Authored by I Boujoual*,
Abstract
Introduction: Temporomandibular dysfunction is a benign pathology, with polymorphic expression and subject to multiple factors that participate in its etiology, which makes the diagnosis of certainty difficult. A wide range of therapeutic options are available, including splints, physical therapy, pharmacotherapy (analgesics, muscle relaxants, anxiolytics, antidepressants, etc.)
Objective: The aim of our work is to conduct a systematic review evaluating the clinical efficacy of muscle relaxants and paralyzers in the treatment of temporomandibular disorders in the light of Evidence Based Dentistry.
Methods: The collection of data from the scientific literature was carried out among the production that appeared during the period from 2000 to 2021. The literature search was carried out by exploiting databases accessible via the Internet, namely Medline through its search engine Pubmed, Elsevier, Google scholar, Research for life and Web of science. A bottom-up manual search covering the same study period was carried out in order to expand our bibliography. The writing of this systematic review followed the guidelines of PRISMA Statement (Preferred Reporting Items for Systematic Reviews and Meta-Analyses).
Results: 9 relevant articles were retained after critical reading guided by CASP-type reading grids. The articles were then classified into 3 categories according to the type of molecule administered:
-Administration of centrally acting muscle relaxants
-Administration of anxiolytics with muscle relaxant properties
-Administration of muscle paralyzer
The articles were classified in tables according to the PICO criteria (Participants/Interventions/Comparison/Outcomes). The results of our study showed a decrease in pain intensity after administration of muscle relaxants and anxiolytics with muscle relaxant properties. Botulinum toxin injection also has the advantage of being a minimally invasive procedure and an effective treatment method in patients who do not respond to the most conservative treatments.
Discussion: The results of our studies regarding the efficacy of muscle relaxants and paralytics in the management of temporomandibular disorders are supported by other systematic reviews and meta-analyses. However, new research with a longer observation period, a large sample size and a correct methodology is still needed.
Conclusion: The disparity of the results of the studies and the absence of scientific evidence that would lead to a consensus on the efficacy of muscle relaxants and paralytics in the treatment of TMD do not allow for clear-cut conclusions. In addition, the small size of the populations studied makes it impossible to extrapolate the results, which is why more in-depth studies are needed.
Keywords: Temporomandibular joint disorders, Neuromuscular agents, Cyclobenzaprine, Botulinum toxins
Introduction
The manducatory apparatus is a system formed by several elements; a passive articular component (temporomandibular and occlusal) and an active muscular component, which maintain reciprocal relations of influence between them, in coordination with the neuromuscular system [1].
These different components cannot be dissociated from each other, their harmony conditions the efficiency of the manducatory apparatus, and any alteration could disrupt the balance of the whole, manifesting in a craniomandibular dysfunction. Defined as a mechanical attack on the TMJs, of multifactorial etiology, craniomandibular dysfunction can manifest locally at the TMJs or a distance from them [2].
The most characteristic symptoms of these diseases are pain, joint noises, and dyskinesias. The latter is related to abnormal muscular activity: the masticatory muscles are the most affected and the pain can be related to damage to muscle fibers, fascia insertions, or tendons [3].
The overall treatment aims to reduce pain, improve function and act on the psyche. To achieve this, various therapeutic approaches are available, such as maxillofacial physiotherapy [4], cognitive-behavioral therapies, hypnosis [5], occlusal orthoses [6], and pharmacological therapies (muscle relaxants, analgesics, anxiolytics, NSAIDs, etc.).
Muscle relaxants act directly on the skeletal muscles due to a selective chemical action on the central nervous system. The principal molecules are Cyclobenzaprine, Tetrazepam, Thiocolchicoside and Baclofen [7].
The lack of consensus concerning the place of muscle relaxants and paralyzers in the management of disorders of the manducatory apparatus means that practitioners are confused about the use of these molecules.
The objective of this article is to evaluate, based on literature data, the clinical effectiveness of these molecules in the management of dysfunctions of the manducatory apparatus.
Materials and Methods
A literature search was performed in the international databases Medline, and Elsevier, by their search engines; respectively PubMed, and ScienceDirect. we also consulted Google Scholar.
The electronic search strategy was based on Boolean equations using MESH words related to the topic:
- “Temporomandibular joint disorder” (Mesh) And ”Neuromuscular agents” (Mesh)
- “Temporomandibular joint disorder” (Mesh) And “Cyclobenzaprine” (Mesh)
- “Temporomandibular joint disorders” (Mesh) And “Botulinum toxins” (Mesh)
Inclusion criteria
Controlled clinical trials and randomized clinical trials, conducted in humans, with identical follow-up between groups, published between 2000 and 2021 and written in French or English were included in our review.
Exclusion criteria
It was excluded from this review: Studies with publication dates before 2000, studies conducted in animals, case series, retrospective studies, literature reviews, and studies funded by manufacturers.
After searching the database, the bibliographic references of the selected articles were examined for other articles on the same topic. The scientific articles were independently checked by two authors (B.I. and F.K.), who assessed the methodological quality of all included articles using the Critical Appraisals Skills Program (CASP).
Results
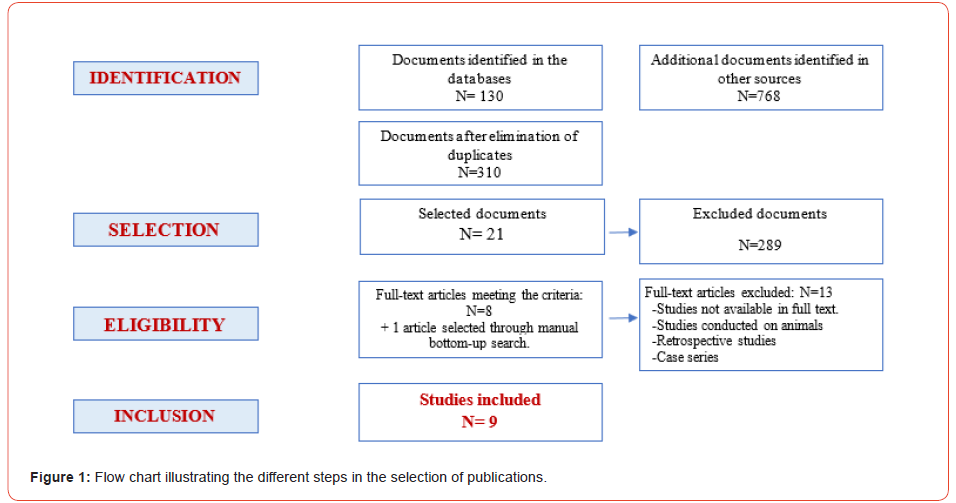
The results of our search are presented using a flow chart showing the selection of articles. A general description of the studies will be listed in a table and the articles will be classified in tables according to PICO criteria (Participants/Interventions/ Comparison/Outcomes) (Figure 1).
The studies were classified into three principal categories according to the type of molecule administered:
- Administration of centrally acting muscle relaxants
- Administration of anxiolytics with muscle relaxant properties
- Administration of muscle paralytics
The description of the articles included in our review was carried out according to the PICO criteria (Participants/ Intervention/ Comparison/ Outcomes). For each article, the variables studied and their measurement tools as well as the most significant results were summarised in the form of a table (Table 1).
Table 1:
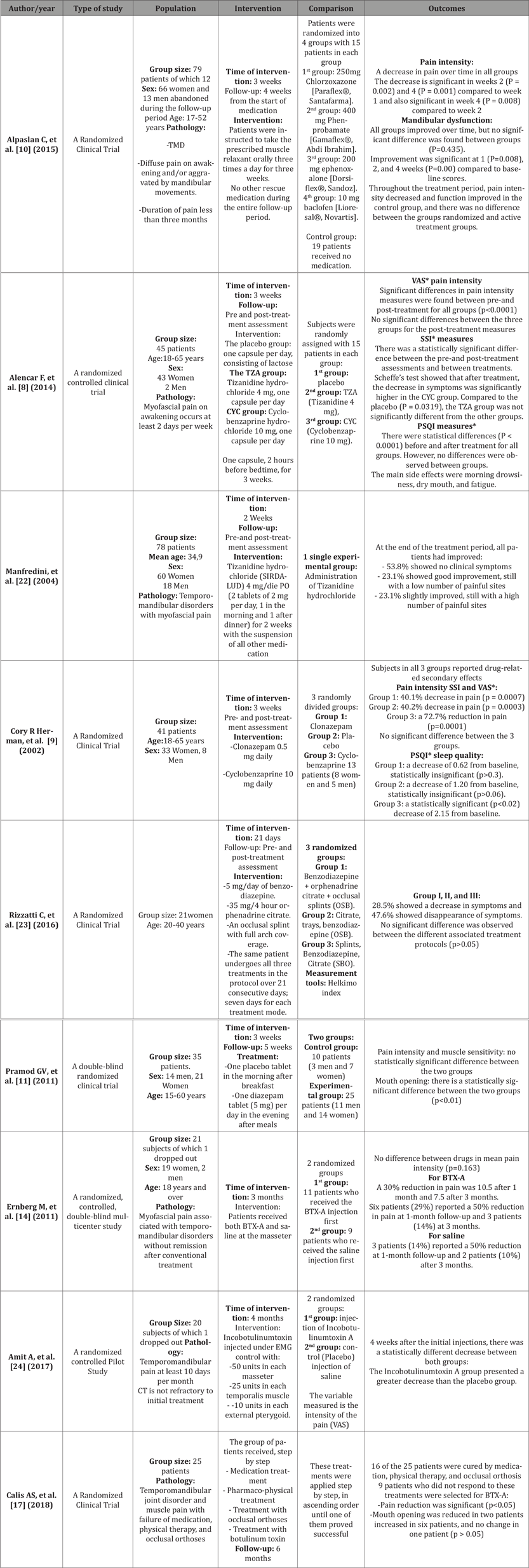
*VAS Visual Analogue Scale
*PSQI Pittsburgh Sleep Quality Index
*SSI Symptom Severity Index
Discussion
Regarding the effect of centrally acting muscle relaxants on the management of MAD
To evaluate the effect of muscle relaxants in pain management all authors used the visual analog scale to identify pain intensity.
The study by Alencar F, et al. [8] concluded that there was an eventual improvement in symptoms for all groups: Cyclobenzaprine, Tizanidine, and placebo groups, between pre-treatment and post-treatment, but no statistically significant difference could be observed between the active groups.
However, another study by Cory R Herman, et al. [9], evaluating the effect of Cyclobenzaprine on patients with waking myofascial pain, comparing it with Clonazepam and placebo, concluded that Cyclobenzaprine is more effective than the anxiolytic (Clonazepam) in the treatment of temporomandibular disorders when combined with patient education and a home self-care program for pain management.
In the trial by Alpaslan C, et al. [10], all four groups of patients who received muscle relaxants (Chlorzoxazone, Phenprobamate, Mephenoxalone, Baclofen) had pain reduction and improved mandibular function during the follow-up period. Nevertheless, in terms of symptom resolution, the final results were comparable between the groups. Muscle relaxants in the four groups for active treatment were no more effective than no active treatment. These results show that symptoms may resolve over time, even if no treatment is given in TMD.
However, the response of patients may differ in the treated and control groups. The complex biopsychosocial factors in the etiology of TMDs may lead to variable treatment outcomes. In most cases, it appears that no medication is needed as the natural course shows the resolution of symptoms.
A muscle relaxant may be prescribed for severe pain and dysfunction, while follow-up may be recommended for mild symptoms, remembering that myofascial pain symptoms tend to resolve with or without medication.
Regarding the efficacy of anxiolytics with muscle relaxant properties in the management of DAM Through the clinical trial conducted by Pramod GV, et al. [11], we concluded that the reduction in pain score was better in the diazepam group (72%) than in the placebo group (65%).
Indeed, Basmajian JV [12] compared Cyclobenzaprine with Diazepam and placebo in patients with muscle spasms in the lumbar and neck region. Clinical improvement in signs and symptoms was observed for both drugs and placebo, and there was no statistical difference between the three treatment groups.
Singer and Dionne [13] in their clinical trial of patients with chronic orofacial muscle pain found a significant decrease in pain symptoms in the groups treated with Diazepam alone and the combination of Diazepam and Ibuprofen.
As a result, the use of anxiolytics with muscle relaxant properties in the management of manducatory system disorder allows amelioration, by acting on the underlying anxiety as well as on masticatory muscle spasms.
Regarding the efficacy of botulinum toxin in the management of TMD Studies included in our research concerning muscle paralytics concluded the effectiveness of the latter in improving pain scores. However, this conclusion should be qualified since the tool used to measure pain intensity was the visual analog scale which is a subjective tool.
The study by Ernberg M, et al. [14], showed no significant difference in pain reduction between BTX-A and saline injection into the masseter muscle for patients with persistent myofascial pain associated with MAD.
Other studies by Guarda-Nardini L, et al. [15] reported a 50% reduction after BTX-A administration and 5% after saline administration, while Kurtoglu C, et al. [16] reported a 22% pain reduction for BTX-A and 13% for saline at one-month follow-up. The study by Calis AS, et al. [17] also showed that pain was reduced after BTX injection by 100%.
Finally, the study by Freund and Schwartz concluded that muscle pain in patients with TMD was reduced by 50% after BTX-A administration. It was also observed that the degree of mouth opening increased. Three processes have been recognized concerning the effectiveness of BTX-A injection [18, 19]:
Firstly, muscle relaxation: the reduction in muscle tone is explained by the inhibition of alpha and gamma neurons. Secondly, the mechanism is associated with the reduction of inflammation in the TMJ and muscle. Inflammation of the TMJs limits the movement of the capsules and ligaments. The third process is the relief of pain and the increase in the degree of mouth opening.
Botulinum toxin has the advantage of being a minimally invasive procedure and an effective treatment method in patients who do not respond to the most conservative treatments (gentle diet, non-steroidal anti-inflammatory drugs, and occlusal splints). In addition, the relatively short administration time of botulinum toxin, the low level of pain associated with its application, and the low risk of complication can all be cited as significant advantages [20, 21].
In light of the above, we can conclude that the studies do not seem to be in complete agreement on the efficacy of botulinum toxin in the management of TMD. Hence the need for further studies to judge the actual action of this substance in the treatment of patients.
Conclusion
Dysfunctions of the manducatory apparatus are complex pathologies with a multifactorial etiology and multiple manifestations that complicate their diagnosis and their management.
The diversity of study results and the lack of scientific evidence leading to a consensus make it impossible to reach clear-cut conclusions. In addition, the small size of the populations studied makes it impossible to extrapolate the results.
As a result, further studies are required, with a more extended observation period and larger sample size, to provide a better analysis of the efficacy of muscle relaxants and paralytics in the treatment of TMD.
To read more about this article...Open access Journal of Dentistry & Oral Health
Please follow the URL to access more information about this article
https://irispublishers.com/ojdoh/fulltext/clinical-effectiveness-of-muscle-relaxants-and-paralytics-in-the-treatment.ID.000630.php
To know more about our Journals...Iris Publishers
To know about Open Access Publishers





No comments:
Post a Comment