Authored by Ivan N Koshits*,
Introduction
In modern ophthalmology, until recently, there were no reliable methods of diagnosis that allow to reliably and objectively separate the age-related eye hypertension (AEG) and the initial stage of open-angle glaucoma (OAG). Therefore, often the doctor is forced to make a decision on the diagnosis of AEG or OAG not based on objective, reliable and numerical data on the level of IOP in the patient’s youth, but according to the mythical level of statistical IOP rate which is actually as highly reliable as in the case of treatment by the criterion of average temperature in the hospital. That is, the decision is forced to be made in many ways intuitively and without a clear idea of whether the current level of IOP for the patient at this age is normal or abnormal. Attempts to carry out reliable diagnostics for reliable separation of AEG and OAG using archaic criterion intraocular pressure level” do not allow doing it for the following reasons [1-3].
1. Lack of IOP standards for healthy eyes with AEG and eye standards with OAG in the world today, which take into account
Region of residence and race of the patient,
Patient age according to the world health organization (who) classification),
The level of blood pressure,
Type of refraction,
Belonging to the low, medium or high range of ophthalmotonus in youth,
Background value of the current rigidity of the fibrous membrane of the patient’s eye,
The level of current fluctuations of the sclera (it’s new to ophthalmology concept)
2. Low accuracy of measurements of the level of IOP that will not reliably make a diagnosis of AEG or OAG [4,5]
3. The absence of baroreceptors in the eye, which does not allow the eye to control the level of IOP, so the eye is able to control only its volume [3,6,7].
Therefore, there is a need to develop new theoretical ideas about the physiological nature of intraocular pressure and regulatory functions of sclera. But it was also necessary to develop new methods of dynamic diagnostics, allowing reliable and reliable separation of AEG and OAG.
Material and Methods
The first group consisted of patients with AEG under the age of 75 years, a total of 326 healthy eyes with a high range of IOP in youth. The second group consisted of patients aged 55-76 years with primary OAG, a total of 75 glaucomatous eyes with a low range of IOP in youth. The level of current true IOP in both groups at the time of the examination was 23-28 mmHg for the differential diagnosis we used the modified pneumatic analyzer ORA, whose computing platform was thoroughly upgraded [1-3,8-10]. This allowed the Koshits-Svetlova method to determine in vivo the volumetric rigidity of the fibrous sheath of the eye (FSE), the true IOP according to Goldmann, the IOP level in youth, the belonging of the eye to the low-range, average, or high-range IOP rates, as well as the parameter introduced by us – scleral fluctuation (SF) [1-3,9- 12].
In Figure 1 the scheme shows measurement of physiological parameters of FME using our technique. SF is a new functional parameter in ophthalmology, which characterizes the ability of the sclera to restore its original shape after the pneumatic impact. SF also characterizes the functional ability of F to directly participate in the outflow of intraocular fluid, due to the retaliatory reduction of the internal volume of FSE with the help of pre-stretched elastic collagen fibers of the sclera and myofibroblasts (Figure 1).
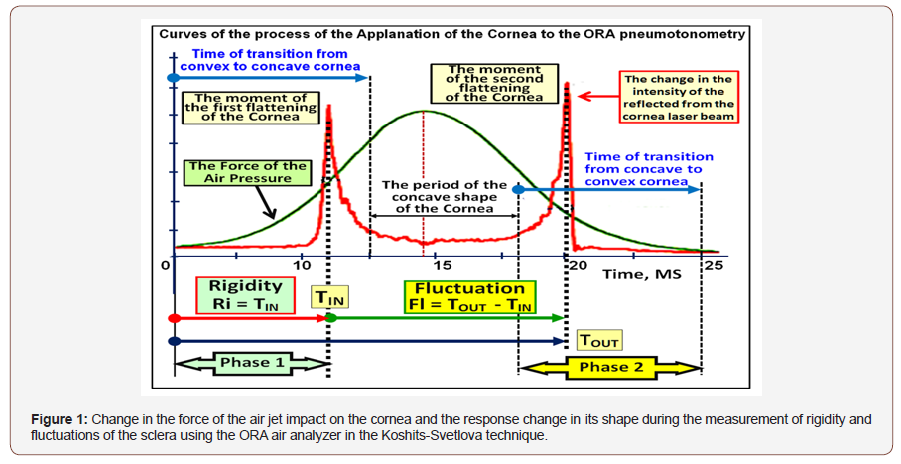
Phase 1 Increase in the volume of the sclera due to displacement of intraocular liquid under the cornea. The rigidity of the sclera prevents this increase in volume.
• Phase 2 Restore the shape of the cornea using the elastic structures of the sclera.
Today this dynamic diagnostics can be carried out by our techniques also using a pneumatic analyzer Corvis ST, which as well as air analyzer ORA allow you to determine when the first and second flat state of the cornea in the process of the impact of a jet of air (Figure 2).
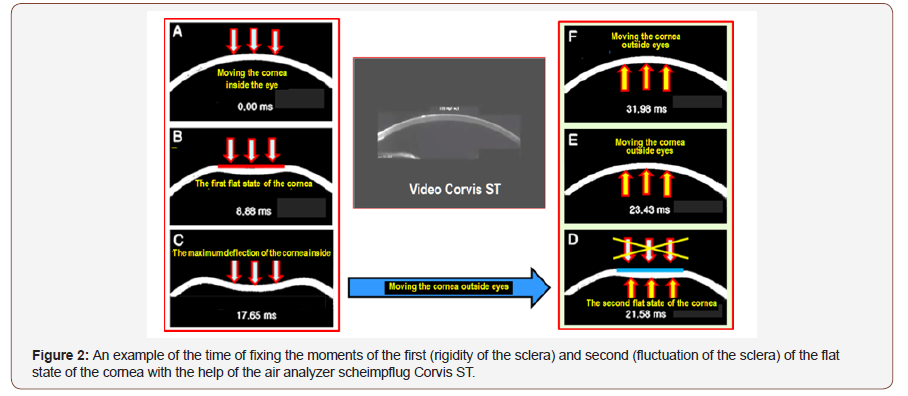
It should be noted that the time of the whole process of pneumatic action on the eyes of analyzers ORA and Corvis ST is not more than 30 milliseconds. At the same time, the intraocular volume remains constant, since the intraocular fluid does not have time to leave the eye outward along the paths of its slow drainage and diffusion. This allows you to avoid significant errors during the measurements and allows to consider this method as close to the standard.
Results
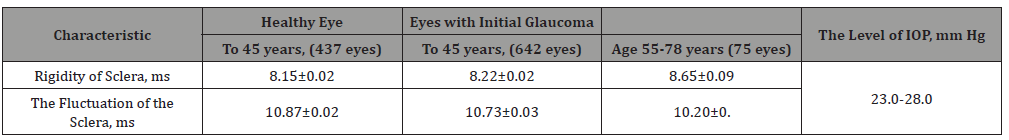
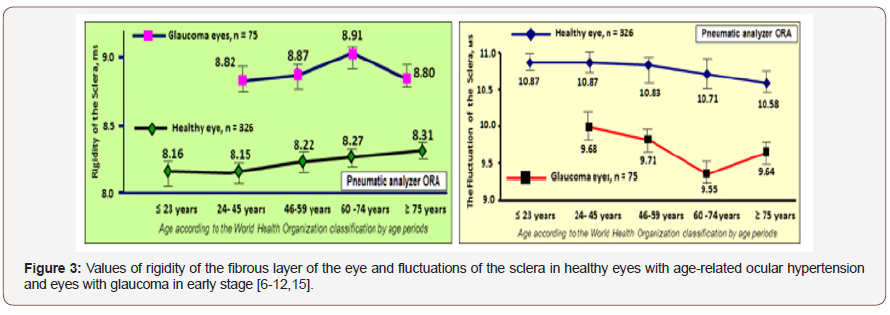
The increase in rigidity and decrease in scleral fluctuation with age are presented in table 1. A comparison of the values of the rigidity of FSE in healthy and glaucoma’s eyes within a close age group reveals significantly higher level of stiffness in glaucoma’s eyes than in healthy and, consequently, a lower level of fluctuations of the sclera Figure 3. In the eye with OAG age-increased rigidity of the sclera superimposes the processes of accelerated aging of FSE, which leads to abrupt jump in rigidity and a significant reduction in the functional capacity of the sclera to fluctuate. This significantly reduces viscoelastic and functional properties of FSE in general. Moreover, the level of FSE rigidity in the glaucomatous eye already in the early stages of OAG significantly exceeds the levels of rigidity compared to healthy eyes with AEG in the elderly. But the most important thing is that the regions of finding representing the rigidity and fluctuation Figure 3 for AEG and OAG do not intersect anywhere. This allows reliably and objectively diagnose AEG or OAG separately from each other (Table 1 & Figure 3).
Table 1:
Discussion
It became clear that the development of norms/standards of rigidity and fluctuation of the sclera for healthy and glaucomatous eyes from the point of view of the physiology of the eye is much more effective than the development of standards for uncontrolled levels of IOP in the eye. After all, the fluctuation and rigidity directly characterize the current functional state of the FSE, which must be maintained independently if this is the prevention of AEG or the treatment of OAG. So, restoration or maintenance of functional fluctuations of the sclera is pathogenetically justified method of treatment of the OAG or prevention of the AEG. This will ensure functional state of intraocular exchange of aqueous humor by maintaining the level of scleral fluctuation not less than 50-60% of the norm. Targeted reduction of rigidity of the sclera or the current IOP must ensure the maintenance of the scleral fluctuations at physiologically reasonable level [9,11,12].
These biomechanical and physiological characteristics of the eye can now be determined by our method using pneumatic analyzers ORA and Corvis ST. We were able to create a theory of physiological functions of the fibrous membrane of the eye, as well as to develop new methods of dynamic diagnosis, allowing to determine numerically and reliably the following biomechanical and physiological characteristics of the eye [3,6,10,13]
• The level of rigidity of the sclera, • The level of IOP in a young patient in the elderly, • The level of sclera fluctuation, which characterizes the degree of preservation of the functional physiological characteristics of the sclera, i.e. in particular to assess its ability to participate effectively in the regulation of the current volume of the eye, • Affiliation current IOP of the patient to an area of high (17-22 mm Hg), average (13-16 mm Hg) or low (9-12 mm Hg) Goldmann norms [14] and determination of abnormality of the current level of IOP.
Conclusion
1. Determination of biomechanical and physiological characteristics of the eye according to our methods is now possible with the help of dynamic diagnostics using pneumatic analyzers ORA and Corvis ST.
2. The new diagnostic methods developed by us allow us to reliably and reliably separate the eyes with AEG from the eyes with OAG.
3. Our new theoretical concepts allow us to create effective ways to prevent the development of AEG and OAG, as well as effective ways to treat OAG [8,10,15].
To read more about this article...Open access Journal of Ophthalmology & Vision Research
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers
To know about Open Access Publishers





No comments:
Post a Comment