Authored by Andrea Hernández-Pérez*,
Abstract
Background: Almost a third of smoking population in Mexico reported having received counseling at some point in their life.
Objective: To evaluate how knowledge and attitudes towards smoking cessation techniques is affected by the prevalence of smoking and electronic cigarette use in health professionals.
Methods: An online survey among healthcare professionals (n=632) from Federal Hospitals and National Health Institutes in Mexico City with a questionnaire evaluating tobacco and electronic cigarette consumption and attitudes towards smoking cessation.
Results: 17.4% of the evaluated healthcare professionals were current smokers, 1.5% were current users of electronic cigarette. Only 23.2% of healthcare professionals reported receiving training in smoking cessation techniques and 32.2% thought that electronic cigarette is a method for smoking cessation. Smokers considered more often than non-smokers that healthcare professionals should not give brief intervention for smoking cessation (2= 15.4 p<0.01) and reported that they do not have a major role in smoking cessation (2= 11.1 p<0.01).
Conclusion: Smoking in healthcare professionals could adversely affect the probability of giving advice for smoking cessation to their patients. A considerable percentage of HP, smokers and no smokers, consider the electronic cigarette as a valid method of smoking cessation, when scientific evidence of effectiveness or long-term safety is lacking.
Keywords:Smoking; Smoking cessation; Electronic cigarette: healthcare professionals
Abbreviations:ENCODAT 2016-2017: National Survey of Drug, Alcohol and Tobacco Consumption; WHO: World Health Organization; COPD: Chronic Obstructive Pulmonary Disease; GATS: Global Survey on Smoking in Adults; GHPSS: Global Health Professions Student Survey
Introduction
Tobacco kills 7 million people in the world each year and is one of the main causes of preventable morbidity and mortality in the world [1]. In Mexico, according to data from the National Survey of Drug, Alcohol and Tobacco Consumption (ENCODAT 2016-2017) 17.6% of people between 12 and 65-years smoke, with an average age of onset of 19.3 years and a daily consumption of 7.4 cigarettes. A large proportion of smokers (73.6%) want to quit, however, less than a third reported having received counseling at some point in their life to quit smoking. Among those who quit smoking only 3.5% used drugs or counseling [2].
Most smokers want to quit smoking, nevertheless it is a goal difficult to attain without help, due to the addictive potential of nicotine. Therefore, the World Health Organization (WHO) recommends a series of strategies to address the epidemic of smoking which are included in a plan of measures to reverse the tobacco epidemic called MPOWER, and the “O”, offer help to quit tobacco. Specifically, the section on offering help to people who smoke includes personalized brief intervention and pharmacological therapy, thus increasing the probability of successful cessation up to 3 and 7% respectively [1,3].
For smoking cessation, the participation of healthcare professionals is vital. They are often seen as role models. Even though, a significant prevalence of smoking has been reported in health professionals in Mexico, ranging from 20 to 30% [4,5]. Physicians that smoke have negative attitudes towards public politics on tobacco control and a lower probability to give brief intervention for smoking cessation [6]. The intervention they might offer for the prevention and cessation of smoking is valuable. Unfortunately, several studies have shown that some health professionals do not provide the required counseling [7,8]. This also takes place in patients with Chronic Obstructive Pulmonary Disease (COPD), since only 5% of them report that they have been given counseling at some point in their life [9].
On the other hand, health professionals face a challenge in the wake of new forms of tobacco consumption such as electronic cigarette. According to the latest surveys, their use has increased since they were launched in 2006 [10]. In Mexico, 5.9% of health professionals reported its use at least once in their lifetime; despite the ban that exists for its distribution. So, there is neither regulation, nor is there a conclusive scientific evidence on the benefit of it in smoking cessation and the risks associated with its use in Mexico [2,11].
Therefore, it is important to identify the knowledge and attitudes that health workers have regarding tobacco, electronic cigarettes and cessation, and how it is affected by tobacco smoking.
Materials and Methods
The study was approved by the Ethics Committee of the Ismael Cosio Villegas National Institute of Respiratory Diseases, with protocol number C23-17 and the participants gave a written informed consent. The procedures followed were in accordance with the ethical standards of Helsinki Declaration of 1975, as revised in 1983. It complies with the Statement: guidelines for reporting observational studies (STROBE) checklist for crosssectional- studies.
An online survey in healthcare professionals (doctors, nutritionists, dentists, social workers, researchers, nurses, psychologists and interns) from National Health Institutes and Federal Hospitals in Mexico City and the metropolitan area. The minimum sample size estimated was 376 participants, assuming a 15% prevalence of smoking with an error margin of 5%, a confidence level of 95% (z=1.96), and a refusal rate of 50%.
Measurement
The survey questionnaire was designed on Google Forms platform and distributed on the internet official pages of the institutions, advertised through their electronic newsletters, social media and e- mail of healthcare professionals with a snowball sampling strategy. All the survey were filled in anonymously.
The survey was done from May 2017 to September 2019. It consisted of a group of items from various previously standardized surveys, such as the Global Survey on Smoking in Adults (GATS 2015) [12] and the Global Health Professions Student Survey (GHPSS) [13]. Its execution had an estimated response time of 10 minutes. The survey included 8 sections: 1) sociodemographic data, 2) pattern of tobacco use and cessation, which was used to estimate the prevalence of smoking (defined as the consumption of 100 cigarettes) and current smoking (defined as the consumption of at least 1 cigarette in the past 6 months) 3) electronic cigarette, which was used to estimate the prevalence of its use 4) attitudes towards tobacco which gave information on the opinion healthcare professionals had about the attitudes they should have towards tobacco and smoking patients and 5) curriculum which asked about the knowledge obtained during their formation in relationship with tobacco.
Analysis
The data were analyzed with the statistical package R, version 3.6.1. Frequencies and percentages were used to describe categorical data, median and interquartile range for quantitative data. Chi-square was used for association between consumption and attitudes towards tobacco cessation. A p value < 0.05 was considered statistically significant with 95% confidence interval.
Results
In all, 632 (98.44%) of the initial 642 surveys from health professionals were included in this analysis. One (0.16%) was eliminated because the respondent had only completed junior high school, two (0.31%) more for inconsistencies in their responses about conventional cigarette consumption patterns, and seven (1.09%) more for inconsistencies in their responses about their electronic cigarette consumption pattern.
The median age of the participants was 34 (29-48) years, 63.3% (n = 400) were women. 28% (n = 177) had a medical specialty. Most of the participants were physicians and residents (n=382) (Table 1).
From the total individuals surveyed, 75.7% (n = 479) reported to have consumed cigarettes at some time in their lives, 27.9% (n = 176) were smokers (they have consumed at least 100 cigarettes in their live) and 17.4% (n = 102) were current smokers (they had smoked at least 1 cigarette in the past 6 months). The prevalence ofelectronic cigarette use at some point in life in health professionals was 12% (n = 76) and in current consumers, 1.5% (n = 10) and 32.2% (n = 204) reported they think that the electronic cigarette is a method to quit smoking. There was a positive association between those who have not received training on cessation techniques and those who think that electronic cigarette is a suitable method for smoking cessation. (c2= 4.01 p <0.05) (Table 2).
Table 1:General characteristics of the sample.
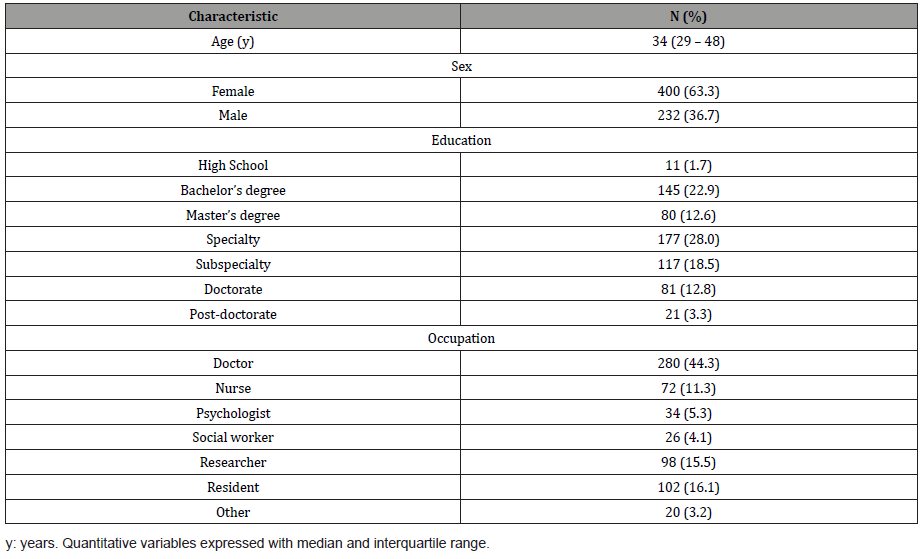
Table 2:Characteristics of smoking and use of electronic cigarettes in health professionals.
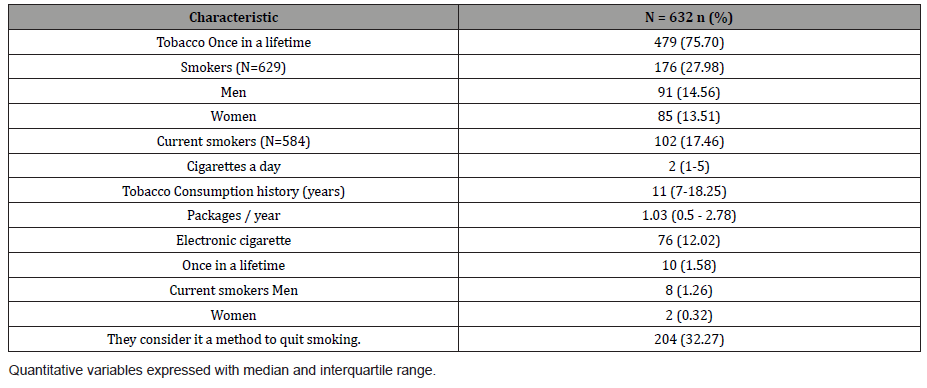
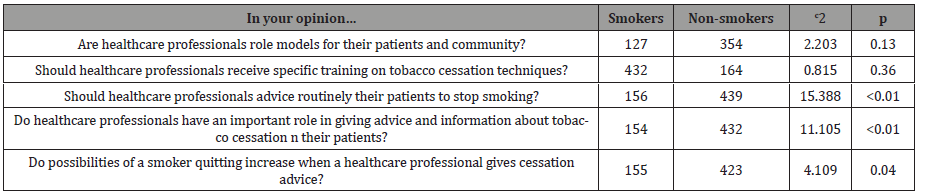
Table 3:Associations in attitudes towards smoking between smoking and non-smoking health professionals.
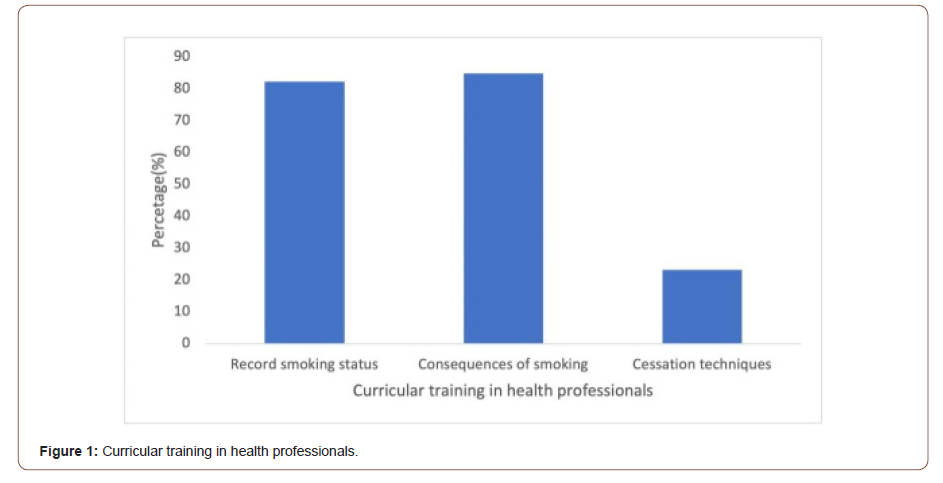
More than 80% of participants mentioned they were taught how to record smoking status in the medical history and about the risks of smoking; although only 23.2% (n = 142) of them reported having received formal training on techniques to quit smoking (Figure 1).
There is association between smoking and considering that health professionals should not routinely give brief advice to patients c2=15.388 (p <0.01). Similarly, an association was found between being a smoker and considering that health professionals do not play an important role in giving advice and information on smoking cessation c2=11.105 (p <0.01) (Table 3).
Discussion
The present study determined that smoking prevalence in healthcare professionals from Mexico City responding to the survey was similar to that reported in the national smoking survey ENCODAT 2016- 2017. The smoking prevalence in healthcare professionals has decreased compared to that reported by Sansores et al. in 1999 (28%) and by Salmerón et al., (19.2% of current smoking) in healthcare professionals in Mexican Social Security Institute in 2002 [4,14].
In our survey, men and women smoked similarly, but the prevalence in women was 8,7% higher than in the national survey, consistent with the increase in women tobacco use tendency. On the other hand, the average of daily smoked cigarettes was lower than the reported nationally (7.4 cigarettes/day) probably because hospital are smoke-free as stablished on the Tobacco Use Regulation [15].
The prevalence of current electronic cigarette use in health professionals was larger than the national (1.1%). Puzzling was the finding of a third of health professionals considering that electronic cigarette, an illegal item in Mexico, is a method for smoking cessation, and apparently dismissing the outbreak of lung injury associated to vaping reported recently [16] and the absence of demonstrated efficacy of electronic cigarette for tobacco cessation [2,17].
Mexico was the first country to ratify the WHO Framework Convention on Tobacco Control, but our General Law on Tobacco Control lacks mentioning the importance of education on tobacco issues for healthcare professionals, and it is uncommon that healthcare professionals receive training on tobacco cessation which makes more difficult helping current smokers [14].
It was also observed that being a health professional with an active smoking pattern was associated with a negative attitude towards cessation tools, a tendency to perceive cessation tools unimportant and a lower probability of offering those helpful tools to quit smoking, to patients. Duaso et al. reported that physicians with current smoking had 17% risk of not giving brief intervention on smoking patients [18].
The health professional’s population evaluated consists of professionals who in their daily consultation would face patients with multiple chronic conditions that are smoking- related. Since they work at third-level hospitals, they might find patients with cardiovascular, oncological and pulmonary diseases, among others. Therefore, it is relevant to include tobacco cessation in the curriculum of all health professionals and promote the implementation of national free cessation alternatives for healthcare professionals to improve if possible, their attitude towards smoking patients.
This study has some limitations. The sample corresponds to volunteers and are unlikely to be representative of all health workers of the institutions, although in general the prevalence of smoking was similar to that reported in the general population of Mexico, except in women. The participants may have a positive attitude towards tobacco issues. But the interest may be related to tobacco health issues in the family, or in the professional activities. The prevalence of smoking was not verified with any biochemical measure to confirm use which could produce an underestimation of prevalence on healthcare professionals. Future studies could include these indexes. Additionally, being a cross- sectional study limits the possibility to confirm any causal relationship between variables.
Conclusion
The prevalence of smoking in health professionals is significant and providing support to stop smoking will be essential in health institutions. Promoting cessation would likely increase the physician´s role model for their patients as an example of healthy practices. There is also evidence of a deficiency in smoking cessation training, and a tendency from the smoking health professionals to undermine the importance of cessation tools. In addition, the perception of a lower risk linked to the use of electronic cigarettes, expressed by health professionals, is another weakness to be worked on.
To read more about this article....Open access Journal of Addiction and Psychology
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers





No comments:
Post a Comment