Authored by Idelphonse B Ahogni*,
Abstract
Malaria is a disease declared by WHO as a public health problem in developing countries It is a parasitic infection of erythrocytes by a protozoan of the genus Plasmodium transmitted by the bites of female Anopheles mosquitoes. The risk of contracting this disease does not spare any section of the population. This study aims to assess the impact of behavioral changes in the population prone to malaria disease after having implemented preventive strategies such as solid awareness and training in repairing mosquito nets. This is a cross-sectional study conducted from April to June 2017 among children under five years of age whose parents had previously (2 years before) received nets followed by sensitization for better use (cluster 1: 115) plus LLIN repair kits (cluster 2: 121) or none at all (cluster 3 control: 137). Children were randomly selected. Thick and thin blood smears were produced on the same slide according to WHO protocols, hemoglobin was read on Hemoreader equipment and RDTs were also performed. A total of 373 children were examined and sampled. Overall prevalence of anemia was 60%. The overall prevalence of anemia was 60% with no significant difference between the three clusters (p>0.05). Out of 373 slides read by microscopy, 19.3% showed P. falciparum and no others species was identified. The prevalence of malaria in Group 1, cluster 2 and cluster 3 was 22.6%, 4.9% and 29.9% respectively (p<0.001). Awareness more repair kits are probably at the root of the low rate of parasitized children in cluster 2 (p<0.001). This assessment showed a low prevalence of parasitaemia in children whose parents received LLINs and repair kits and were sensitized to better use. The National Malaria Control Program (NMCP) should be more involved in raising awareness of behavior change for better net use.
Keywords: LLIN, Malaria, Parasitemia, Anemia, Benin
Abbreviations: ACTs: Artemisinin-based Combination Therapy; BCC: Behaviour Change Communication; CREC: Centre de Recherche Entomologique de Cotonou; LLIN: Long-Lasting Insecticidal Nets; NMCP: National Malaria Control Program; PADNET: Advance the Durability of Long-Lasting Insecticide-treated Nets; PTDP: Parasitic Thick Drop Positivity; RDT: Rapid Diagnostic Test; WHO: World Health Organization
Background
Malaria, the world’s leading parasitic disease, is now a real public health problem that threatens more than 2.4 billion people worldwide, i.e. nearly 40% of the world’s population (WHO, 2008) [1]. Global malaria mortality has been estimated at 405,000 in 2018, compared to 416,000 in 2017 and 585,000 in 2010 [2].
In Benin, malaria is a real public health problem due to its high prevalence, severity and significant socio-economic consequences. The entire population is exposed to malaria. However, pregnant women and children under five years of age continue to be the most vulnerable groups and are exposed to severe forms of the disease. According to the Yearbook of Health Statistics 2018, malaria accounts for 45.8% and 49.7% of the reasons for consultation among the general population and among children under five years of age respectively. The incidence of the disease in 2018 was 17.1% in the general population and 36.3% in children under five years of age [3]. Considering the severity of the disease, Benin has opted to implement malaria control strategies adapted to the specificities of the different epidemiological facies, integrating the strengthening of multiple prevention methods on the one hand and the improvement of early and correct access to malaria diagnosis and treatment on the other hand [3]. The strategic lines of control are based on prevention, case management including the confirmation of all cases before treatment and the use of ACTs, monitoring the efficacy of antimalarial drugs, and monitoring the efficacy of longlasting insecticidal nets (LLINs) [3]. The use of LLINs has become one of the most important and effective mass prevention methods against malaria [4-5]. Evidence for the efficacy of LLINs is well known [4-6] and in Benin, efforts for their mass distribution are in line with WHO recommendations [7-12]. The success of LLINs in malaria prevention is due to the fact that they provide both effective individual protection for users and community protection if net coverage is high enough to reduce vectorial capacity [13]. For this reason, universal access is a primary goal to be achieved for WHO and malaria control programmes. In October 2007, the country organized an integrated LLIN distribution campaign targeting children under five years of age with vitamin A, albendazole deworming. A total of 1,500,000 LLINs were distributed. In July 2011, a campaign was organized in conjunction with the polio vaccination, with administration of vitamin A and albendazole de-worming. A total of 4,000,000 LLINs were distributed during this campaign. In August 2014, 6,077,272 LLINs were distributed to households. In 2017, 6,552,158 LLINs were distributed out of the 6,741,542 pre-positioned LLINs, i.e. 97.19%. LLIN ownership increased remarkably from 2006 to 2017, from 25% to 92%, and LLIN use increased from 20.1% to 82% among children under 5 years of age and from 19.6% to 85% among pregnant women.
However, one of the handicaps associated with the promotion of LLINs is premature wear and tear. According to manufacturers, LLINs can last 3 years and withstand 20 washes. But under field conditions, many studies show that their lifespan is shorter. In Benin, after the distribution of Olyset LLINs in 2011, 90% of these nets had holes after 2 years of use in rural areas [14-15]. To address the problem of low durability of LLINs in field conditions, the Project to Advance the Durability of Long-Lasting Insecticidetreated Nets (PADNET) has initiated a study based on the proper use of these nets to reduce the frequency of holes and tears, which should result in an increase in the lifetime of LLINs. This increase in lifespan should be accompanied by greater entomological and epidemiological effectiveness. It is within this framework that this study was carried out with the aim of assessing the impact of three prevention strategies on Plasmodium falciparum infection and anaemia in children aged 0-5 years sleeping under LLINs and whose households may or may not be aware of best practices for use.
Methods
Type and period of study
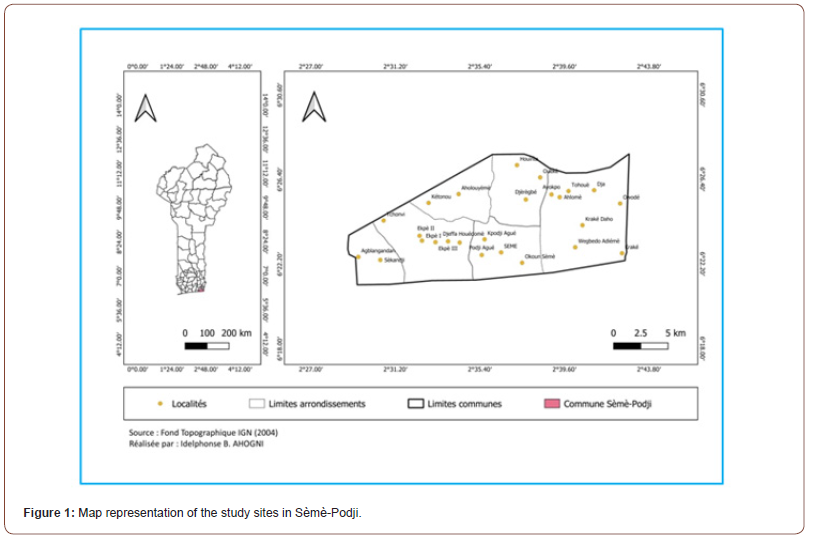
We conducted a cross-sectional descriptive study from April to June 2017 in the commune of Sèmè-Podji (data collection site) and at the laboratory of the entomological research centre in Cotonou (data management site).
Study site
The study was conducted in the commune of Sèmè-Podji, located between parallels 6°22’ and 6°28’ North latitude and meridians 2°28’ and 2°43’ East longitude in the department of Ouémé, south-east of the Republic of Benin on the Atlantic coast. The commune of Sèmè-Podji is bounded to the North by the city of Porto-Novo and the Aguégué, to the South by the Atlantic Ocean, to the East by the Federal Republic of Nigeria and to the West by the city of Cotonou. Its climate is tropical Sudano-Guinean with two dry seasons (December to February and August to September) and two rainy seasons (April to July and October to November). The average temperature is around 27°C with relatively high humidity. The influence of the coastal wind on the climate often creates cyclical disturbances that make the commune of Sèmè-Podji, one of the wettest areas in southern Benin with an average annual rainfall exceeding 1,100 mm [15-17]. Agriculture in this commune occupies the majority of the population without distinction of gender and age groups. An increase in livestock farming is also noted in sectors such as pigs, cattle and sheep, goats, rabbits and aulacodes. These conditions are favourable to the development of Anopheles gambiae, vector of the parasite Plasmodium falciparum, which causes malaria.
Study population and sample size
The study was carried out in 3 clusters
Cluster 1: 115 children under 5 years of age sleeping under LLINs whose households were informed about best practices for use,
Cluster 2: 121 children under 5 years of age sleeping under LLINs whose households were informed about best use practices and who have received kits to repair these LLINs if needed,
Cluster 3: 137 children under 5 years of age sleeping under LLINs with no other information received (control).
A total of 373 children were randomly selected from the households involved in the ‘’Impregnated Nets Life Extension Project’’ study out of a total of 593 children in the study. The conditions for obtaining this size are based on the R software. Core Team software (version 3.31-2016).
Inclusion criteria
All non-ill children under 5 years of age whose parents have agreed to participate in the study and who have given their consent for samples collection.
Study Setting
The study consisted of collecting blood from children aged 0 to 5 years in health center and study sites. Analyses of the blood collected are carried out in the Centre de Recherche Entomologique de Cotonou (CREC).
Ethical considerations
By decision No. 29 of 19/11/2013 PADNET, obtained the ethical opinion after submission of the study protocol to the National Research Ethics Committee of Benin,
All children are systematically subjected to temperature taking. Those over 38°C are subjected to the Rapid Diagnostic Test (RDT) and were routinely managed after testing positive for RDT.
Data Collection
We went to the different center of chosen places according to a schedule of visits previously submitted to the children’s parents. The collection procedure consisted of the following steps:
1. Interview with the women or the community relays who came with the children through “counseling”,
2. The children accompanied by the mothers or relays were directed to the room where the samples were taken,
3. Additional information on the study was given to the relays or mothers with precise explanations on malaria (origin, causes, consequences, modes of prevention),
4. A case notification form was filled in order to determine the possible risk factors associated to malaria disease.
Technical methods of blood collection
Blood sample were collected from children by a laboratory technician following appropriate SOP. Approximately 2-4 ml of venous blood were collected in a EDTA K3 tube labeled with patient ID. A thick and thin blood smears were produced from EDTA K3 tube on labeled slides.
Determination of hemoglobin
Hemoglobin concentration (g/dl) were performed by Hemo- Control EKF Diagnostics using undiluted blood. The haemo-drive control was used worth a short light path containing three reagents: sodium deoxycholate, sodium nitrate and sodium acid. Only 10/μL of capillary blood were required. It was introduced into a device and the hemoglobin result was obtained in less than 60 seconds.
Examination of the slides
Slides sent to the laboratory are subject to double reading by qualified technicians. A search for Plasmodium were carried out on the Giemsa-stained slides (thick drop for the search and blood smear for the identification of the Plasmodium species). Asexual forms of Plasmodium were counted in a blood volume occupied by 200 leukocytes and the parasite density were calculated assuming that the number of leukocytes/μL of blood is equal to 8,000 (according to WHO recommendations). The thick smears were read by the same experienced technicians.
Statistical analysis
The data collected was encoded, processed and analyzed using SPSS version 21 software (Chicago software package). The R version 3.6 software was also used for certain analyzes, including the determination of Odds ratios, the Chi-square test. Thus, multivariate logistic regression allowed the comparison of the different study groups in terms of sex, age in relation to parasitemia and anemia. To show the impact of using LLINs with awareness and / or tear repair kits as a limiting risk factor for malaria, we used the Chi-square test, the confidence interval and the test, of equal variances.
Results
Socio-demographic data from the survey of children in the three clusters
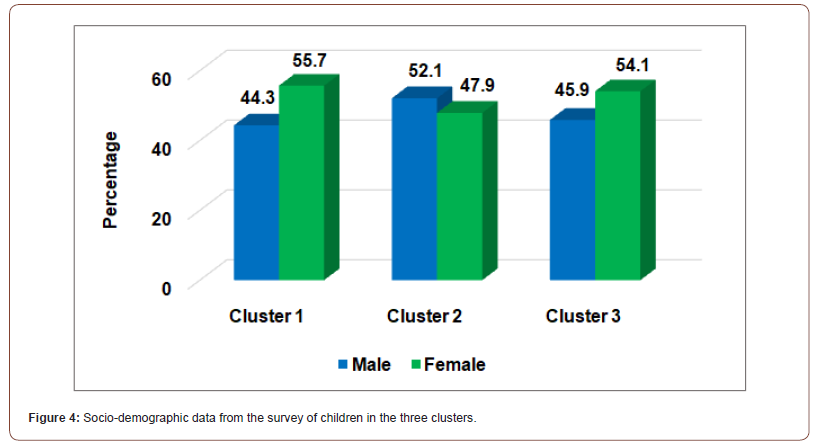
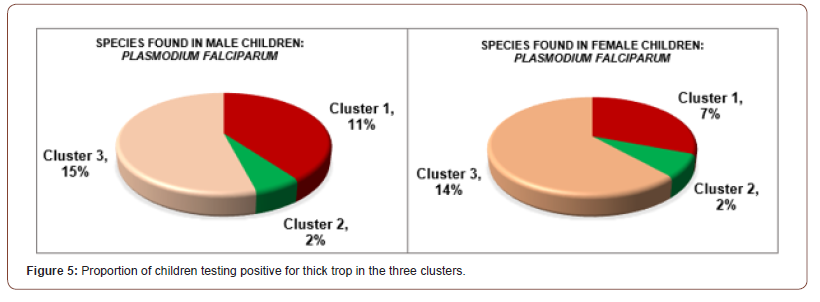
The sample size for the three studied clusters combined were 373 children aged from 2 to 60 months. Samples were collected from all 373 children. The mean age was 48 months and the sex ratio 177/196 (90%) (in the three clusters combined). The average age of the children was 48 months (4 years), the minimum age was 2 months and the maximum age was 60 months (5 years). The proportions of female children were slightly higher than male children in clusters 1 (55.7% vs. 44.3%) and 3 (54.1% vs. 45.9%) in contrast to cluster 2 (47.9% vs. 52.1%) (Figure 4). Out of 373 slides read by microscopy, 19.3% showed P. falciparum and no other species was identified. The prevalence of malaria in cluster 1, cluster 2 and cluster 3 was 22.6%, 4.9% and 29.9% respectively (p<0.001). Only 2% of both girls and boys were positive in cluster 2 compared to 7% and 11% in cluster 1 and 14% and 15% in cluster 3 (Figure 5). Of all the children tested positive, the only species found was Plasmodium falciparum.


Prevalence of anaemia in children in the three clusters by sex
Table 1 above presents the result of the analysis of hemoglobin levels by sex in the three clusters according to World Health Organization (WHO) criteria. Overall prevalence of anaemia was 60%. There was no statistical difference when anaemia is considered between the three groups (p>0.05). The results of this survey shown none of the children in clusters 1 and 3 had severe anaemia, 2.6% of the boys in cluster 2 had. On the other hand, the proportion of children with mild anaemia were ranged from 42.1% to 55.5% (all clusters combined) against 44.4% and 56.4% for those with moderate anaemia.
The results of this survey show non-significant difference by age in the clusters. Anemia was more present in children aged from 36 to 60 months in clusters 1, 2 and 3 (26.1%; 35.1% and 21.9% respectively). The prevalence of mild anaemia was similar in the three clusters and only one child showed a severe form of anemia (cluster 2). For each additional year, the odds to be anaemic (versus not to be anaemic) increase by a factor of 1.02. The Likelihood Ratio Test statistic was 18.259 (chi-squared distributed with four degrees of freedom). The associated p-value (p<0.001) indicated that our model fits significantly better than the model with only the intercept. The p-value associated to the Hosmer & Lemeshow Goodness of fit test is 0.456 which is greater than 0.05. Thus, the model adequately fits the data (Table 2).
For each additional year, the odds to be anaemic (versus not to be anaemic) increase by a factor of 1.02. The Likelihood Ratio Test statistic was 18.259 (chi-squared distributed with four degrees of freedom). The associated p-value (p<0.001) indicated that our model fits significantly better than the model with only the intercept. The p-value associated to the Hosmer & Lemeshow Goodness of fit test is 0.456 which is greater than 0.05. Thus, the model adequately fits the data (Table 3).
Table 1: Distribution of haemoglobin levels by sex in the three clusters..
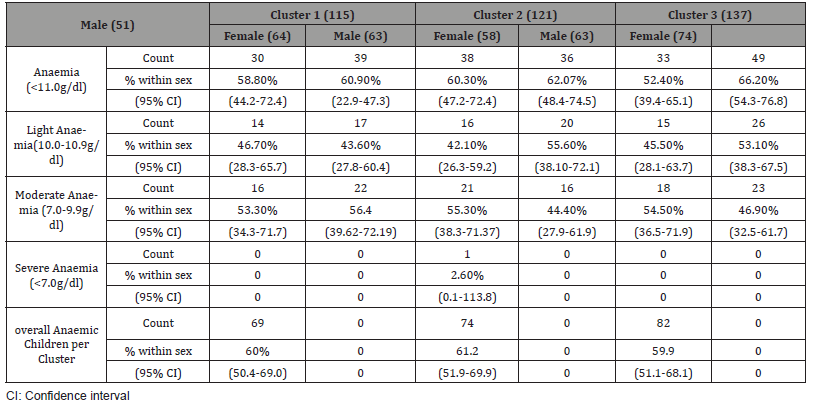
Table 2: Distribution of the anaemia rate according to ages in months at clusters..
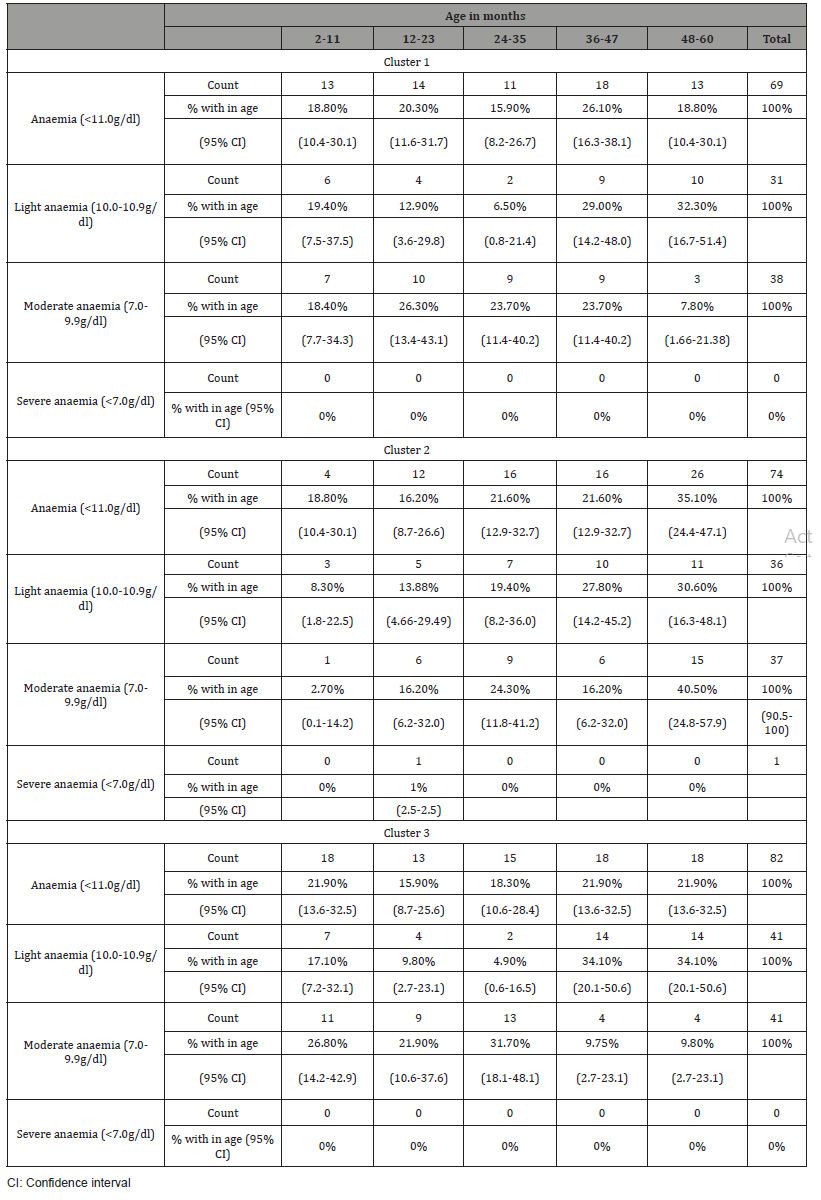
Table 3: Summary of Logistic Regression Analysis for variables predicting anemia (clusters, age and gender) for 323 children under five..
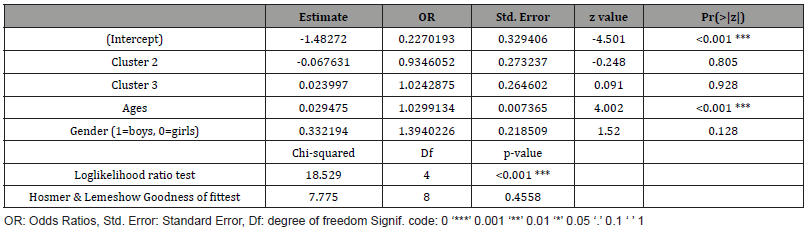
Table 4: Variations in parasitic thick drop positivity (PTDP) and TDR positivity in the three clusters..
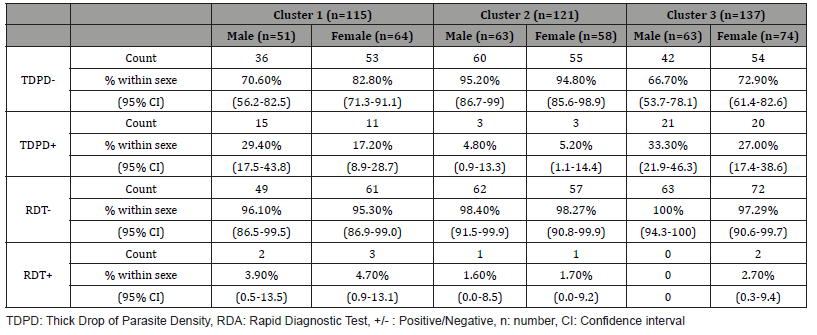
Table 5: Distribution of parasitaemia as a function of age (in months) in the children’s clusters..
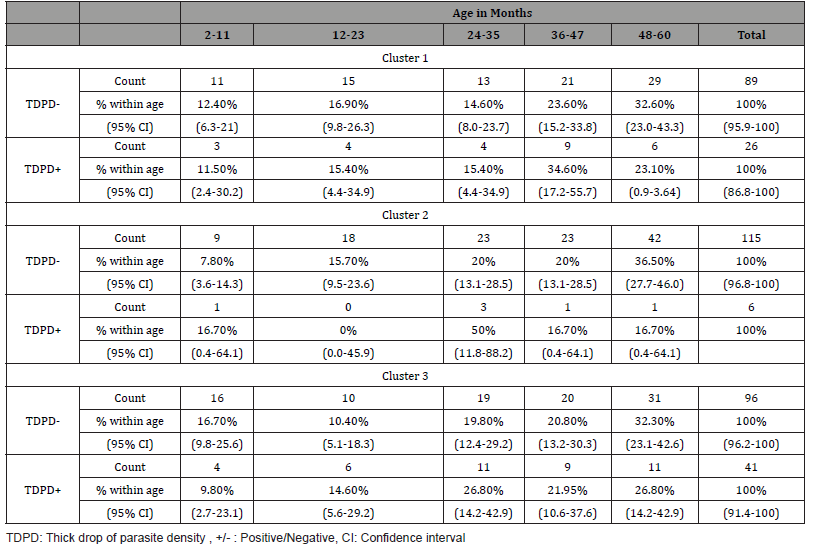
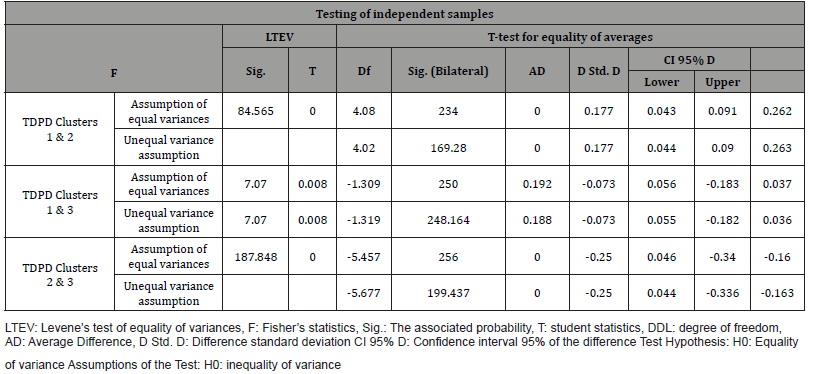
Table 6: Test ofStudent for comparison between means..
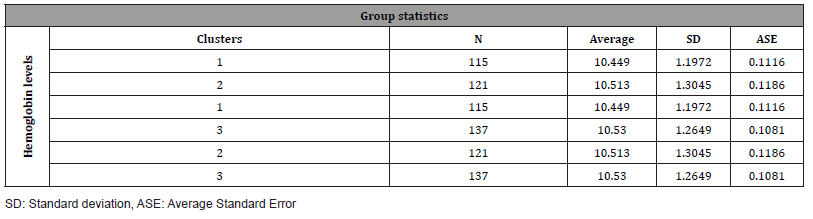
Table 7: Test for comparison of variance between the three clusters in the study..
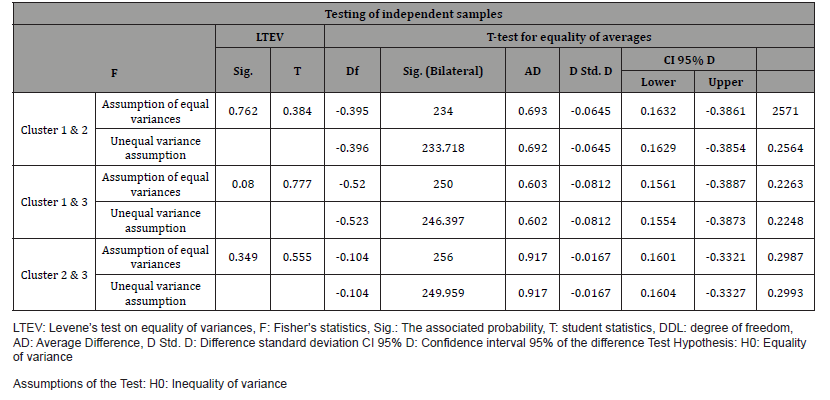
Table 8: Summary of logistic regression analysis for variables predicting parasitemia (clusters, ages and gender) for children under five years..
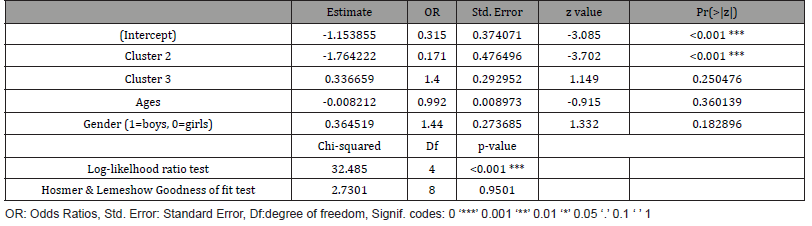
Table 9: Test ofStudent for comparison between means..
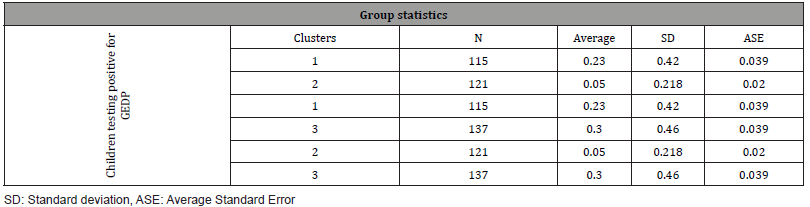
Table 10: Test for comparison of variance between the three clusters in the study..
Microscopy and RDT results in the three studied clusters
Microscopy results by gender
Table 4 shows the distribution of microscopy results. Children of cluster 3, were the most parasitized with 33.3% for male against 27.0% for the female. Table 4 shows the distribution of microscopy results. There was a significant difference between cluster 2 compared with clusters 1 and 3 (p<0.0001).
Positivity of the RDT by gender
A RDT was systematically performed for all children whose body temperature was above 37 degrees Celsius regardless of the cluster. Less than 5% of the children who were tested (all clusters) had a positive RDT (Table 4).
Thick drop positivity by age
Table 5 shows the prevalence rates of malaria parasitemia in children by age (2-60 months). Overall, the results of the thick droplets show that the most parasitized children (34.6% and 26.8%) were those between 36 and 47 months of age. However, it should be noted that the prevalence of malaria parasitemia increase with the age of the children.
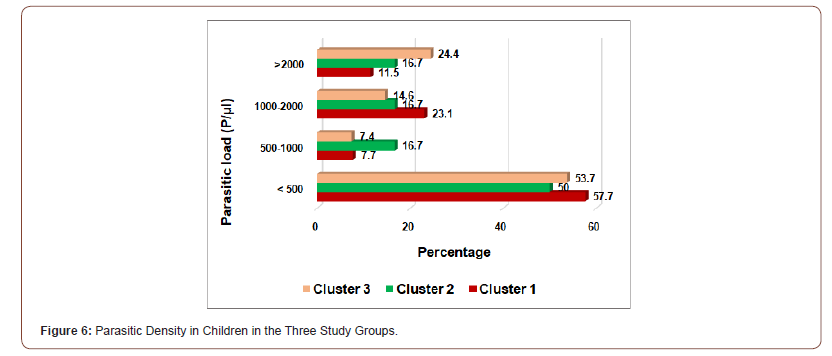
Parasitic density in children in all three studied clusters
In clusters 1, 2, 3, respectively, 57.7% (15/26), 50% (3/6) and 53.7% (22/41) of children testing positive had parasitaemia of less than 500 parasites/mm3. Parasitemia’s greater than 2,000 parasites per microliter of blood were observed in cluster 3 (24.4%) and the lowest in cluster 1 (11.5%) (Figure 6).
Impact of Behaviour Change Communication (BCC) on parasitaemia and anemia in the three clusters
On anaemia: In this table, we determined the effect of sensitization (Cluster 1) and repair kits (Cluster 2) on haemoglobin levels compared to children sleeping under LLINs whose parents did not receive any form of sensitization or tear repair kit (Cluster 3). There was little variability in the three groups. In summary, there was no significant difference in mean hemoglobin levels between the three studied clusters. Thus, there was no association between LLIN use and anemia with regard to the strategy adopted for its use (Table 6).
Test of equality of Variance (Levene test)
Table 7 allowed us to compare the variation between the proportions of anaemic individuals between the different clusters. It has been observed that with this test, contracting anaemia was not linked to the cluster in which the child was (p˃0.05).
Comparatively to children of cluster 1, being in cluster 2 led a decrease in the odds to be parasitized (versus not to be parasitized) by a factor of 0.17. Moreover, there is no any statistical significant difference between children in cluster 1 and children in cluster 3 with respect to thick drop positivity (Table 8). The chi-squared test statistic of 20.8, with two degrees of freedom was associated with a p-value < 0.001 indicating that the overall effect of cluster is statistically significant.
We compared the mean of parasitized individuals between the different clusters. A significant difference was observed between the mean of the positive thick drops of individuals of cluster 2 compared to cluster 1 and 3. There was however a difference between those of cluster 1 and 3 though this difference was not significant (Table 9).
Test of equality of Variance (Levene test)
Table 10 allowed us to compare the variation in the proportions of parasitized individuals between the different clusters. It was observed that the probability associated with this test at the end of the relationships between the different groups and the parasitaemia is p = 0.008. This probability is <5%, therefore, there is a significant difference between the variances of the groups.
Discussion
During this study on three prevention strategies for Plasmodium falciparum infection (prevalence of parasitaemia) and anaemia on children aged 2 to 60 months in the district of Sèmè-Podji in southern Benin, we were worked on a sample of 373 children out of 595 in the cohort.
The 36-48 months age group was the most represented. The mean age of the children was 48 months. The youngest age was 2 months and the old and the eldest 60 months (5 years). In our study, the most affected children anemia between 36-60 months old. The results of Nathalie and Ngnie et al. from Benin and Cameroon [16, 17] who found respectively a higher frequency of what in infants 12- 24 months of age (43% and 85.4%) contrasted with our own (about 20.29%) in infants of 12-23 months of age in our three studied clusters. In Tunisia, a study carried out showed that the prevalence of anaemia reached and exceeded the threshold of 50% in children aged between 6 and 23 months [18]. Other studies conducted in Guinea [19]; Cameroon in 2009 by D. Danielle [20] and Measureds in 2008 in Burkina Faso [21] found respectively: 79% in children between 6 months and 59 months; 80.8% in children under 5 years and 99.4% in children between 10-11 months. This difference could be due either to the causal condition or to the location of the surveys. Although the prevalence of anemia was lower in our study, we found no association between the use of LLINs and this condition with regard of the strategy adopted for its use.
The prevalence of positive thick drops varies from one group to another in our study. This finding has already been done in other studies where the prevalence of thick drops varied: 32 to 53% in Benin [22], 60.26% in Equatorial Guinea [19], 40 to 80% in Burkina Faso [21], 85 to 95% in Congo [23] and 10% in Senegal [24] in asymptomatic children.
The systematic performance of the RDT for children with fever above 37 degrees showed that only 4.7% of children were positive for TDPD. This result indicates that fever may be associated with low parasitaemia (probably due to several other causes), while high parasitaemia may remain asymptomatic. Thus, the combination of fever and positive TDPD to diagnose malaria in endemic areas is not sufficient, even in the absence of clinical signs suggestive of another condition [21,24].
Overall, the results of the thick drops in our study show that the most parasitized children (34.6% and 26.8%) were those aged between 36 and 47 months (clusters 1 and 3), compared to 50% for children aged between 24 and 36 months in (cluster 2). The low rates obtained were 11.5%, 9.8% (between 2 and 11 months). Other authors have shown the precocity of Plasmodium Falciparum carriage in endemic areas [23]. It appears from our study that Plasmodium falciparum, the parasite responsible for the pathology of malaria was the only parasite responsible of the positivity of the test for the positive children. Our study reveals that malaria prevalence was 22.6% (26/115), 4.9% (6/121) and 29.9% (41/137) for clusters 1, 2 and 3 respectively. These results contrast with those of the Cocody study showing the prevalence of 41.97% for Plasmodium falciparum and 24.91% for intestinal parasitosis (ascariasis) [25]. In Senegal, a study carried out shows that malaria due to Plasmodium falciparum has a high incidence in children aged 4-5 years. This incidence was 87.2% in Ghana, 63.8% in Uganda, 84% in Abidjan and 45.5% in Nigeria [26]. The ecology of the study environment in each country added to the fact that we could not carry out all the required assessment to be able to find all the pathologies which could be related to the cause of the anaemia in our study could explain this noticed difference. If there is no statistically significant difference between clusters 1 and 3, we had, however, noted that it exists when we compare these two clusters to cluster 2 with regards to the parasitaemia of the children whatever the sex. Sensitization and repair kits for possible tearing of nets could explain the low number of children infected in cluster 2.
Conclusion
This assessment showed a low prevalence of parasitaemia in children whose parents received LLINs and repair kits and were made aware of better use. It is therefore crucial and very important that the national malaria control program of the Ministry of Health increasingly involves in these strategies awareness of behavior change and the provision of remedies, especially LLINs.
To read more about this article...Open access Journal of Biology & Life Sciences
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers





No comments:
Post a Comment