Authored by Ayşe Güneş Bayir*,
Abstract
The most common cause of chronic gastritis is considered to be H. pylori infection, which also paves the way for peptic ulcers and stomach cancer. In the presence of chronic gastritis, a decrease in stomach acid levels or a complete loss of acidity occurs. In the case of decreased acidity in the stomach causes the stomach to become more open to germs. Microorganisms colonizing the stomach promote the formation of carcinogenic chemical compounds. Chronic gastritis is manifested by some clinical symptoms such as abdominal pain, heartburn, burning sensation, nausea, vomiting, and diarrhea. The primary treatment is undoubtedly nutritional therapy together with appropriate drug therapy. Diet and lifestyle factors can help to prevent the disease as well as slowing down the course of the disease and reducing clinical symptoms. Alcohol consumption and smoking can increase the risk of disease, whereas too spicy-salty foods, bitter- sour foods and caffeine-rich drinks can improve the symptoms of the disease. Meals should be consumed with small and frequently, keeping the chewing time long. In the course of chronic gastritis, vitamin B12 and vitamin C deficiency and absorption problems can be seen quite often. In order to meet the deficiency of these vitamins, it is important to add antioxidant-rich fruits and vegetables to the meals and increase their consumption. In cases where nutritional deficiency cannot be met, it is recommended to take vitamin supplements. Absorption of vitamin B12 takes place in the ileum. Consumption of nutrients that improve intestinal flora is recommended due to absorption problems. Consumption of probiotics has a healing effect on the intestinal flora. For this reason, it is recommended to consume foods such as probiotic yogurt, milk and dairy products, kefir. As a result, adequate and balanced nutrition affects the formation and course of the disease positively. This review focuses on the nexus between adequate nutritional interventions and chronic gastritis and particularly, how adequate and balanced diet can support during treatment of the disease.
Keywords: Nutrition; Gastritis; Helicobacter pylori; Stomach
Introduction
Gastritis is a digestive system disease that usually occurs as a result of inflammation of the aster epithelial layer [1]. According to the progression of the disease and its pathological features, gastritis is divided into acute gastritis and chronic gastritis. Acute gastritis mainly characterized by drugs, corrosion reagents, food, bacterial infection, drusgs and stress factors [2]. This disease is divided into acute irritated gastritis, acute infectious gastritis, acute erosive gastritis, acute hemorrhagic gastritis. Chronic gastritis, on the other hand, is associated with many more factors due to its complex mechanism [1,2]. Adequate and balanced nutrition contributes to the treatment of the primary causes of gastritis and to its progression in a short time [3]. Disease is examined under four different headings as acute gastritis, chronic gastritis, atrophic chronic gastritis and non-atrophic chronic gastritis. The main causes of chronic gastritis disease are acute gastritis factors whose treatment is neglected or delayed [4]. Chronic gastritis is divided into two groups: atrophic chronic gastritis and non-atrophic chronic gastritis. Both types of gastritis represent phenotypes and forms of chronic gastritis. All of these diseases present with different effects and inflammatory changes [4-6].
Chronic gastritis was started to be investigated in the 20th century and the cause of the disease could to be autoimmune [4]. H. pylori infection is histologically related to gastritis and is the most common cause of chronic gastritis in the world. H. pylori is the major etiologic cause worldwide for chronic gastritis disease [6-8]. Chronic gastritis, the most insidious, dangerous and common disease of humanity, continues until the end of life [4,9]. In some countries, for example China, the prevalence of chronic gastritis in endoscopic tests is approximately 90%. In the studies conducted, a relationship could not be established between gastrointestinal symptoms and gastrointestinal symptoms, since no symptoms were observed in the diagnosis of chronic gastritis [9]. Although autoimmune markers and chemical agents also cause chronic gastritis. They are not as effective as H. pylori. These markers and agents cause mostly inactive gastritis. However, there is still insufficient information about the effects of genetic factors and autoimmune causes on the formation and progression of H. pylori-induced gastritis [4,6,10]. However, the processes of chronic gastritis caused by autoimmune causes are much faster, progressive and difficult to treat than chronic gastritis caused by H. pylori. Chronic gastritis is the underlying cause of gastric cancer and peptic ulcer diseases.
However, underestimated chronic gastritis can be the cause of many premature deaths worldwide [4]. Excessive alcohol consumption, free radicals, microorganism infections, H. pylori infection, stress and emotional problems, use of steroidal and nonsteroidal anti-inflammatory drugs, some different drugs, nutritional errors such as inadequate and unbalanced nutrition and factors that damage the gastric mucosal barrier cause chronic gastritis. It is one of the factors [1]. Permanent life-long damage, which is caused by the high destruction of the gastric mucosa by the harmful and irritating inflammation located on the surface of the stomach, causes chronic gastritis [5]. That is, chronic gastritis is an inflammatory disease of the gastric mucosa and inflammation of the epithelial lining of the gastric mucosa [1,6]. Although chronic gastritis can cause stomach discomfort and dyspepsia, indigestion, it can also lead to weight loss [1].
It is known that the treatment of chronic gastritis that has not progressed until the last stage will reach the core by removing the H. pylori bacteria from the environment and the inflammation in the gastric mucosa can return to its healthy state [4]. Especially in acute gastritis whose treatment has been neglected, malnutrition, insufficient vitamin and protein consumption, problems in the immune system, smoking and alcohol addiction, genetic inheritance and factors, rapid food consumption and the destruction of the gastric mucosa. According to the results of a study conducted by Kim, et al., which investigated the relationship between the increase in the risk of erosive gastritis and the speed of eating, the risk of erosive gastritis was found to be approximately 15% in people with a fast-eating speed of less than 5 minutes at a meal. In addition, it has been shown that the fast-eating speed is 1.7 times more than people with a low eating speed [5].
H. pylori is an effective factor causing chronic gastritis, peptic ulcer and stomach cancer, and these diseases can cause serious problems [1,4]. H. pylori is the leading cause of acute and chronic gastritis, gastric cancer, gastric ulcer and gastric mucosa-associated lymphoma [5]. However, there are also great differences between these diseases. While peptic duodenal ulcer disease is generally observed in individuals with non- atrophic H. pylori gastritis, it is known that the stomach becomes hypochlorhydria and peptic duodenal ulcer disease is less common in individuals with atrophic gastritis [4]. According to some studies, the risk of gastric cancer in the presence of H. pylori increases 4 to 6 times [11]. Gastric adenocarcinoma is divided into diffuse type and intestinal type. A small percentage of infected people develop gastric cancer, but gastric cancer is often diagnosed late. Identifying and preventing factors that may cause risk in the course of the disease is the most important premise for overcoming the disease [4,5]. Gastric and intestinal metaplasia of atrophic origin, which may pose a risk for gastric adenocarcinoma, is directly related to H. pylori and shows the importance of H. pylori in the pathogenesis and etiology of cancer. Infection of H. pylori infection is limited to the corps and Antrim. Therefore, the development of gastric adenocarcinomas of the antral corpus is thought to be due to H. Pylori infection. The origin of gastric lymphomas is usually B cells, and the relationship between H. pylori and the lymphoid tumor associated with the mucosa has been confirmed, and it has been shown that 95% of lymphoid tumors are associated with H. pylori [11]. In chronic gastritis, a decrease in stomach acid or even complete disappearance can be seen. As a result, the acid-free stomach becomes open to microbes and is colonized by a flora of microbes. These microbes, which multiply in the acid-free stomach, can form chemical compounds such as nitrosamine and acetaldehyde, which are highly carcinogenic [4]. When looking at chronic atrophic autoimmune gastritis, it is an organ-specific disease. This disease is characterized by the opposition of autoantibodies to intrinsic factor and gastric parietal cells, and in the population, chronic atrophic autoimmune gastritis is more common in older women, occurring in 2% of the general population. In advanced stages of the disease, there is a great reduction or even absence of gastric glands and gastric mucosa. More zymogenic cells and parietal cells can no longer be found in the gastric mucosa and therefore have to be replaced by intestinal metaplasia. These changes in histology may result in decreased intrinsic factor, achlorhydria, and hypergastrinemia [12].
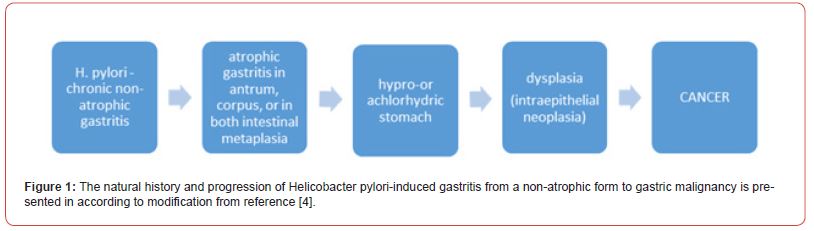
The priority for the treatment of chronic gastritis is nutrition along with medication. With adequate and balanced nutrition, the disease responds to treatment in a short time and contributes to it. Finding and solving the underlying cause of the disease, reducing the amount of acid in the stomach, that is, reducing factors such as antacids, proton pump inhibitors, H2 blockers, meeting B12 deficiency, eliminating H. pylori infection are the conditions that should be considered for treatment [3,5]. B12 are micronutrient supplements that can be helpful for folic acid supplementation and iron supplementation improvement factors [5]. As in acute gastritis, an elimination diet can be applied in the treatment of chronic gastritis [3] (Figure 1).
Atrophic Chronic Gastritis
Chronic atrophic gastritis is a chronic disease that causes complete loss of mucosal glands as an inflammatory process caused by inflammation progresses [6,13]. Loss of these glands occurs when the glands damaged due to inflammation leave their place to connective tissue or glandular structures that are not suitable for settling in that area [6]. Although these histological differentiations in the mucosal glands may be associated with H. pylori infection, they may also be due to parietal cells. These changes may also be due to an autoimmune-related reaction. Until now, there is no documented criteria worldwide to distinguish chronic atrophic gastritis caused by H. pylori from this clinical entity by analyzing autoimmune gastritis [13]. It is known that at times, chronic atrophic gastritis caused by H. pylori cannot be distinguished from gastritis of autoimmune origin. In these cases, it is possible that chronic atrophic gastritis caused by H. pylori infection will go away on its own when it reaches achlorhydric and atrophic levels with serious progression, and in this case, it is possible to mislead and confuse the pure autoimmune gastritis etiology [4]. Usually, these damaged glands take on the appearance of intestinal-type epithelial glands when transformed into glandular structures but may also take the phenotype of mücin- secreting antral glands when in the oxyntic mucosa [6]. Gastritis due to autoimmune features may progress more rapidly than atrophic gastritis due to H. pylori [4]. Histological criteria were taken into account to detect metaplastic differentiations in the antral and oxyntic mucosa, and a recommendation was made as a standard by taking all of the scales defined as visual analogies as reference. Nevertheless, biopsy is a valid diagnostic factor for mucosal chronic atrophy. At the same time, the higher the rate of spread in atrophy, the greater the need for biopsy [6]. There are two different methodological approaches that can be used to address and evaluate these situations. The first of these approaches is serological studies using marker factors of gastric functions. The second is the studies conducted by performing histological analysis of biopsy samples taken by invasive upper esophagogastroduodenoscopy method, and these studies have the gold standard among diagnostic methods. The validated and now standardized OLGA method for grading and classifying the severity of chronic atrophy regulates the disease as 5 stages and classifying it from 0 to 5. Stages of atrophy have also been associated with atrophy of the oxyntic or antral mucosa which are defined as OLGA III and OLGA IV [4,13]. In individuals more prone to autoimmune diseases, autoimmune gastritis may result in a very rapid progression of chronic gastritis due to H. pylori with atrophic markers, resulting in general and total atrophy. This may result in an acid-free stomach [4]. Although the chronic inflammation in the corpus is mild as a result of chronic atrophic gastritis, which is severe, all of the oxyntic glands have disappeared, and the stomach has become completely acid-free [5]. In the stomach, which has been exposed to ascitic and atrophic gastritis, loss of intrinsic factor occurs, and therefore, there is a decrease in the absorption of serum vitamin B12, or even a complete loss. Dietary metabolism is highly impaired in the stomach, which has suffered from acid loss, and there has been a decrease in the bioavailability and absorption of micronutrients such as iron, magnesium, calcium, zinc, folate, and some drugs [4,5]. Deficiency in vitamin B12 can cause neurological and hematological problems and disorders, as well as increase the risk of osteoporosis due to vitamin B12, vitamin D and calcium deficiency [5]. Fragmentation and destruction of parietal cells is another factor that causes a decrease in the amount of acid in the stomach in chronic atrophic gastritis. This may lead to the development of many factors such as iron deficiency anemia [13]. In the presence of an ascitic stomach and atrophic gastritis conditions, gastric cancer is a very likely disease. Chronic atrophic gastritis has a much greater effect on cancer formation than H. pylori. A chronic atrophic gastritis occurring in both the antrum and the Corpus increases the risk of developing cancer due to the destruction of the gastric mucosa [4].
In the treatment of chronic atrophic gastritis, a treatment method similar to the methods used in the treatment of chronic gastritis is followed. For treatment, first, it is necessary to eliminate the H. pylori infection and to eliminate the B12 deficiency. Stress management should be kept in the foreground in this disease where nutritional therapy is also very important in addition to drug therapy [3,5]. For pernicious anemia caused by chronic atrophic gastritis, treatment of symptoms in the early period is also an important factor in the atrophic treatment of the disease. Micronutrients diagnosed as deficient such as iron, vitamin D, and folate must be met [5].
Micronutrient Deficiencies in Atrophic Chronic Gastritis
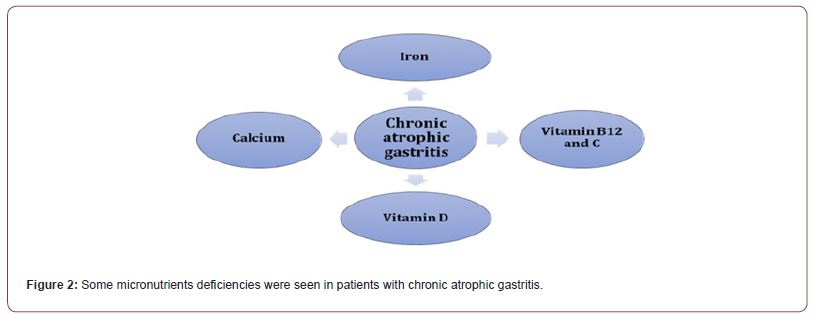
Deficiency of some micronutrients (Figure 2). was seen in patients with atrophic chronic gastritis according to malabsorption of iron, vitamins B12, C and D [12-16]. Therefore, for example a replacement of vitamin B12 are required for these patients by intramuscular cyanocobalamin at a dose of 1000 μg daily for one week, then weekly for 4 to 8 wk., and then monthly for life. On the other hand, iron malabsorption and the onset of iron deficiency anemia appear to be biologically plausible. However, patients with atrophic chronic gastritis should be evaluated for the development of concomitant iron deficiency. Vitamin C has an antioxidant and may also reduce inflammation in these patients. Long-term malabsorption can result in deficiency of calcium and vitamin D which can increase the risk of osteoporosis.
Vitamin B12 Deficiency
Vitamin B12, namely cobalamin deficiency, is frequently seen in chronic atrophic gastritis and its varieties. This vitamin is one of the most important micronutrient sources in the regulation of neurological functions, hematopoiesis factors, energy production and DNA synthesis. Vitamin B12 cannot be synthesized by the human body and is therefore taken with the food consumed or as a supplement [12-14]. Neuropathy can be seen in the results of its deficiency and malabsorption disorder, and this can cause problems in the central nervous system, although hematological differences are not observed. Mainly spinal cord involvement occurs and atrophy can be observed. Axonal loss as a result of atrophy may cause sensory ataxia, gait disturbance, spastic paraparesis, deterioration in visual functions, and changes in neural reflexes [12,13]. At the same time, cobalamin deficiency, which acts as a cofactor, when necessary, is one of the biggest causes of megaloblastic anemia. Megaloblastic anemia is found in 61% of individuals with vitamin B12 deficiency and folate deficiency [12]. Vitamin B12, that is, cobalamin, acts as a cofactor in the conversion of methylmalonic acid and converts it to succinyl coenzyme A [14]. Hydrolysis of vitamin B12 is carried out by hydrochloric acid and gastric pepsin. Cobalamin, which is then hydrolyzed, bonds with intrinsic factor, which is needed for absorption in the distal ileum and synthesized by gastric parietal cells [12]. Some of the sources of vitamin B12 are meat, some fortified cereals, fish, milk and dairy products. Absorption of vitamin B12 takes place in the ileum [14].
Iron Deficiency
Iron used in iron digestion is seen in two different forms as heme iron and non-heme iron. Heme iron is in meat hemoglobin and myoglobin and dissolves in an alkaline pH environment. At the same time, it is easily absorbed in the duodenum. Non-heme iron exists in ferric form and makes up almost 80% of dietary iron intake. However, as long as non-heme iron is not reduced to the chelated form, it cannot be absorbed, is more difficult to absorb and is less, besides, it is insoluble and begins to precipitate at pH >3 [12]. In patients with chronic atrophic gastric hypochromic anemia and iron deficiency usually precede the presence and development of megaloblastic anemia. The pathophysiology seen in iron deficiency is generally examined in foür different mechanisms. these are competition with H. pylori for required iron in the diet, inflammatory hepcidin regulation, chronic occult bleeding due to gastric micro erosions, and hypochlorhydria [13]. Secretion of hydrochloric and ascorbic acid is important for the dissolution of non- heme iron and for a normal iron absorption mechanism. Iron supplementation and treatment are of great importance in the treatment of chronic atrophic gastritis, but since patients may be quite resistant to oral iron treatment, parallel treatment of H. pylori infection is recommended in addition to iron treatment [12]. According to some studies, dietary iron intake appears to have an inverse relationship with gastric adenocarcinomas, and iron intake causes a reduction in bacteria. In addition, H. pylori uses essential iron for its own use and reduces the secretion of ascorbic acid, which prevents iron from being oxidized. H. pylori, which causes hemorrhagic gastritis, causes iron deficiency by causing blood loss [5].
Calcium Deficiency
Calcium is a very important micronutrient for bone development. Both actively and passively absorbed calcium is absorbed in the proximal small intestine as Ca2+. Absorption begins when the calcium salts in the stomach turn into calcium chloride, which dissolves easily in water. The bioavailability of dietary calcium salts varies depending on many factors, including gastric acid secretion, circulating vitamin D levels, physiologically progressive functions of the intestine and stomach, and the amount and structure of calcium taken. Stomach acidity is a very important factor as it increases the ionization and dissolution of calcium. Surgical gastric procedures such as gastrectomy cause changes such as weight loss, as well as calcium malabsorption. As a result of calcium malabsorption and long-term treatment to suppress acid in the stomach, a large increase in the risk of osteoporosis and fracture can be observed [12,14].
Vitamin C Deficiency
Vitamin C is also known as ascorbic acid. Ascorbic acid, which is used for the production of proteins such as norepinephrine, serotonin and collagen and has a great importance, is a vitamin that cannot be synthesized in the human body. Vitamin C can only be taken into the body through diet and supplementation. While the absorption of this vitamin takes place in the stomach and small intestine, this amount of absorption decreases in patients with chronic atrophic gastritis. It is thought that the reason for this is due to the in vitro effect of the high pH value in the gastric mucosa and therefore ascorbic acid degradation occurs. At the same time, Ascorbic acid, that is, vitamin C, is a serious antioxidant that cleans the stomach by converting nitrite compounds in gastric juice into nitric oxide, and its loss causes problems. It is known that vitamin C also reduces oxidative damage in the gastric mucosa by reducing the inflammation caused by H. pylori [12].
Vitamin D Deficiency
Currently, there are not many studies investigating the link between vitamin D and atrophic chronic gastritis. The main source of vitamin D is sunlight. In a 2012 researched study, a large decrease in vitamin D levels was observed in individuals with chronic atrophic gastritis disease when comparing and contrasting the general population with nonspecific gastritis. A published article showed that vitamin D deficiency seen in patients with chronic atrophic gastritis is associated with an increased prevalence of secondary hyperparathyroidism. These results reported that vitamin D or calcium metabolism may be highly impaired in individuals with atrophic chronic gastritis disease, due to intestinal malabsorption of vitamin D [12].
Nutritional Treatment in Chronic Gastritis
H. pylori is a bacterium that causes chronic gastritis and has a great effect on cancer formation. Many studies have drawn attention to the link between H. pylori, gastritis, cancer caused by gastritis, and nutritional therapy. Some foods are triggers for gastritis, while others help reduce the effects of the disease [5, 11]. For this reason, the most effective and helpful factor in the treatment of gastritis is a properly applied diet therapy. Removing the foods that will tire the stomach from the nutrition plan with the diet therapy applied reduces the effect of increased gastritis disease in the body [3]. Diet and nutrition are very important in preventing disease. At the same time, its place in the treatment cannot be ignored. Nutrition therapy is very important for strengthening the stomach wall and reducing the irritation in the stomach [5]. Cigarette consumption is thought to cause gastric cancer. According to the results obtained from the studies, it has been observed that smoking is a high risk factor for H. pylori infection. It is also known that smoking affects acid secretion [11]. Studies investigating the link between alcohol consumption and chronic gastritis contradict the results. Some studies show that alcohol consumption reduces the effect of H. pylori due to its antimicrobial effect, while others show that alcohol consumption increases the risk of gastritis. Smoking should be stopped in the treatment of gastritis [5,11]. Plenty of water should be consumed but not taken with meals, an average of 10 glasses of water should be drunk per day. In chronic gastritis patients with a high risk of dehydration, there are three different detection methods to detect dehydration: abnormal skin disorders, abnormal respiratory conditions, and increased capillary refill time [3,5,15]. Food should be chewed for a long time. In this disease, the flow of water in the stomach is slow and the long chewing factor increases the flow of gastric juice. Therefore, foods that require long chewing should be preferred [3]. There are studies showing that excessive salt consumption causes gastritis. In addition, excessive salt consumption is known to be a risk factor for gastric cancer and atrophic gastritis [11,19]. In the nutritional treatment of the disease, the consumption of foods that will cause indigestion, excessively brewed tea, alcohol, carbonated drinks, coffee, fried meals, excessive spices and sauces, sour foods such as hot peppers and pickles, sweets and pastries should be limited. Foods that will create an acidic effect should be restricted as they will cause a heartburn effect [3,5]. During this disease period, all kinds of cheese, especially curd cheese, can be consumed easily [3]. Meals should be consumed sparingly, slowly and frequently, in an orderly fashion. Eating and drinking activities should be finished at least two hours before going to sleep, especially at night. Numerous and different foods should not be consumed in a single meal. Food should not be eaten fast or hastily. Meals should not be too hot or cold, and foods with low fiber content should be preferred. At the same time, the dining environment should have a comfortable atmosphere. Failure to provide these factors may cause abdominal pain, nausea, and heartburn [3,5,9]. In chronic gastritis disease, which causes a decrease in intrinsic factor in the stomach, low serum vitamin B12 deficiency is observed. At the same time, since acid production in the stomach is reduced, the absorption of calcium and iron in the body is considerably reduced. For this reason, the course of the disease can be improved by paying attention to the consumption of foods rich in B12, iron and calcium. Vitamin B12, which is mostly taken from meat, milk and dairy products, fish and cereals, has an important place in the treatment of gastritis [3,14]. There is a decrease in the levels of ascorbic acid in the gastric juice of individuals with gastritis. This situation prepares the ground for dysplasia and gastric cancer by the oxidation of the cells in the mucosa. Based on these findings, vegetables and fruits with high vitamin C content should be added to every meal, and vitamin C supplements should be taken in cases where they cannot be consumed [3,5]. Consumption of fresh vegetables and fruits has also been shown to reduce the risk of gastric cancer formation [3]. In studies, it has been shown that vitamin C supplementation allows to reduce the incidence of gastritis disease and gastric cancer [5]. In some studies, it has been observed that consuming approximately one glass of broccoli sprouts per day helps to reduce the effect of H. pylori infection. It is also known that consumption of carrot and spinach juice is beneficial [3]. Foods containing probiotics should be added to the diet plan [11]. Probiotics are organisms that are found in foods and do not have a pathogenic effect, and their consumption has positive effects on the disease. Although the consumption of probiotics is thought to help increase the number of bacteria in the intestine, improve the intestinal microflora and the production of lactic acid. Fermented milk and dairy products, yogurt, kefir, buttermilk and yeast are examples of probiotics. Probiotics are also highly effective in the treatment of diarrhea and cancer [6, 16].
Conclusion
Adequate and balanced diet seems to have a great effect on the treatment of gastritis and its derivatives, gastroenteritis cancer and infection by H. pylori bacteria. At the same time, it is very important to close the deficiency of iron, calcium, vitamin B12 and vitamin C, to prevent anemia, and to take adequate probiotics. Cigarettes and alcohol consumption is not recommended because it causes not only gastritis but also many diseases. Foods that are spicy, salty, sour, bitter, high in acidity, rich in caffeine and difficult to digest can not only make the treatment of the disease difficult and increase the symptoms, but also cause the disease. Therefore, the intake of such foods should also be limited in patients with chronic gastritis. Thus, it can assist in making an informed decision about dietary choice, both at the individual level and in clinical settings.
To read more about this article...Open access Journal of Gastroenterology & Hepatology
Please follow the URL to access more information about this article





No comments:
Post a Comment