authored by Othman Rizk A Mishref*
Abstract
Keywords:Neutropenia; Bone marrow failure; Severe combined immunodeficiency
History
A previously healthy, 10-month-old male infant presented with cold symptoms and fever (temperature up to 38.5 °c) for the last 3 days, that was responding to paracetamol for few hours then recurs. It was associated with slightly decreased oral intake. He is not irritable. He is breast feeding with little smashed food. There were no significant symptoms or signs other than fever. He had been doing well until his current illness.
• The bowel pattern and urination had been normal.
• No relevant past or family history or chronic illness or hematologic disorders.
• No previous hospital admission
• No history of contact with any specific infection
• perinatal history: full term, normal vaginal delivery, smooth perinatal history.
• Nutritional history: exclusive breast feeding till age of 6 months and then started weaning with smashed food, but mainly dependent on breast feeding.
• Vaccination history: vaccinated up to date.
• Normal developmental history
• Medication history: Nil.
Examination
Vital signs are normal. Height and weight are at the 50th percentile for age. Physical examination was normal. No; oral thrush, lymphadenopathy, hepatosplenomegaly, or skin lesions are noted.
Routine investigations were done; complete blood count (CBC), C-Reactive Protein (CRP), Liver Function Tests (LFT), Renal Function Tests (RFT), all came normal except CBC showed marked neutropenia, absolute neutrophil count of 40/μL.
Clinical Course and Discussion
The patient was admitted for neutropenia workup. He was commenced on IV antibiotics (ceftazidime). He had undergone many laboratory tests without any clue to the diagnosis. These tests included a CBC, urine analysis, chest X-ray, blood culture, urine culture, stool culture, Widal test, Paul-Bunnell test, tests for brucellosis, leptospirosis, and dengue fever.
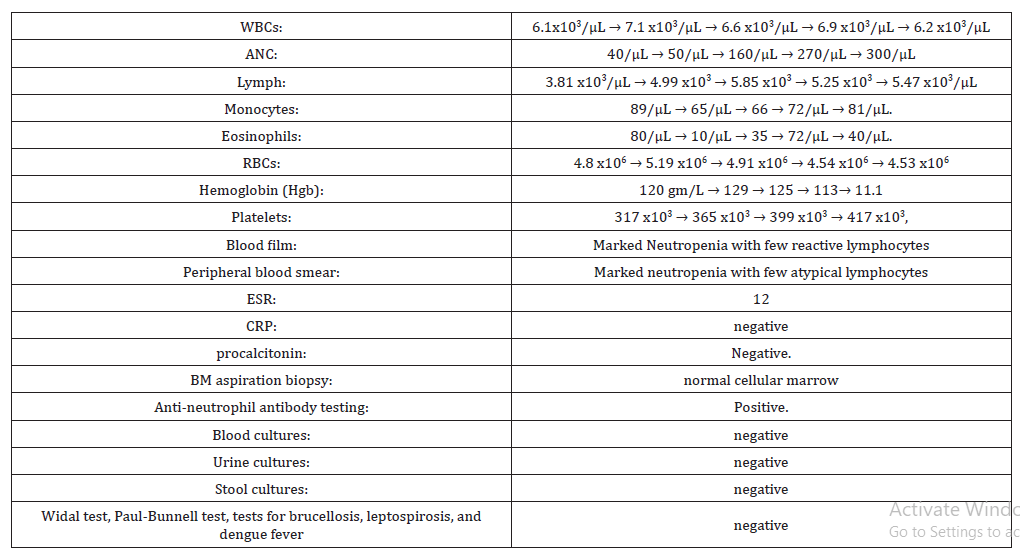
He had persistently low absolute neutrophil count (ANC) during hospital stay (Table 1):
Table 1:Laboratory results.
It is most unlikely that this infant has an acute bacterial infection, as fever has improved since admission and stayed afebrile till discharge from hospital, together with no focal site of infection or any complications, looks well, not toxic look, active and playing and feeding well. A chronic infection such as tuberculosis (TB) may present with continuous high fever, loss of weight, toxic look, night sweating as seen in disseminated/miliary TB. However, the patient received BCG vaccine and there is a BCG scar in the left shoulder. Other chronic infections without localizing symptoms include CMV, toxoplasmosis, malaria, EB virus, brucellosis are unlikely. Similarly, infiltrative disorders (malignancy/histiocytosis/sarcoidosis) are also a possibility
Of note, a CBC at birth demonstrated normal absolute neutrophil counts. There is no history of increased bacterial or fungal infections. He is the only child for the family and there is no family history of recurrent bacterial infection, neutropenia, immunodeficiency disease, autoimmune disease, or malignancy. There is no history of infant deaths in the family and CBC was done for both mother and father and was found to be normal. There has been no history of recent medication use. His growth and development had been normal until the onset of this illness.
The patient was discharged after 12 days. During his hospital stay he does well. During subsequent febrile illnesses, he does well clinically. Three months later, after he initially presented with neutropenia, his ANC improves to 1700 /μL. All investigations came normal except persistent neutropenia, positive Antineutrophil antibody, and diagnosis of chronic benign neutropenia of infancy and childhood is done.
Final Diagnosis
Chronic benign neutropenia of infancy and childhood.
Background
Neutropenia is defined as a decrease in the absolute neutrophil count (ANC) <1,500/ μL. ANC= (%bands + %mature neutrophils) X total WBC count. Neutropenia may be due to decreased neutrophil production, storage, or release; redistribution from circulating to marginated pools; or increased destruction. Neutropenia can be classified to; mild (ANC 1,000-1,500/μL), moderate (ANC 500- 1,000/μL), or severe (ANC <500/μL). ANC <200 is also termed agranulocytosis [1].
Acute neutropenia evolves over a few days because of rapid neutrophil consumption and compromised neutrophil production. Chronic neutropenia lasts longer than 3 months and arises from reduced production, increased destruction, or excessive splenic sequestration of neutrophils. The etiology of neutropenia can be classified as either an acquired, extrinsic disorders (Table 2&3) or more rarely an inherited, intrinsic defect (Table 4). Cyclic neutropenia is a rare (1-2/million) Autosomal Dominant (AD) disorder characterized by primary cyclic (every 21 days) variations in bone marrow reserve; regularly recurring fever every 21 days with oropharyngeal and skin infections. In general, common disorders are usually benign clinically and occur in children with no significant medical history of bacterial or fungal infections. Rare congenital disorders result in extremely high risks of infection and require specific laboratory tests to be diagnosed [2].
To read more about this article......Open access Journal of Pediatrics & Neonatal Care
Please follow the URL to access more information about this article
https://irispublishers.com/gjpnc/fulltext/isolated-benign-infantile-neutropenia.ID.000555.php
To know more about our Journals...Iris Publishers





No comments:
Post a Comment