Authored by Shehla Khan*,
Introduction
Squamous cell carcinoma (SCC) of the lip is the most common malignancy accounting for 25% of all oral cavity cancers [1]. The lower lip is the most commonly effected site accounting for 90 % of the reported cases with strong male predominance. Most of these cases occur due to its greater exposure to the predisposing factors [2, 3]. Since lip SCC is a transitional zone tumor between skin and the oral mucosa, it acquires characteristics of both [4]. SCC grows through the mucosal surfaces and infiltrates the deep structures in a predictable fashion. Tumors can spread by direct penetration, tracking along the nerves and vascular invasion routes [5]. The defect left by excision of such tumors presents a challenge to the operating surgeon particularly when commissures are also involved. We report such a case in which excision was performed with simultaneous reconstruction using bilateral inferiorly based extended nasolabial flaps.
Keywords: Nasolabial flap; Facial artery ligation; lower lip and chin reconstruction; Plastic and reconstructive surgery; Head and neck oncology
Case Presentation


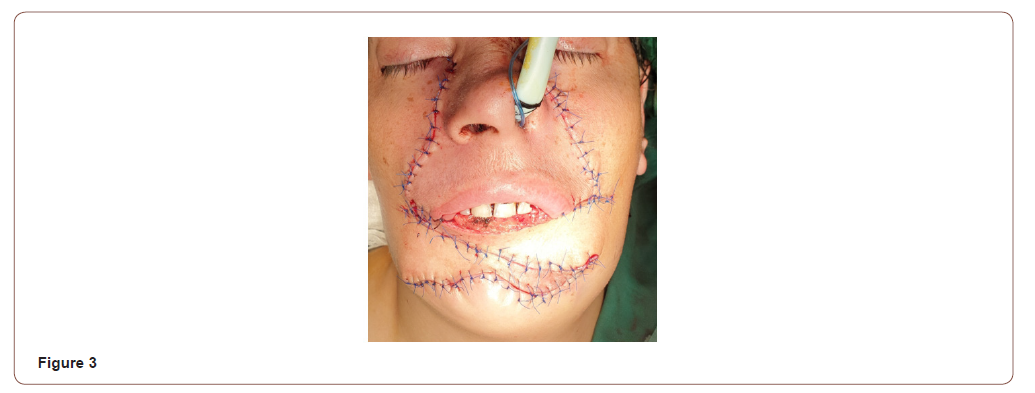
A 30-year-old woman presented with a recurrent fungating squamous cell carcinoma involving her lower lip including bilateral commissures and extending onto the chin area (Figure 1). She had continuous drooling of saliva and inability to eat food properly due to lack of competent seal of the oral aperture. Computed tomography (CT) with contrast showed the erosion of the anterior buccal cortical plate of the mandible. There was no radiologically significant disease in the neck. Patient was admitted and wide local excision was performed with 1cm margin and marginal mandibulectomy. Bilateral selective neck dissection (I-III) was also performed with preservation of facial artery. The size of the defect created after excision of the tumor was 6x8cm (Figure 2).
A bilateral inferiorly based nasolabial flap was marked on both sides 2-3mm lateral to the nasolabial fold. Facial artery was identified with Doppler ultrasonography and its course was marked. An axial pattern flap was raised just above the muscular layer to preserve the facial nerve. The inferiolateral end of the incision was extended laterally upto 2cm above the anterioinferior angle of masseter muscle. The medial incision was extended in downward direction to join the lateral border of the defect. The right nasolabial flap was used to reconstruct the resected part of the chin upto the future labio mental fold. Lingual mucosa was then sutured to the inner surface of the flap to recreate labial sulcus. Following this the left nasolabial flap was used to reconstruct the lower lip (Figure 3). Patient was kept on nasogastric feed for one week. Postoperatively there was sensation present to the light touch and pin prick in both flaps. On drinking water, pursing of lower lip was also noted.
Discussion
Defects created after tumor excision involving total lower lip and chin can be a great challenge to even the most experienced surgeon to reconstruct. A detailed assessment of the defect, including size, location, depth, extent, inclusion of the nearby subunits, and the effect on function are of paramount importance in determining the success of the reconstruction. Reconstructive goals include restoration of normal anatomy and function like oral competence and lip motion while minimizing secondary deformity and optimizing the aesthetic result. The techniques available for total lip construction include local flaps such as Bernard von Burrow-Webster and nasolabial flap [6, 7]. These flaps have the advantage of replacing like tissue with like and low morbidity. They generally produce good functional results and are aesthetically pleasing. Regional flaps like pectoralis major myocutaneous and deltopectoral flap have also been used but are bulky and nonfunctional [8, 9]. Free microvascular flaps like radial forearm and anterolateral thigh flap have been used with varying variations and success rates [10, 11].
In modern literature, nasolabial flap was first described by a German surgeon, John Friedrich Dieffenbach in 1846. Since then, this flap has been used extensively with varying success in reconstruction of orofacial defects [12, 13]. It can be raised unilaterally or bilaterally and can be designed as superiorly, inferiorly or centrally based pedicle flap. Its feeding vessel is facial artery that after originating from the external carotid passes underneath the posterior belly of digastric muscle and swirls around the submandibular gland before appearing at the anteroinferior border of the masseter muscle. It then travels upwards toward the medial canthus and terminates while anastomosing with ophthalmic branches of internal carotid artery with certain variation [14]. The flap is commonly designed lateral to the nasolabial fold with the medial limit of the flap 2-3mm lateral to this fold [15]. Traditionally, inferiorly based nasolabial flap are raised upto the oral commissure. However, for larger defects especially in cases of total lip chin defects, flap can be extended in downward direction. While generally these flaps are raised as pedicled flaps, difficulty arises when concomitant neck dissection is also planned. In such cases, random pattern flap may be harvested but it might increase the risk of partial or total necrosis particularly when bilateral facial arteries are ligated. Some authors have preserved the facial artery while performing the neck dissection, there is concern, however, that it might increase the risk of recurrence.
Varghese, et al. [16] in a large series of 224 cases performed 234 nasolabial flaps along with 63 functional neck dissections and 82 ipsilateral supraomohyoid neck dissections. 19 patients out of 212 developed either partial or total flap necrosis where facial artery was preserved. While in those cases (n=12) where facial artery was ligated, 2 developed total flap loss and 7 had partial necrosis (p=0.0000001). A significant difference indicating impact of facial artery ligation on flap survival. Overall, 23.2% (52) cases developed locoregional recurrence (p=0.03) in this series [16]. Similarly, Wijk, et al. [17] in another case series reported performing 105 flaps in 79 patients, of these 26 were bilateral. In all cases traditional modified radical neck dissection was performed. Partial flap loss was noted in 12 cases while 5 cases developed wound dehiscence. Secondary tumor or local recurrence was seen in 22% cases [17]. Singh et al, [18] in another case series reported 22 patients where nasolabial flap was harvested along with concomitant neck dissection while preserving the facial artery. In 15 cases, excision of tumor was acheived through intraoral excision while in 7 cases lip split was performed. Additionally, 7 patients received adjuvant radiotherapy. 3 patients developed wound dehiscence and one reported orocutaneous fistula while 1 suffered from local recurrence [18]. Mebed, et al. [19] in another case series of 23 patients, performed 19 nasolabial flaps and 4 facial artery musculomucosal flaps. In all cases, concomitant neck dissection was performed while ligating the facial artery. They reported 2 cases of wound dehiscence and 1 case of partial necrosis [19]. In another study by Ducic, et al. [20] nasolabial performed on 18 patients. 4 of these cases were performed along with ipsilateral radical neck dissection (facial artery ligated). No complication was noted effecting the flaps in this series [20].
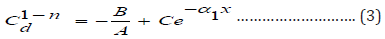
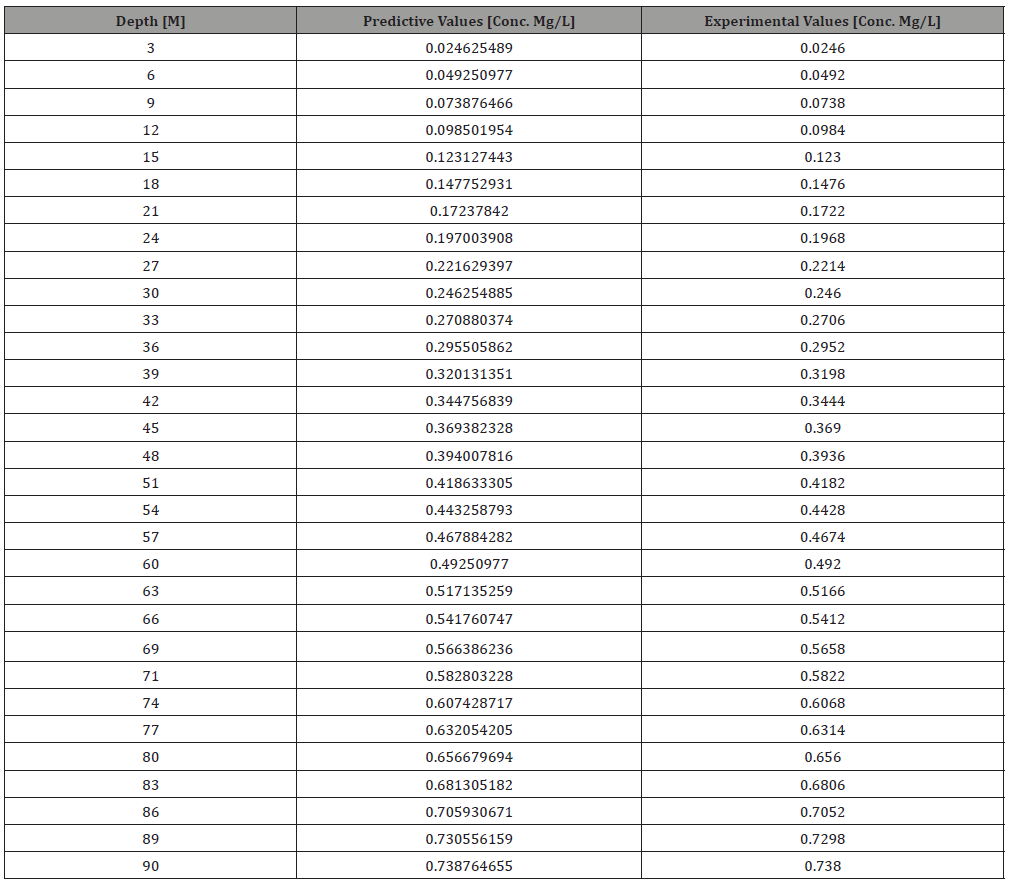
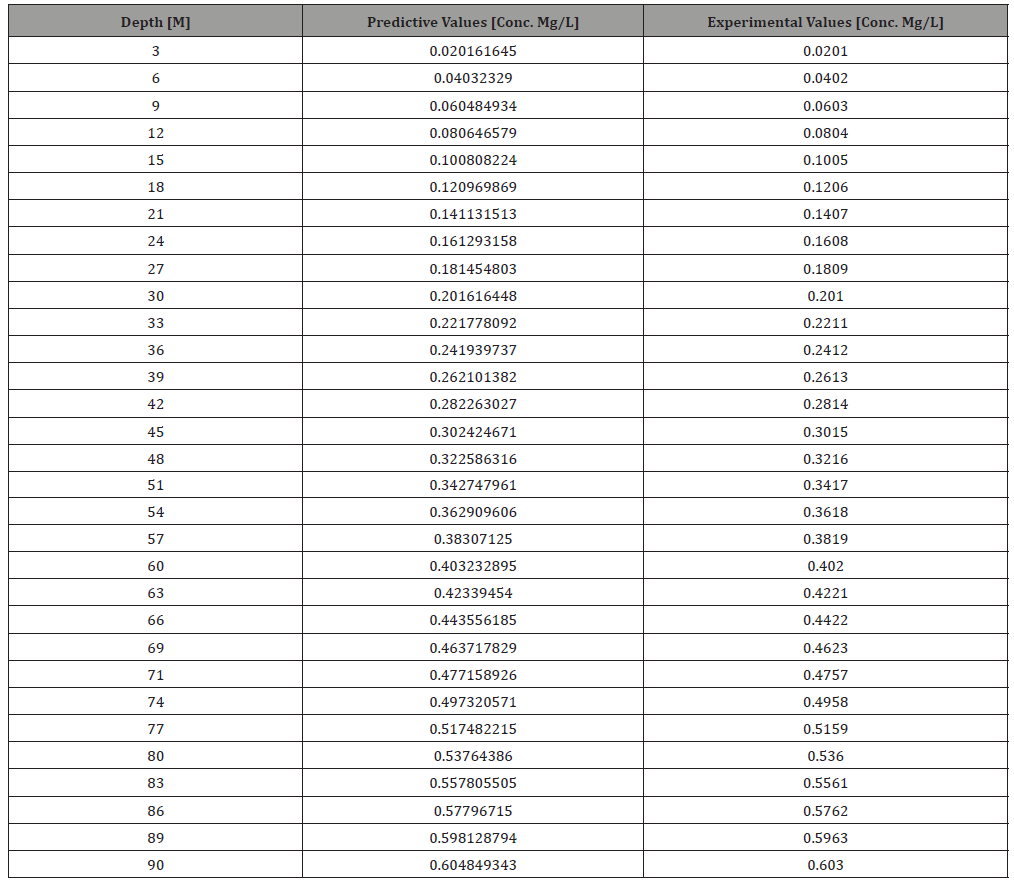
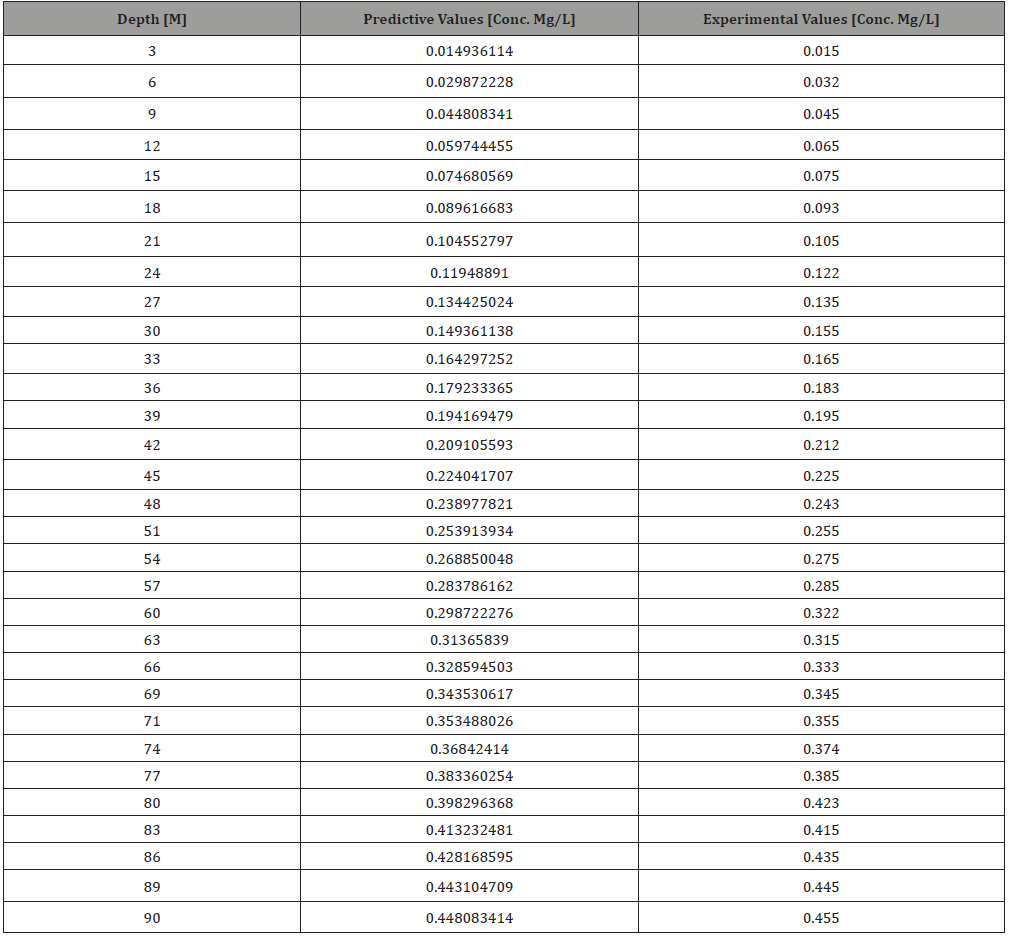
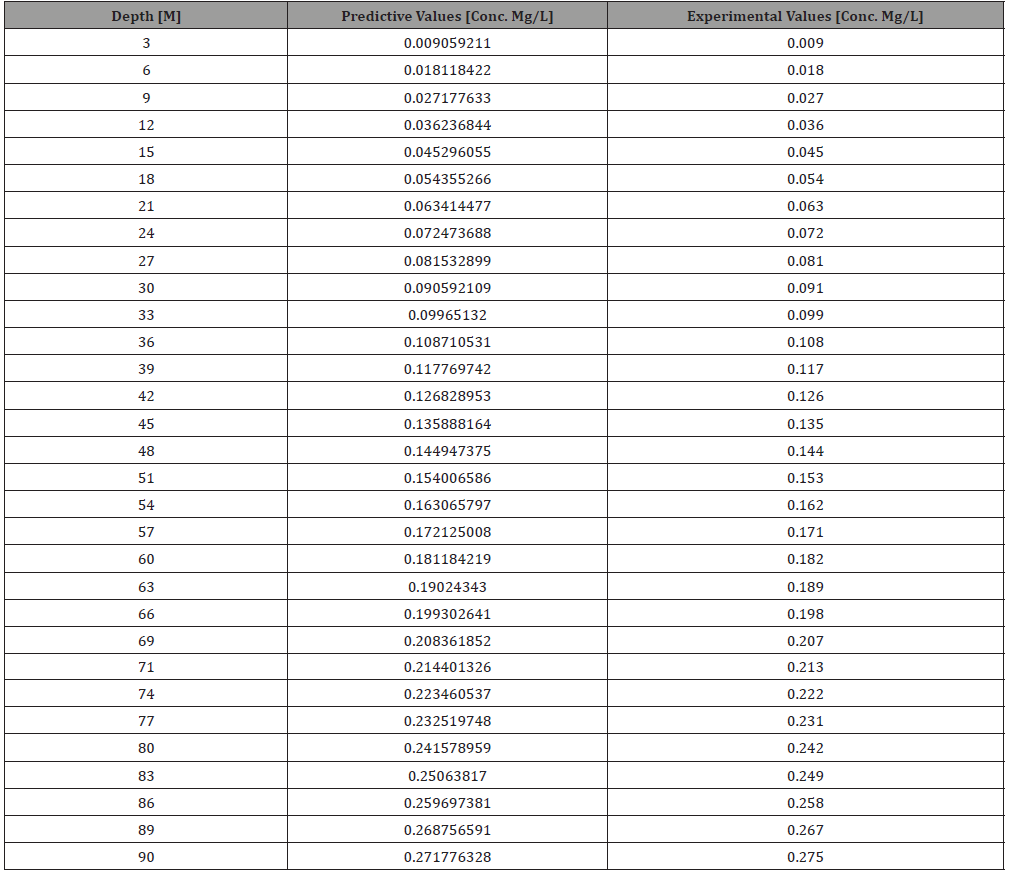
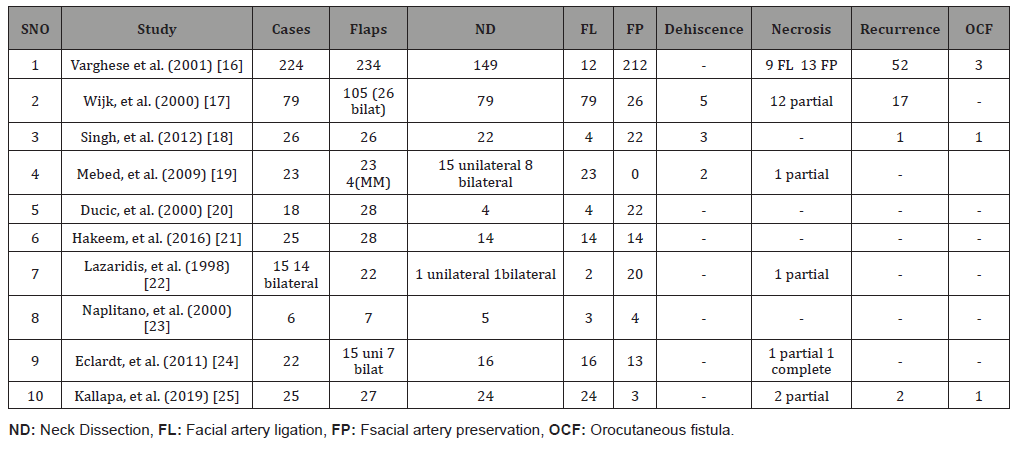
The summary of these results along with other are given in (Table 1). A metanalysis of these results show that over all 515 nasolabial flaps were performed. Facial artery was ligated in 163 while preserved in 352. Those cases where facial artery was ligated, 27 (16.5%) developed either partial or complete necrosis but in those where facial artery was preserved, only 13 (3.69%) developed partial or complete necrosis (p <0.001). Overall, 347 concomitant neck dissections were performed in these cases with overall locoregional recurrence rate of 20.7% (72) cases. It is however not clear that whether risk of neck recurrence increased with facial artery preservation [16-25].
Table 1:
Conclusion
Nasolabial flap is a widely harvested flap in head and neck region for local reconstruction. Its width can be a limiting factor but if raised bilaterally, can compensate for it. Extended flaps may be required occasionally for more complex and inferior defects. In such cases where concomitant neck dissection is planned, facial artery ligation may compromise flap survival. Risk of recurrence associated with facial artery preservation is not clear even if it is an elective procedure.
To read more about this article...Open access Journal of Dentistry & Oral Health
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers