Authored by Sepideh Khazeni*,
Mini Review
Inflammatory bowel disease (IBD) is a chronic and progressive inflammatory condition involving the gastrointestinal (GI) tract with an increased risk for colon cancer. Two main IBD are affecting the GI tract: Crohn’s disease (CD) that the inflammatory conditions that can affect the entire GI tract, and ulcerative colitis (UC), in which the inflammatory conditions only affect colonic mucosa [1]. Since 1990, the prevalence of IBD has been stabilizing in western countries, but the incident has been globally accelerating in newly industrialized countries in Africa, Asia, and South America [3]. The exacerbation of IBD forces an excessive economic burden on the healthcare system [4] and impairs patients’ quality of life [4, 5].
The systematic reviews highlighted the role of genetic and environmental factors as the main risk factors associated with the IBD, but the leading cause of IBD has not yet been fully understood [2]. Studies showed that patients with a family history of IBD have four times the risk of developing the disease [6]. Over 200 risk loci have been identified for IBD. Many loci overlap between IBD and some autoimmune disorders, particularly with psoriasis and ankylosing spondylitis [7]. In addition, some medications, such as oral contraceptives [8] and non-steroidal anti-inflammatory drugs [9], are associated with an increased risk of IBD, while Breastfeeding appears to decrease the risk of IBD [10]. Other than genetics, dietary intake might affect the risk of GI tract inflammation in CD and UC. For example, it has been reported that western diets with a high amount of total fats, total polyunsaturated fatty acids (PUFAs), omega-6 fatty acids, and meat might increase the inflammation in the GI tract and subsequently increase the risk of CD and UC. On the contrary, diets with an abundance of vegetable intake might decrease UC risk, and those richer in fibre and fruit might reduce the risk of CD [11].
Theoretically, the Mediterranean or vegetarian diet is more beneficial for IBD prevention and management than the western diet. Because the Mediterranean and vegetarian diets provide plentiful anti-inflammatory micronutrients, essential fatty acids, and fibres [12]. Further clinical studies can demonstrate the benefit of Mediterranean or vegetarian diets in the prevention, treatment, and management of IBD. Meta-analysis showed that Mediterranean Diet might prevent the development of IBD through gut microbiota [13]. Shifts in microbial composition in IBD patients between remission and active disease might contribute to IBD flare-up [14]. It is known that an increase in Fusobacterium bacterium is associated with IBD [13]. Limited clinical studies showed that probiotics might be as effective as conventional therapies in preventing IBD relapses [12]. However, the solid preclinical data suggested that probiotics can aid patients with IBD management [15]. Further clinical studies can demonstrate the benefit of the probiotics in prevention, treatment, and management of IBD.
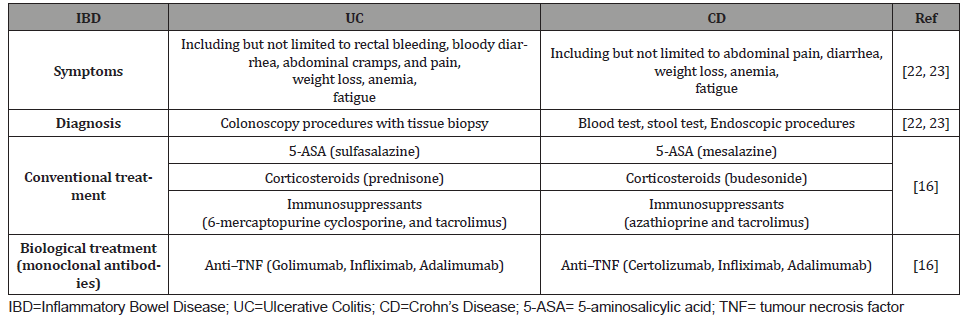
The IBDs are mainly managed with conventional therapy through groups of medications such as 5-aminosalicylic acid (5-ASA) derivatives, Corticosteroids, and immunosuppressants [16]. However, meta-analyses showed that in IBD patients, immunosuppressants such as methotrexate, azathioprine, and 6-mercaptopurine have no statistically significant advantage over placebo for induction of clinical response and remission [17]. Furthermore, meta-analyses showed superior clinical response induced by tacrolimus compared to placebo in patients suffering from UC. Tacrolimus also induced mucosal healing in UC patients [17]. The second-line therapy for IBD patients not responding to conventional treatment is biologic therapy by administrating monoclonal antibodies as anti–tumour necrosis factor [TNF], anti– integrins, and anti–cytokines [18]. The anti–TNF such as Golimumab and Certolizumab is prescribed for treatment or management of UC and CD, respectively. Moreover, other anti–TNFs such as Infliximab (IFX) and Adalimumab (ADA) are approved to manage both UC and CD. However, in severe IBDs, the increased levels of proteases, including matrix metalloproteinases (MMPs) in inflamed bowel, might fail the response to anti–TNFs [19].
(Table 1) summarised the correct IBD management. IBDs might increase the risk of developing extra-intestinal cancers. Meta-analyses demonstrated an increased risk of skin cancer by 2.2 fold and hepatobiliary malignancies by 2.3 fold in IBD patients. Furthermore, the risk of hematologic malignancies increased for CD patients by 2.4 fold and lung cancer by 1.53 fold [20]. The recent systematic review showed that in patients with IBDs, there is no risk associated with SARS-COV-2 infection. Moreover, IBD management by immunosuppressant or biologics might not affect the SARS-COV-2 infection prognosis. In contrast, IBD management by Corticosteroids might increase the risk associated with a worse prognosis of SARS-COV-2 infection [21-23].
Table 1:Summary of current IBD management.
As the current treatment and maintenance of IBD are costly for patients and the healthcare systems, herbal treatments might represent an effective complementary and alternative medicine [24]. In addition, several herbal medications might potentially be effective for the treatment of IBD as they are known to have antiinflammatory effects such as immunomodulatory properties, antimicrobial activities, antioxidant activities, and antiulcer [25]. Clinical studies showed that using herbal medicines such as curcumin, Aloe vera and Boswellia serrata could induce clinical remission or improvement in patients with mild or moderate IBD as effective as conventional therapy [26]. However, randomized controlled trials of herbal therapy for IBD treatment remain limited and heterogeneous [27]. Therefore, we suggest further clinical studies to better demonstrate the benefit of herbal medicines in the prevention, treatment, and management of IBD.
To read more about this article...Open access Journal of Gastroenterology & Hepatology
Please follow the URL to access more information about this article





No comments:
Post a Comment