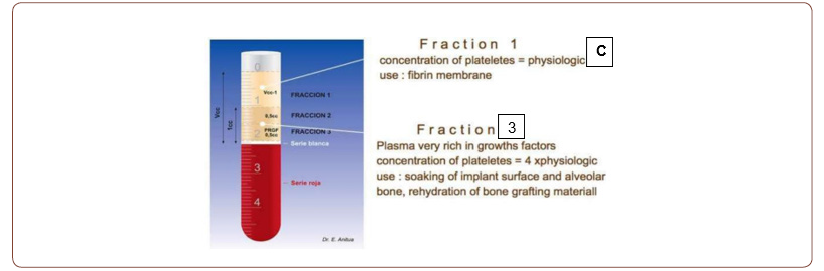
It corresponds to the Fraction 2: the fraction above the interface of the red thrombus fraction. From this preparation the red and white cells were eliminated and the platelets are concentrated 2.84 times, less concentrated compared with PRP where the platelet concentration is 8.79 times [5]. It has been studied that overconcentration of platelets reduces the positive effect of PRP preparations for tissue regeneration [5]. The PRGF preparations where the platelets are optimally concentrated, then it could have a more suitable application for tissue regeneration than PRP itself [5]. El PRGF is the first 100% autologous preparation derived from PRP. Studies coincide that PRGF promotes and accelerates the regeneration of both bone and soft tissue, because it has the potential of inducing both growth and differentiation of mesenchymal stem cells, those who accelerate the bone healing [10]. It has been the first platelet concentrate assessed in a randomized clinical study, with the objective of studying its effect in alveolar preservation, with positive results [10].
Clinical applications of PRGF
1. Reduces the marginal bone loss in periodontically compromised sockets in immediate placed implants [10].
2. Reduces the pain intensity of post extraction socket, decreasing the frequency of alveolar osteítis [10].
3. Combined with anorganic bovine bone (ABB) in sinus lift procedures, it showed that the newly formed bone area was larger than the ABB alone [10].
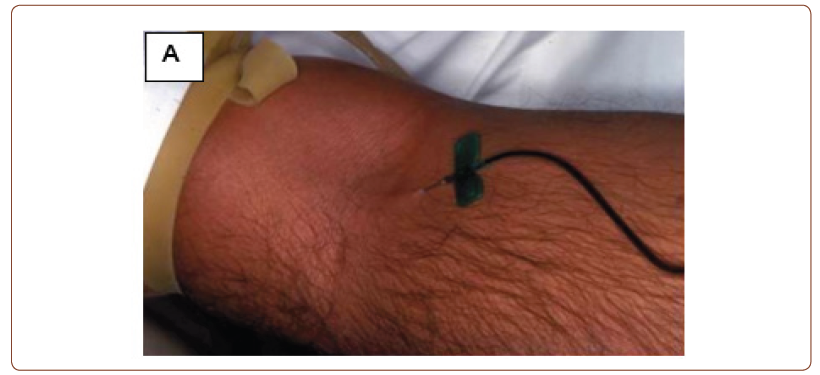
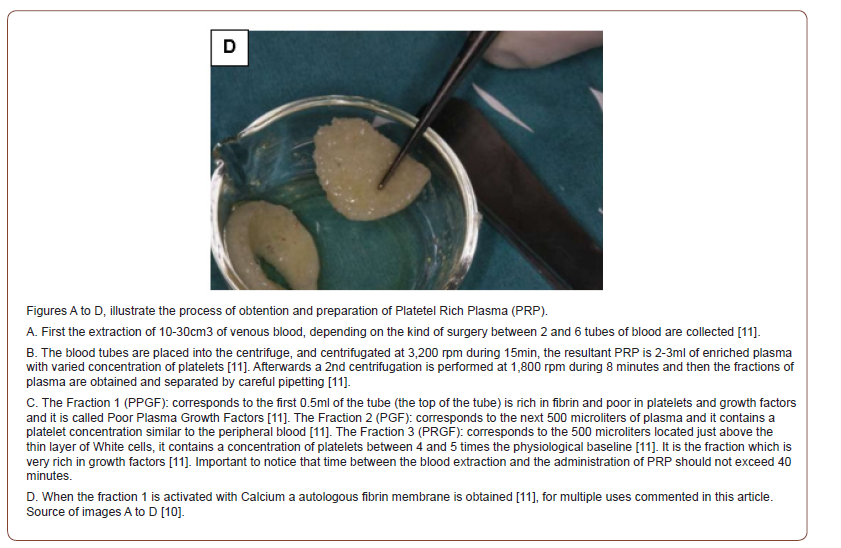
4. PRGF has been used in the treatment of Miller Class III gingival recessions with bone loss, by combining a coronal advancement flap plus PRGF and FDBA (bone graft) improving the profile of both bone and soft tissue defects [10] (Figures A-D).

Conclusion
The clinical applications of PRP preparations and PRGF nowadays go beyond the field of Oral and Maxillofacial surgery with the certainty that more applications will be found with the aid of clinical studies that support them. It is important to know the different kind of platelet preparations that have been emerging through the evolution of PRP technology development as their clinical use is based in different indications according to the concrete application field.
Discussion
There is the incorrect concept that PRP preparations promote implant Osseointegration somehow, when in reality osseointegration depends in physicochemical parameteres and their related biological mechanisms such as the chemistry and texture of the implant Surface. PRP is not used to accelerate osseointegration, in fact it has been proven that PRP can improve the early healing (not osseointegration) of titanium implants without modifications on their surface and it is a fact that PRP has no effect in the osseointegration of implants with chemically modificated surface [9].
To read more about this article...Open access Journal of Dentistry & Oral Health
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers





No comments:
Post a Comment