Authored by Kratika Mishra*,
Abstract
Mucormycosis (MCM) is a life-threatening infection that carries high mortality rates with devastating disease symptoms and diverse clinical manifestations. This article briefly explains clinical manifestations and risk factors and focuses on putative virulence traits associated with mucormycosis, mainly in the group of diabetic ketoacidotic patients, immunocompromised patients. The diagnosis requires the combination of various clinical data and the isolation in culture of the fungus from clinical samples. Treatment of mucormycosis requires a rapid diagnosis, correction of predisposing factors, surgical resection, debridement and appropriate antifungal therapy. The overall rate of mortality of mucormycosis is approximately 40%.
Keywords:Amphotericin B, emerging, Mucorales, mucormycosis, zygomycetes
Introduction
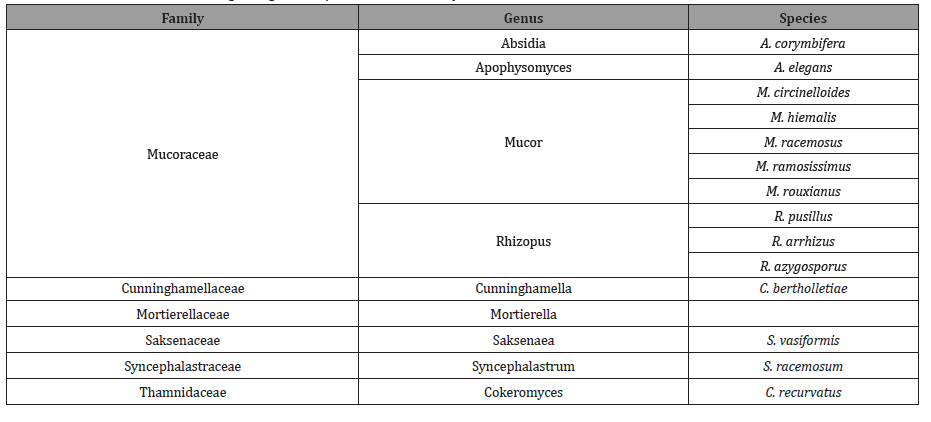
Mucormycosis is defined as an opportunistic infection, affecting patients with diabetes mellitus (DM), neutropenia, malignancy, chronic renal failure, and acquired immunodeficiency syndrome and those who have received organ or hematopoietic stem cell transplants, it can affect immunocompetent hosts as well (such as trauma patients) [1,2]. It is third invasive mycosis after candidiasis and aspergillosis which is caused by several species of different genera [3] (Table 1).
Table 1: Classification of the aetiological agents responsible for mucormycosis.
This mucormycosis infection is caused by Mucorales. Zygomycetes is the class that is divided into two orders i.e., mucorales and entomophthorales. Mucormycosis is a fulminant disease with high rates of mortality and morbidity that mainly affects the immunocompromised patients.
This disease is characterised by host tissue infarction and necrosis. Tissue necrosis due to blood vessels invasion and subsequent thrombosis are the hallmarks of invasive mucormycosis. In a French study, mucormycosis incidence increased by 7.3% per year in neutopenic patients [4].
Routes of Transmission
The most common route of transmission is inhalation of spongiosprores. Other routes are direct implantation into injured skin like burns, intra-venous drugs administration, exposure or trauma with contaminated soil. It is rapid progressive disease extending into neighbouring tissues, including orbit and brain involvement in more severe cases.
Classification of Mucormycosis is based on the involvement of anatomic sites of infection reflecting in part the portals of their entrance in the humans. The spores enter through different routes of transmission the disease may present as rhino-orbitalcerebral, pulmonary, cutaneous, subcutaneous, gastrointestinal and disseminated form [5,6].
Discussion
The mortality rate of mucormycosis is approximately 40%, but this rate depends on the clinical presentation of the disease, the underlying disease, surgery, and the extent of the infection [7,8,9,10].
Mucormycosis occurs in patients with diabetes mellitus and ketoacidosis, haematological malignancies [11,12,13,14] like neutropenia [12,15] or graft vs. host disease, in solid-organ transplant patients [11,19,20,18–33] and in patients receiving high doses of corticosteroids [34].It is infrequent in immunocompetent patients like those patients that are without any risk factors,HIVinfected patients and patients with solid organ tumors [35,36].
Mucormycosis most commonly occurs in the sinuses (39%), lungs (24%), skin (19%), brain (9%), and gastrointestinal tract (7%), in the form of disseminated disease (6%), and in other sites (6%) [37]. With the exception of rhino-cerebral and cutaneous mucormycosis, the clinical diagnosis of mucormycosis is difficult, and is often made at a late stage of the disease or post-mortem [38].
Diagnosis includes tests using cultures of clinical samples, sputum analysis, histopathological testing and it requires the combination of various clinical data and the isolation in culture of the fungus from clinical samples. Other techniques involve computed tomography scans, magnetic resonance imaging. Magnetic resonance imaging is technique of choice when intracranial structures are affected. Molecular biology advances would greatly improve diagnosis in such deadly disease.
Treatment depends on early diagnosis, correction of predisposing factors, anti fungal therapy, surgical debridement and resection. Patients with diabetic ketoacidosis should be addressed and suppression of corticosteroids should be done. The best treatment of mucormycosis is rapid and complete surgery. Surgery combined with use of antifungal therapy is best choice of treatment [39,40,41]. Current studies suggest that point to high dose liposomal amphotericin B has shown variable activity in vitro against agents responsible for mucormycosis. Other drugs of choice includes itraconazole, voriconazole, posaconaazole, ravuconazole [42]. Other therapeutic alternatives include cytokines such as gamma interferons or granulocyte-macrophage colony stimulating factors for treatment of mucormycosis [43,44].
Conclusion
This life-threatening fungal infection is characterised by host tissue infarction and necrosis that occurs in immunocompromised patients with high rates of mortality. Further studies are required to analyse and better optimise induction and consolidation treatment. The clinical outcomes of patients with mucormycosis are poor especially in patients with uncontrolled diabetes and age is negative prognostic factors.
To read more about this article....Open access Journal of Clinical Case Studies
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers





No comments:
Post a Comment