Authored by Sue Ann S Lee*,
Abstract
This study explored the feasibility of telepractice intervention for treating prepositions using animated illustrations. Since telepractice service delivery models have become more popular during the pandemic, the benefit of various therapeutic materials needs to be evaluated. While animated illustration has been used in diverse educational areas, its benefits have not been investigated within telepractice service delivery models for speechlanguage intervention. Four 6-year-old English-speaking children who had difficulty in using prepositions participated in this study. Two children were diagnosed with developmental language disorders whereas the other two children were diagnosed with hearing loss. All children received a 30-minute language therapy session via telepractice twice a week for six weeks. Intervention materials were made either using animated or static illustrations. Two children (one from each diagnosis) received language therapy using animated pictures; the other two children received the same language therapy using static images. All children improved their use of prepositions during the post-tests compared to their pre-tests. Qualitative analysis indicated that the children who received language therapy using animated illustration performed similarly to children who learned with static images. The current study was conducted with only four children. Future studies should replicate the current study with a larger number of participants to evaluate the effect of animated illustrations in treating prepositions for children with language disorders.
Keywords: Telepractice; Intervention; Preposition; Animation; Hearing impairment; Developmental language disorder
Introduction
While traditional speech-language pathology services have been provided in-person or in a face-to-face fashion, telepractice, the use of internet-based services to assess, treat, or consult at a distance with patients who have communication disorders [1], has been implemented as an alternative mode of service delivery in the speech-language pathology and audiology professions. Telepractice service delivery models have unavoidably become more necessary due to the short- and long-term quarantining requirements of those impacted by the coronavirus (COVID-19) global pandemic. A rapid expansion of telepractice in communication disorders practice has been observed across varied settings in the U.S., including schools, hospitals, and outpatient clinics.
Previous telepractice research in preschool- and schoolaged children
In recent years, the volume of telepractice studies examining preschool- and school-aged children with various communication disorders and developmental disabilities has increased [2-4]. However, a relatively small volume of telepractice experimental research has investigated treatment efficacy in preschool- and school-aged children with speech and language disorders. In recent systematic reviews of telepractice for preschool and school-aged children with speech and language disorders [5, 6], only 10 non-duplicated experimental studies were included. This volume is smaller than those examining adult populations. For example, Weidner and Lowman [7] found 26 experimental studies on adult speech and language intervention via telepractice between 2014 and 2019. Furthermore, systematic reviews by Molini-Avejonas, et al. [8] and McCarthy, et al. [9] indicated that telepractice for individuals with hearing loss has focused on audiology services to identify the presence of hearing loss or parent- or family-centered early intervention. Only a few studies have been conducted to examine the effectiveness of telepractice for treating language skills in preschool or school-aged children with hearing loss [10, 11].
The existing telepractice research has examined treatment progress in language intervention via telepractice across a broad level of language behaviors rather than evaluating change in a specific target skill in children. For instance, Gabel, et al. [12] reported that 33.3% and 40% of 71 children with speech and language disorders improved one or multiple levels in telepractice intervention, respectively. The children’s progress was measured by the change in four functional communication measures (FCM) including speech sound production, spoken language production, spoken language comprehension, and intelligibility. The authors also compared children’s progress with National Outcomes Measurement System (NOMS), reporting that the percent of improvement was similar to that of the NOMS data set (28.2% and 34.1%). When progress was evaluated in terms of FCM, it was difficult to identify whether all language behaviors on each FCM or a specific language behavior would be improved in the children.
Furthermore, some researchers [10, 13] compared outcomes using a standardized assessment (e.g., the Preschool Language Scale-4, PLS or Revised Preschooler Language Assessment, RPLA) in children who received language therapy via telepractice or in-person therapy. These standardized tests are designed to measure overall language abilities, such as expressive or receptive language skills. Similar to the FCM, when standard scores of the participating children were compared between telepractice and face-to-face intervention, it is difficult to determine if the changes were due to overall improvements or specific target behavior. Although these previous studies suggest that service delivery via telepractice is equally as effective as face-to-face language intervention, it is not certain whether the telepractice service delivery model is effective for specific language domains such as morphology, syntax, or semantics. Therefore, more studies are warranted to examine treatment effects of telepractice for children with language disorders, targeting specific language behavior across various language domains.
Prepositions in children with language disorders
Language is composed of content and function words. As function words, the development of preposition use is vital in language acquisition because it helps children develop a configuration of temporal and spatial systems of a language by identifying the time of the event or location of objects relative to referent time and objects [14, 15]. For example, it is necessary to identify the topological distinction between interior and exterior subspace in preposition acquisitions like in or on. It is also essential to understand the movement of an object toward or away from a reference location (across or through) to develop an early spatial system [15]. The initial spatial system is relatively simple in child language; however, it becomes more complicated when a second object (between) and deictic relation (front/back) are applied [15]. Inappropriate use of prepositions may prevent a child’s further academic or occupational development as prepositions are critical in mathematics [16] and daily activities (e.g., understanding directions), respectively.
Most studies examining prepositions in English-speaking children were conducted decades ago. Brown [17] documented development of prepositions in and on as among the first grammatical morphemes in young children. Other prepositions such as up and down are often observed in young children’s first words and early word combinations [18]. A longitudinal study [19] from the CHILDES archives reported that six typically developing children aged ranged from one year ten months (1:10) to 4:2 demonstrated the correct use of locative prepositions as early as 18-26 months of age. The authors examined the emergence of 13 simple and complex locative prepositions. Simple prepositions included in, on, into, onto, out of, off, and of whereas complex prepositions included across, along, around, through, front, back, and between. These prepositions were fully acquired from 31 to 57 months of age in the six children.
It is well documented that children with language disorders demonstrate difficulty acquiring grammatical morphemes, including prepositions [20]. Watkins and Rice [18] examined three prepositions such as in, on, and over in preschool-aged children with language disorders and found that the age-matched children with typical development performed better in the use of prepositions than the language-impaired group. Grela, et al. [21] showed a similar result in their study where locative and dative prepositions were examined in ten children with language disorders. Preposition use is also significantly delayed in hearing-impaired populations. Several studies [22, 23] have reported that children with hearing loss tend to omit prepositions regardless of the mode of communication, although some researchers did not report a delay [24].
Methods for teaching prepositions often utilize motion and spatial activities because the acquisition of these concepts can be facilitated by motion and dynamic interaction between the child and the teachers. For example, when a teacher teaches a child the preposition across, she/he may use a small animal (horse) and a small bridge to show “a horse goes across the bridge.” In telepractice intervention, a similar method could be used in that the speech-language pathologist (SLP) ask the child to follow what they demonstrate through the monitor. On the other hand, the SLP may play videos showing the relative spatial concept or subscribe to commercially available websites that provide instruction materials specially designed for treating various language concepts to young children. It is not certain, however, the degree to which instructional methods or materials affect a child’s ability to learn preposition concepts in telepractice intervention. Furthermore, some students utilities of the telepractice platform, may rely on sharing the traditional static materials on the computer screen. Such static pictures may not show a clear spatial concept to the child because the child may not know what a certain preposition refers to. Coufal and colleagues [25] noted common suspicion on the effectiveness of the telepractice service delivery model might exist due to limited visual and tactile cueing compared to face-to-face speech intervention. Thus, it is essential to examine the benefits of instructional materials to prepare increasing use of the telepractice service delivery model for children with language disorders.
Use of animated illustration
An animation is a form of dynamic representation that can be used to make complex processes understandable to the learner. Research studies report that learning in computer-based animation environments enhances understanding of complex concepts and systems compared to traditional learning environments where information is mainly delivered verbally [26]. Animation can facilitate learning across various instructional fields [27]. Despite the usefulness of animation, contradictory findings exist on the effectiveness of animation-based learning as compared with learning based on static pictures. In reviewing the literature, Tversky, et al. [27] argued that animation-based learning has no significant advantage over static pictures. In contrast, Hoeffler and Leutner [28] claimed that dynamic animations greatly impact successful learning.
A recent body of empirical studies still demonstrated contradicting findings. Rosen [29] tested 5th and 7th-grade students and found an animation-based online learning environment had a significant impact on the transfer of knowledge and on learning motivation. He also found that students perceived themselves as playing a more central role in classroom interactions and felt more interested in learning. Smeets and Bus [30] found that 5-year-old children gained in vocabulary size after reading interactive animated e-books, followed by static e-books. However, Schlosser, et al. [31, 32] tested 3- to 5-year-old typically developing children to ascertain whether they showed better naming and identification of verbs and spatial prepositions when animated or static graphic representations were presented. They targeted 24 verbs and eight spatial prepositions and found that animated symbols were more beneficial than static symbols for verbs but not for prepositions. Schlosser et al.’s studies [31, 32] suggest that animation may not be effective on prepositions; however, further studies should verify this finding due to the limitations of these available studies.
Research using animation has been conducted with various academic subjects in education for typically developing children (e.g., math, science, or language arts). Although animation or 3D materials have been used in a medical and nursing distance learning program [33, 34], only a few research studies have been conducted using animation to address intervention goals for children with language disorders.
Purpose of the study
The purpose of this pilot study was to explore the benefits of the animation-based language intervention via telepractice as compared to static pictures on improving preposition use for children with developmental language disorders and children with hearing loss. This small-scale study was designed to initially understand the effect of animated and static therapeutic materials on treating prepositions. The findings of the current study may allow for more extensive clinical trials to address the effectiveness of animated stimuli in language intervention and to examine possible pre-post intervention changes in outcomes. The current study asked three questions as follows:
1. Do children with developmental language disorders and children with hearing loss improve their preposition productions during post-tests compared to pre-tests using telepractice intervention?
2. Do children with developmental language disorders and children with hearing loss show higher accuracy of preposition productions with animated illustration than static images?
3. Do children with developmental language disorders and children with hearing loss show similar improvement of preposition productions?
Materials and Methods
Participants
The study was approved by the Institutional Review Board of Texas Tech University Health Sciences Center for studies involving humans. Four 6-year-old monolingual English-speaking children participated in the study. The two children were diagnosed with developmental language disorders without any concomitant disorders such as hearing, visual, cognitive, and socio-emotional impairment. The other two children were diagnosed with a mild to severe hearing loss. Except for hearing impairment, these two children did not have other concomitant disorders such as visual, cognitive, and socio-emotional impairment.
The etiology of the children with hearing loss was unknown. One child was diagnosed with bilateral profound sensorineural hearing loss, and utilized bilateral hearing aids from age 2:0 until she was implanted at age 5. The other child with hearing loss was diagnosed with mild to moderate sensorineural hearing loss and had been fitted with bilateral hearing aids since age 3:2. All children received speech-language therapy since they were enrolled at schools (Table 1).
Table 1:Participant Profile & Group.
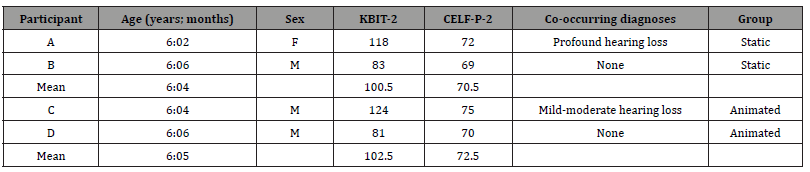
The participants completed two standardized assessment batteries. The Kaufman Brief Intelligence Test-2 (KBIT-2; Kaufman & Kaufman, 2004), and Clinical Evaluation of Language Fundamentals- Preschool-2 (CELF-P-2, Semel et al., 2004) were performed to test non-verbal IQ, and core language skills, respectively. The standard score of KBIT-2 in all children was within 1.5 standard deviations. For the CELF-P-2, all children were 1.5 standard deviations below the mean for their chronological ages, establishing the presence of language disorders.
The two children with developmental language disorders were randomly assigned to one of the two groups (static vs. animated). The other two children with hearing loss were also randomly assigned to one of the two groups. The mean age was 6:4 for the static group, and the mean age was 6:5 for the animation group. Table 1 shows the participant profile, the standard scores of KBIT-2 and CELF-P-2, and group assignment.
The study design
The current study is best described as a case study design. Each child underwent a pre-intervention assessment to establish a baseline (Baseline Phase). After the 6-week intervention was completed, there was a post-intervention assessment within a week (Post-intervention Phase). There are several benefits of the case study design. The case study design can be conducted at various points in the research process in the form of pilot studies to develop ideas for more extensive research in the future [35]. The case study design is also beneficial to capture the reality of therapy outcomes in real-life settings [36].
Baseline and probes
Baseline measures were obtained using probes and a language sample in a face-to-face method. Commercially available picture cards [37] where each preposition is illustrated using a dog figure were used to elicit 12 English prepositions such as in, on, over, under, in front of, behind, above, below, between, through, around, and across. For example, for a picture portraying the preposition behind, a dog is behind a girl. Three different pictures were chosen per preposition. A total of 36 pictures (3 pictures * 12 prepositions) were used to elicit 36 preposition productions.
The sentence completion tasks are commonly used to test grammatical morphemes in both standardized (e.g., CELF-P) and non-standardized language tests [38]. The 36 pictures portraying the 12 prepositions were randomly presented, and the children were asked to complete the pictures in a way that obligates the preposition of interest. For instance, when a researcher showed a picture showing a dog jumping over a fence, she asked the child, “What is the dog doing?” and said, “He is jumping _____.” The child was expected to complete the sentence by saying “over the fence or “over.” No modeling or feedback was given during the probe test. All responses were recorded using a Marantz PMD 671 professional 24bit digital audio recorder.
Technology for telepractice and intervention materials
Interventions were provided using a commercially available videoconferencing platform (i.e., Cisco WebEx) at a university research lab. The children received intervention using the videoconferencing platform Cisco WebEx at their homes. Each child’s mother was sitting next to the child during therapy to help the child log in to the computer and focus on the intervention sessions. Internet connectivity speeds for the participants and clinicians were tested to ensure adequate connectivity. A minimum 1.5Mbps was maintained during intervention. Instructional materials were shown on the screen using the share screen function. Annotation functions were used to maintain dynamic interaction between the clinician and client. The children were asked to respond using the computer mouse. For example, children were asked to circle on the shared material when the clinician asked, “circle the picture showing below”. The annotation function allowed clinicians and clients to choose various shapes and colors. If needed, mothers assisted the child in responding using the annotation function.
For each proposition, five different illustrations were developed using Microsoft PowerPoint software (version 2010). For example, for treating through, the following pictures were used: a tiger jumping through a hoop, a man walking through a door, a train running through a cave, an airplane flying through a cloud, a man swimming through a tube. The same illustrations were repeated once during the intervention. These illustrations were made using either static or animated pictures. More specific information on how Power- Point animations were developed is available on various video tutorials (e.g., https://www.youtube.com/watch?v=kw_udjD2xwo). All images used in the intervention materials were adopted from the internet. The same intervention slides were used for all children.
Intervention
Each child received an individualized 30-minute therapy session via telepractice twice a week for six weeks. Treatment was provided by two speech-language pathology students supervised by the author. Based on the probe tests, ten prepositions were targeted. First, four prepositions (over, under, in front of, behind) were treated during week 1 to week 3 (three sessions for over and under, and three sessions for in front of and behind). Then, two prepositions (above and below) were targeted during week 4. Two prepositions (between and through) were targeted during week 5. Finally, the remaining two prepositions (across and around) were targeted during weeks 6. During weeks 1 through 4, two opposite concepts such as over and under, in front of and behind, and above and below were treated together as pairs because using pairs of words that directly contrast each other is a common strategy for teaching opposites. The rest of the prepositions (between, through, across, around) were practiced individually.
Modeling/imitation, sentence completion, asking questions, and expansion strategies that are frequently utilized in SLP language intervention were employed. After greetings and a connectivity check, the clinician asked the child to repeat what she had said. Then, the clinician asked the child to complete the sentences. The clinician also asked questions like “Where is the book?” If the child could not answer the target preposition, phonemic cues or modeling were provided. If the child could produce the target preposition only, the clinician expanded what the child said to make it a more complex sentence.
Post-Intervention phase
After the intervention phase was completed, probes were collected using the same 36 pictures. In order to examine generalization effects, a 10 to 15-minute spontaneous language sample was collected using two wordless books, including “Frog, where are you?” [39], and “Frog goes to Dinner” [40]. The child was asked to describe what was happening in the story. To facilitate each child’s production, modeling and cues were provided when necessary; however, only spontaneous productions counted. The assessment sessions were videotaped for later viewing for reliability checks using a Sony HDR-CX405.
Scoring and Reliability
The standardized tests and probes during pre-test and posttest sessions were administered and scored by the student clinicians and the author. The probes were coded as correct or incorrect. The percentage of proposition production accuracy was obtained by dividing the number of correct prepositions by the total number of prepositions. To establish interrater reliability of the probes, another speech pathology student, who was blind to study goals, independently assessed probes and language samples. The interrater reliability for the baseline probes was 88%, and for the post-test probes was 92%. The reliability for the language sample was 95%.
Results
Baseline Phase
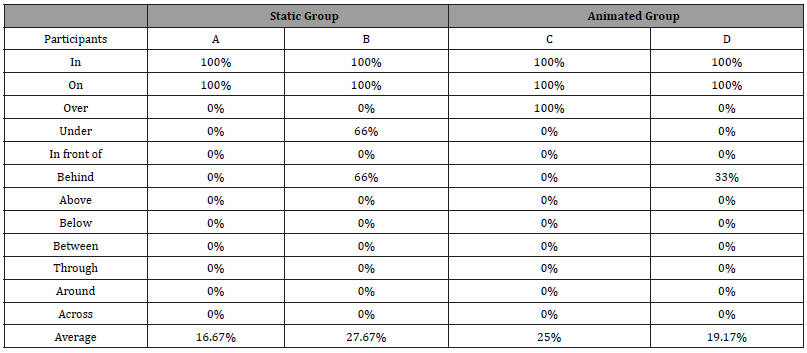
Table 2 shows the child’s production accuracy of each preposition during the baseline phase. The four children showed similar use of prepositions. All children were able to produce the prepositions in and on with 100% accuracy. For the other prepositions, child B produced under and behind with 66% accuracy, whereas child C produced over with 100% accuracy. Child D also made behind with 33% accuracy. However, none of the children produced in front of, above, below, between, through, around, and across during the baseline phase (Table 2).
Table 2:Children’s production accuracy of each preposition during the baseline phase.
Post Intervention Phase
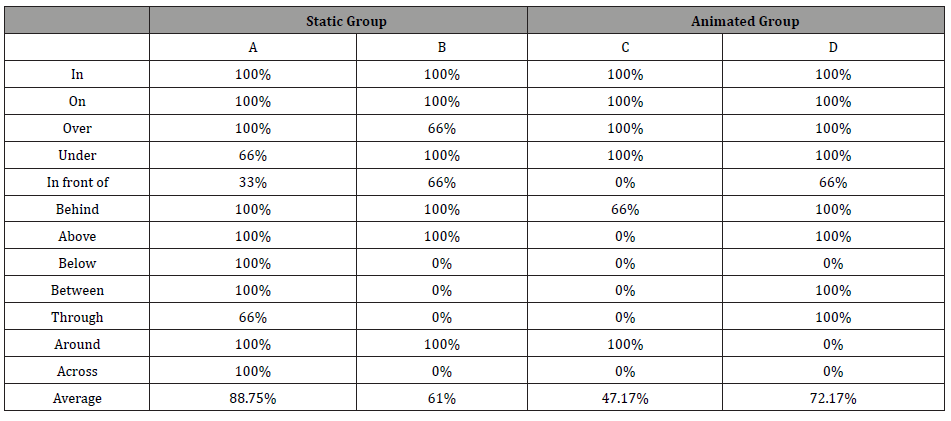
Table 3 shows the production accuracy of each preposition in the four children during the Post-intervention phase. In the static image group, child A produced most prepositions with 100% accuracy, except for under, in front of, and through. She correctly produced in front of only one out of three times. The other two prepositions were correctly produced in 2 out of 3 opportunities. In the same group, child B also produced eight prepositions at least twice correctly. However, below, between, through, and across were not produced at all. In the animated image group, child C was able to produce five prepositions (in, on, over, under, and around) with 100% accuracy, while he produced behind with 66% accuracy. Among 12 prepositions, six prepositions were not produced at all. Finally, child D produced the majority of prepositions with over 66% accuracy. Only three prepositions such as below, around, and across were not produced at all (Table 3).
Table 3:Children’s production accuracy of each preposition during the post-intervention phase.
The language samples showed that children spontaneously produced some prepositions; however, they were limited to in and on. Although Child A performed better than the other children during post-test, she only spontaneously produced in once and on three times. The other children made in 7 to 9 times and on 3 to 4 times. For the target prepositions, in the static image group, Child A made under, over, and behind once. Child B made behind four times, in front twice and over once. In the animation picture group, child C made under once and over three times and child D made over and between three times each.
Discussion
The purpose of this pilot study was to explore whether animated illustration enhances a child’s acquisition of English prepositions in language intervention via telepractice. It was hypothesized that animated illustration would be more beneficial than static images for children to learn about complex spatial concepts. Below, each research question of the current study is addressed.
Do children with developmental language disorders and children with hearing loss improve their preposition productions during post-tests compared to pre-tests in telepractice intervention?
The current study found that all children, regardless of their group identity, improved their usage of prepositions over a sixweek intervention with a total of 6 hours of treatment. Our findings were consistent with previous telepractice studies, claiming that telepractice is a viable service delivery model for children with language disorders [6, 12]. The biggest improvement was found in child A in the static group. She had a 72% overall increase, followed by child D (53%) in the animation group. The other two children in each group showed a similar improvement (33%) as compared to the baseline phase.
Previous studies of telepractice often compared telepractice outcomes to the national NOMS data report [12, 25]. According to NOMS 2012-2016 [41], 39% of pre-kindergarten children with language disorders showed progress in the spoken language production with an average of 12 hours of intervention; however, almost 30% of the children did not show any progress within 8 hours of intervention. Compared to the NOMS, the current study demonstrated that language intervention via telepractice might be an effective way to deliver language intervention to young children with language disorders. Given that limited research examining the efficacy of the telepractice service delivery model for language intervention for young children with language disorders, the current study also supports the feasibility of telepractice to treat prepositions for young children with language disorders.
Do children with developmental language disorders and children with hearing loss show higher accuracy of preposition productions with animated illustration than static images?
The effect of animated illustrations has been contradictory. Some researchers [28-30] claim that animation significantly impacts successful learning in children, whereas others [31, 32] found no significant effect of animated materials on children’s preposition acquisition. The result of the current study was consistent with Schlosser and colleagues in that the clear benefit of animation illustration was not evident in language intervention via telepractice. The children who received language therapy using static pictures showed similar production accuracy to those who received therapy using animated illustrations.
The similar improvement between the two groups may be due to the small sample size in the current study. In addition, two possible factors could be addressed. One factor might be the use of dynamic interaction in both animated and static groups during telepractice intervention. For example, the current study utilized various annotation functions regardless of the group to keep the children fully engaged in the therapy. The children in both groups were asked to participate in the therapy by drawing a circle to an swer which picture shows either over or under or coloring objects. Thus, even children in the static group were actively involved in dynamic interactions during telepractice. Another factor might be the degree and quality of animation developed by the PowerPoint software. In our animated materials, only one feature is typically animated while the other features are static. Also, the animated feature was static until the clinician entered a key to make the feature animated. For example, in a picture where a dog jumps over the fence, the dog was static at first. Then, a dog jumped over the fence when the clinician entered a key. Thus, the degree of animation may not be substantial for children in a learning phase of development. Furthermore, the animated jumping movement in our intervention materials may not look realistic and natural to children. The quality of animation may not greatly impact learning in young children. The quality of animated materials in virtual therapy has been considered a factor affecting the effectiveness of virtual speech-language intervention for individuals with communication disorders [42]. The finding of the current study suggested that the type of media use or materials may not be the primary factor affecting the effectiveness of language intervention.
Do children with developmental language disorders and children with hearing loss show similar improvement of preposition productions?
As mentioned earlier, it was assumed that telepractice might not be effective for speech therapy because visual and tactile cues are limited in telepractice compared to face-to-face methods [25]. While clinical evidence of telepractice as a method of delivering early intervention services to families of infants and toddlers with hearing loss is currently available [3, 43], another assumption regarding telepractice intervention is that telepractice may not work for direct intervention with school-aged children with hearing impairment due to the reduced quality of signals. Although limited, currently available telepractice studies [10, 11, 13] have shown that a direct telepractice intervention with preschool and school-aged children has been feasible. The current study provided additional evidence on the feasibility of a direct intervention for children with hearing loss. Two children with hearing loss showed improvement during the post-test compared to the pre-test period. In particular, one child with severe-to-profound hearing loss (Child A), fitted with cochlear implants, showed the most significant improvement among the four children. However, it is important to note that this study did not intend to compare the outcomes between children with developmental language disorders and children with hearing loss. Instead, this study aimed to find whether both groups showed similar improvement during post-test as compared to pre-test. More research into the efficacy of telepractice in children with hearing loss is warranted.
Limitations and Future Directions
In addition to the small participant number and the heterogeneity of participants included in this study, the current study has limitations. First, although all children who participated showed improvement during the six-week intervention period, the intervention duration may not be sufficient for all children with language disorders to improve all target prepositions. In particular, prepositions
targeted during the second half of the intervention were treated only in two sessions. It was evident that children needed more sessions to achieve better production accuracy. Further studies should carefully consider the number of target prepositions and sufficient sessions to examine the intervention’s effectiveness in improving use of prepositions. Second, the animated stimuli used in the current study were made by a student assistant who majored in speech-language pathology. Thus, the quality of the animation may not be similar to professionally created animated illustrations. It would be interesting for further studies to investigate the effects of the type of animated illustrations on children’s learning to examine if animated illustration made by clinicians using the PowerPoint software is equally effective compared to commercially available animated videos.In conclusion, the current study was designed to investigate the benefit of animated illustrations for treating children with language disorders. This pilot study demonstrated the feasibility of preposition intervention via telepractice for children with language disorders. Future studies should replicate the current study with a larger number of participants to evaluate more strongly the effect of animated illustrations in treating prepositions for children with language disorders.
To read more about this article....Open access Journal of Otolaryngology and Rhinology
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers





No comments:
Post a Comment