Authored by Joshua G Cohen MD*,
Summary
Objective: Our objective was to characterize the association between demographic features and perioperative outcomes in patients undergoing non-elective ovarian cancer surgery.
Methods: Women undergoing ovarian cancer surgery between 2010 and 2015 were identified in the Nationwide Readmissions Database. Patients were divided by whether they had elective or non-elective surgery. Demographic and clinical characteristics, post-operative outcomes including length of stay, adjusted costs at index hospitalization, readmission rates, and mortality were compared between groups. Multivariable analyses were employed to assess the association between baseline characteristics and non-elective surgery, and relevant clinical outcomes.
Results: Of 101,993 patients undergoing ovarian cancer surgery, 19,349 (19.0%) were classified as non-elective. Non-elective patients were more likely to have Medicaid coverage (13.3 vs. 6.4%, p<0.001) and had a higher average Elixhauser Comorbidity Index (3.7 vs. 3.2, p<0.001). Significant predictors of non-elective admission included lowest income quartile relative to highest (odds ratio (OR)=1.27 [1.12-1.43]) and age <50 relative to age > 70 (OR=1.62 [1.45-1.82]). Multivariable analysis revealed that patients presenting for non-elective surgery had significantly higher in-hospital mortality (OR=2.82 [95% Confidence Interval (CI)=2.22-3.58]) and 30-day readmission rates (OR=1.25 [1.15-1.36]). Patients presenting non-electively spent 3.3 more days in the hospital [95%CI: 3.0-3.5]) with $6,188 more in adjusted costs [95%CI: $5,497-6,879].
Discussion: The rate of non-elective ovarian cancer surgery remains high, with increased patient mortality and resource utilization. An independent association between lower income, public insurance, and increased rate of non-elective surgery was observed, highlighting the need to address low socioeconomic populations at risk for ovarian cancer to prevent emergent hospitalization.
Keywords: Ovarian cancer; Non-elective admission; Socioeconomic status
Introduction
Ovarian cancer is associated with significant morbidity and mortality among women in the United States. It is predicted to be the fifth-leading cause of cancer death among U.S. women in 2020 and is associated with a 5-year survival rate of 48% [1]. Optimal treatment strategies vary by histologic subtype, patient comorbidities, and suspected stage at presentation but typically include a combination of cytoreductive surgery and chemotherapy [2]. Management strategies for suspected ovarian cancer are usually developed in a non-urgent setting through patient consultation with a multidisciplinary team, including a gynecologic oncologist.
However, a major challenge of ovarian cancer management is the acuity with which these patients may initially present. Despite much effort, there remains no universal practice for screening, with several studies failing to demonstrate any survival benefit from screening with serum tumor markers or transvaginal ultrasound [3- 5]. As a result, 75% of patients present with late-stage disease, often with metastases to the peritoneal cavity as well as extra-abdominal structures [6]. Given the extent of their disease, these patients may present acutely in an emergency room setting and necessitate urgent surgical intervention; a situation in which they are unlikely to receive extensive counseling or optimal debulking at the time of surgery. They may not have a gynecologic oncologist involved in their treatment planning in this urgent setting. Review of ovarian cancer patient outcomes shows improved overall survival when a gynecologic oncologist is involved in the surgical management of these patients [7,8]. Previous research has demonstrated that these non-elective surgeries are also associated with higher rates of postoperative complications and mortality [9,10]. However, patients who undergo non-elective ovarian cancer surgery remain a poorly characterized population and few studies have examined the risk factors associated with emergent or urgent surgery.
Given the potential to reduce the morbidity and mortality associated with non-elective surgery, this study used the Nationwide Readmissions Database (NRD), a large national database, to characterize demographic and clinical features, identify risk factors, and evaluate outcomes in women undergoing urgent and emergent ovarian cancer surgery. An understanding of this population is the first step in identifying opportunities to reduce the morbidity and mortality associated with non-elective presentation.
Methods
The National Readmissions Database (NRD) was accessed and all adult patients (>18 years) admitted for surgical management of ovarian cancer between January 2010 and September 2015 were identified. The NRD is a database that utilizes state inpatient databases of the Healthcare Cost and Utilization Project (HCUP) to estimate national readmission rates for all patients regardless of insurance status. Importantly, the NRD contains verified patient linkage numbers that can be used to track patients across hospitals within a state, and accounts for 58.2% of all US hospitalizations. When weighted, this database estimates data for approximately 36 million hospital discharges each year.
Using International Classification of Diseases, Ninth Revision, Clinical Modification (ICD-9-CM) codes, the study included patients with a diagnosis of ovarian cancer undergoing cytoreductive surgery, which was defined as any surgery involving oophorectomy. The patient cohort was stratified by the nature of surgical intervention – elective versus non-elective, as coded in the NRD, with the latter defined as emergent or urgent surgery not scheduled in advance (i.e. in the setting of acute onset abdominal pain, nausea and vomiting, or peritoneal signs) [11].
Medical information for patients was extracted from the deidentified dataset for each surgical intervention group, including demographic information such as zip-code derived income quartiles and insurance coverage status, baseline comorbidities (HCUP comorbidities encoded in the NRD, as well as a calculated Elixhauser Comorbidity Index for standardized comparison), hospital care setting, operative details and post-operative outcomes. The Elixhauser index is a widely utilized marker of the relative morbidity of surgical patients [12]. In addition to the route of surgery (open, laparoscopic or robotic assisted), operative details captured included intraoperative need for small and large bowel resection, rectosigmoid resection, ileostomy or colostomy, hysterectomy, lymph node dissection, and splenic, gastric, hepatic and diaphragmatic resection. Post-operative outcomes included length of stay (LOS), adjusted costs at index hospitalization, discharge location, 30-day and 90-day readmission rates as well as in-hospital mortality.
The distributions of continuous and categorical variables were compared between ovarian cancer patients who had non-elective surgery and those who had elective surgery. Continuous variables were analyzed using the Kruskal-Wallis test, while categorical variables were evaluated using chi-square tests. Multivariable logistic regression analysis was used to identify clinical factors independently associated with non-elective surgery. Multivariable logistic regressions were also utilized to identify the independent, predictive value of non-elective surgery on intra-operative procedures and post-operative outcomes. Statistical significance was considered a P value <0.05. All statistical analyses were performed using STATA 15.1 (StataCorp LP, College Station, Texas). This study was deemed exempt by the Institutional Review Board at the University of California, Los Angeles.
Results
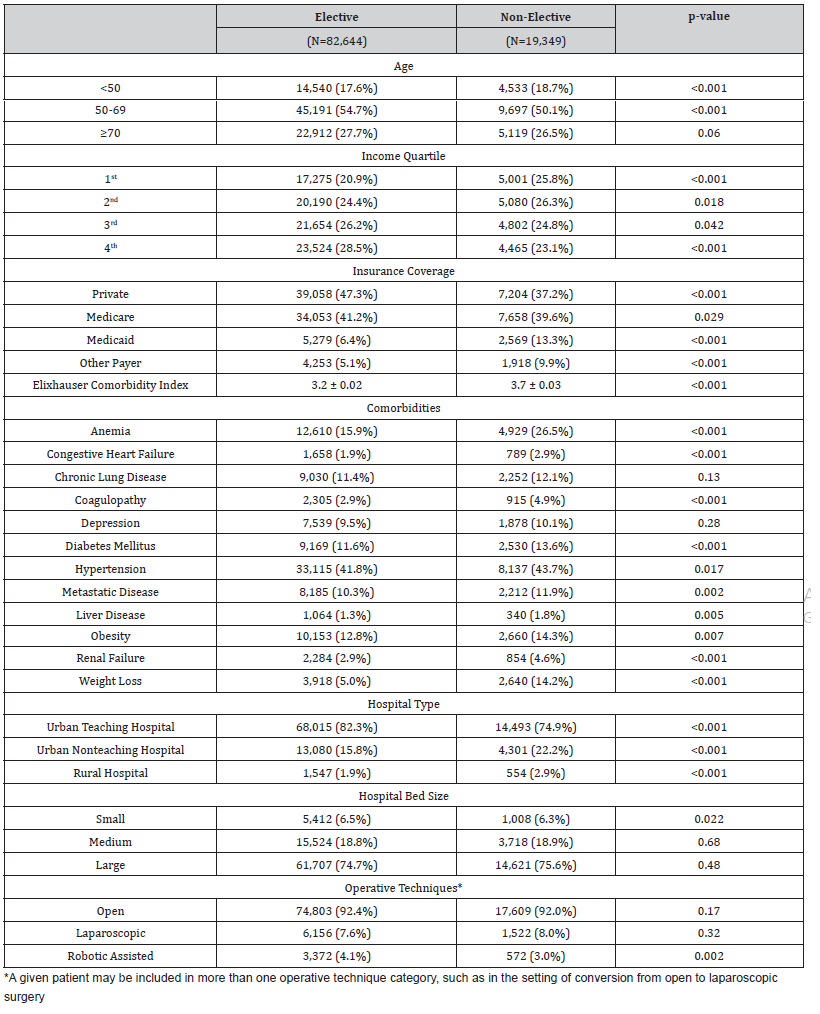
Within the NRD, 101,993 patients undergoing ovarian cancer surgery were identified, of whom 19,349 (19.0%) had non-elective surgery (Table 1). Patients presenting non-electively were on average younger (59.4 vs 61.2 years, p<0.001) and were more likely to fall into the 1st (lowest) income quartile (25.8 vs. 20.9%, p<0.001) and less likely to fall into the 4th (highest) income quartile (23.1 vs. 28.5%, p<0.001) than elective surgery patients. Patients undergoing non-elective surgery had a greater proportion of Medicaid coverage (13.3 vs. 6.4%, p<0.001), and reduced private insurance coverage (37.2 vs. 47.3%, p<0.001) relative to elective patients. Relative to patients undergoing elective surgery, non-elective patients had a higher average Elixhauser comorbidity index (3.7 vs. 3.2, p<0.001), with higher rates of diabetes mellitus (13.6 vs. 11.6%, p<0.001), anemia (26.5 vs. 15.9%, p<0.001), and congestive heart failure (2.9 vs. 1.9%, p<0.001). Non-elective surgery patients were less likely to undergo robotic-assisted surgery (3.0 vs 4.1%, p=0.002) relative to elective patients, although there was no difference in the rate of open surgery (92.0 vs 92.4%, p=0.167).
Table 1: Demographic and Clinical Characteristics of Ovarian Cancer Patients Undergoing Elective Versus Non-Elective Surgery.
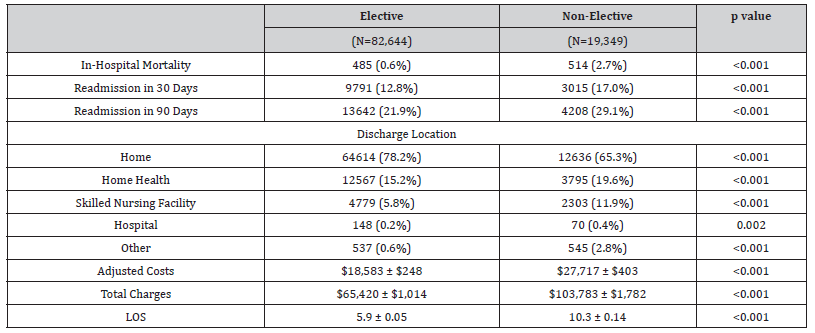
On univariate analysis presented in Table 2, patients presenting non-electively faced higher in-hospital mortality (2.7 vs. 0.6%, p<0.001), higher adjusted costs of index hospitalization ($27,717 vs $18,58, p<0.001), and greater LOS (10.3 vs. 5.9 days, p<0.001) at index hospitalization relative to elective patients. Non-elective patients were more likely to be discharged to a skilled nursing facility (11.9 vs. 5.8%, p<0.001) and were more likely to face readmission within 30 days (17.0% vs. 12.8%, p<0.001) and 90 days (29.1 vs. 21.9%, p<0.001).
Table 2: Post-operative Outcomes for Patient Undergoing Elective Surgery Compared to Non-Elective Surgery.
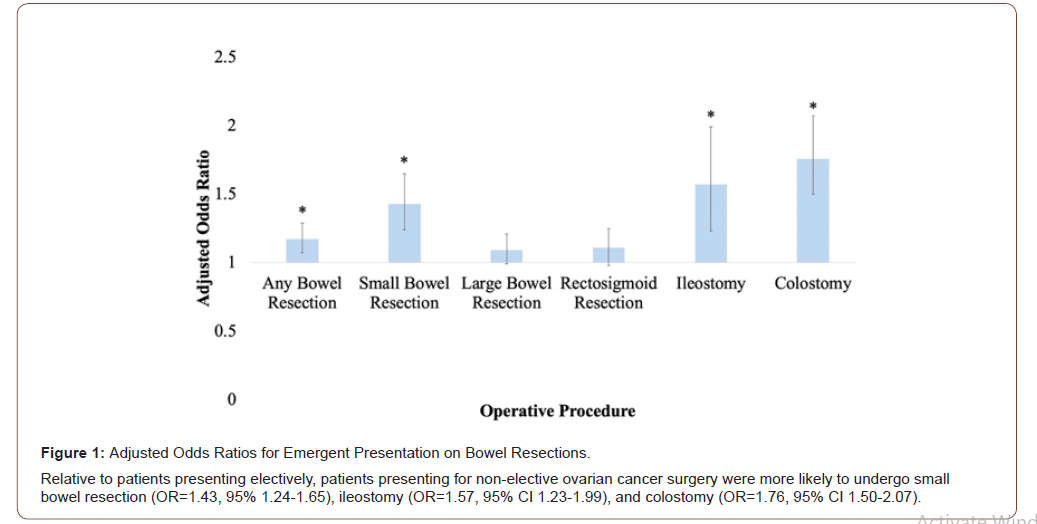
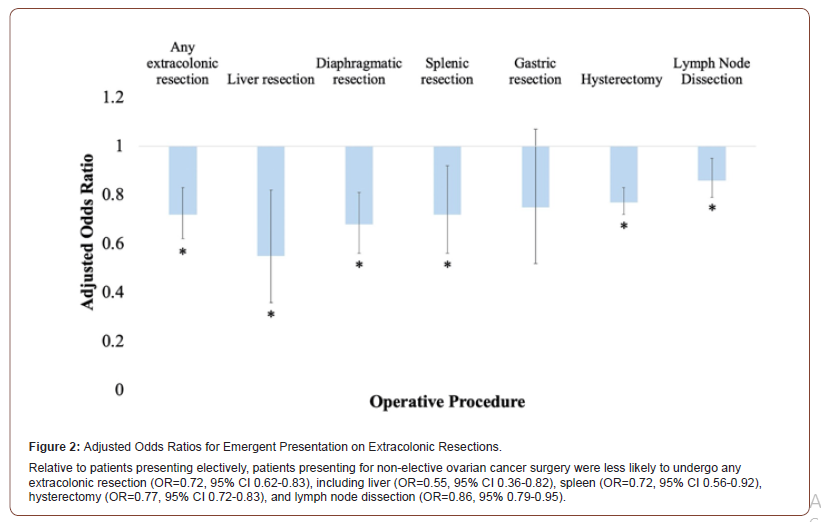
After controlling for baseline differences in demographics and comorbidities, logistic regression analysis revealed patients who underwent non-elective ovarian cancer surgery were more likely to undergo small bowel resection (OR=1.43, 95% 1.24-1.65), ileostomy (OR=1.57, 95% CI 1.23-1.99), and colostomy (OR=1.76, 95% CI 1.50-2.07) relative to patients presenting electively (Figure 1). Patients presenting non-electively were less likely to undergo any extracolonic resection (OR=0.72, 95% CI 0.62-0.83), including liver (OR=0.55, 95% CI 0.36-0.82), spleen (OR=0.72, 95% CI 0.56- 0.92), hysterectomy (OR=0.77, 95% CI 0.72-0.83), and lymph node dissection (OR=0.86, 95% 0.79-0.95) (Figure 2).
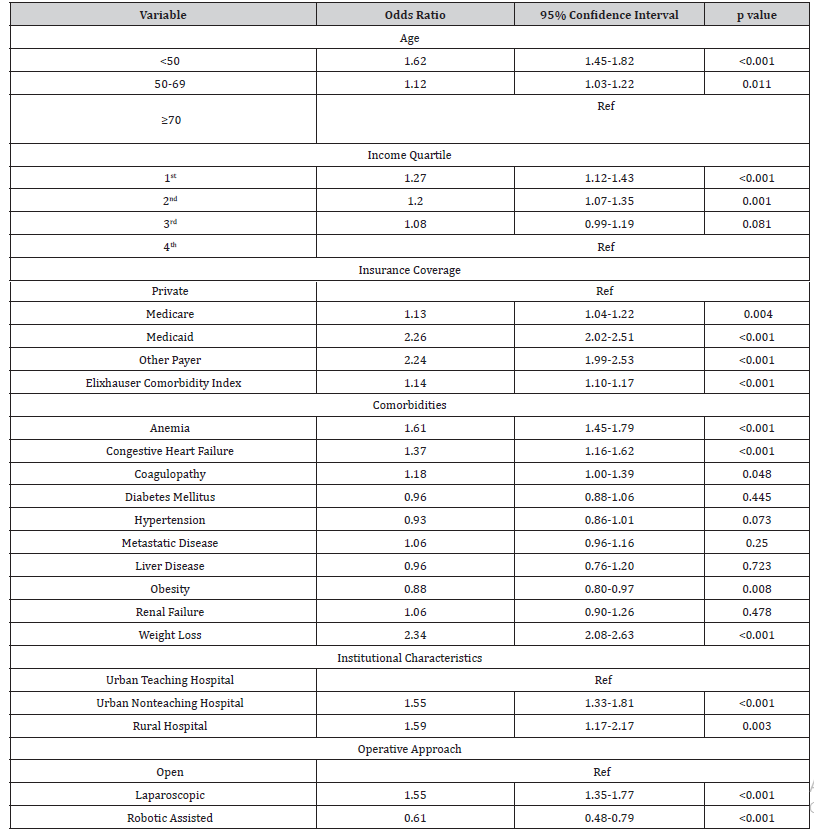
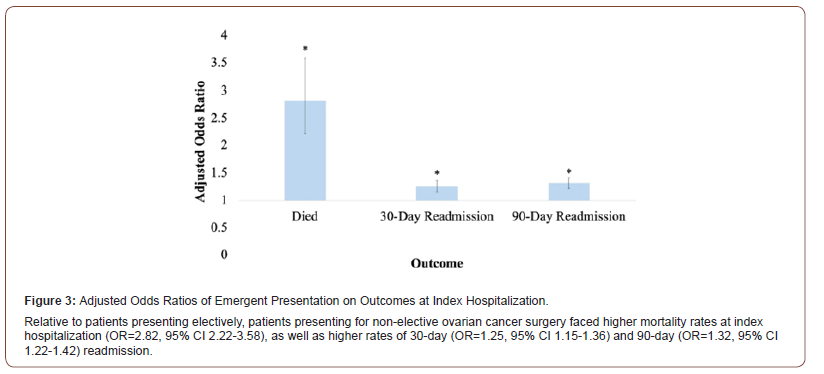
Logistic regression was used to analyze the association between demographic and clinical factors and the likelihood of undergoing non-elective surgery (Table 3). Admission for non-elective surgery was associated with age <50 relative to age >70 (OR=1.62, 95% CI 1.45-1.82), 1st (lowest) income quartile (OR=1.27, 95% CI 1.12-1.43) and 2nd income quartile (OR=1.20, 95% CI 1.07-1.35) relative to 4th quartile, and Medicaid insurance (OR=2.26, 95% CI 2.02-2.51) relative to private insurance (Table 3). Patients undergoing non-elective surgery were more likely to present to urban non-teaching hospitals (OR=1.55, 95% CI 1.33-1.81) and rural hospitals (OR=1.59, 95% CI 1.17-2.17) relative to urban teaching hospitals. Comorbidities associated with non-elective presentation included significant weight loss (OR=2.34, 95% CI 2.08-2.63), anemia (OR=1.61, 95% CI 1.45-1.79), and congestive heart failure (OR=1.37, 95% CI 1.16-1.62). With multivariable analysis adjusting for baseline differences in demographics and comorbidities, non-elective surgery was associated with higher mortality at index hospitalization (OR=2.82, 95% CI 2.22-3.58), and higher readmission rates at 30-days (OR=1.25, 95% CI 1.15- 1.36) and 90-days (OR=1.32, 95% CI 1.22-1.42) (Figure 3). Patients undergoing non-elective surgery spent on average 3.3 more days in the hospital [95%CI: 3.0-3.5]) with $6,188 more in costs [95% CI: $5,497-$6,879] for the index hospitalization.
Table 3: Logistic Regression Analysis of Factors Associated with Non-Elective Surgery.
Discussion
Our study aimed to better characterize the population of patients with ovarian cancer presenting for non-elective surgery. In our analysis of 101,993 patients undergoing ovarian cancer surgery, 19,349 (19.0%) were classified as non-elective. Patients admitted non-electively were younger, more likely to have Medicaid insurance, low income, and more comorbidities than patients admitted electively. While patients undergoing non-elective surgery were more likely to undergo small bowel resection, ileostomy, and colostomy, they were less likely to undergo standard aspects of an ovarian cancer surgery including hysterectomy and lymph node dissection. These patients had longer hospital stays with increased adjusted costs, higher in-hospital mortality rates, and increased rates of readmission compared to patients admitted for elective surgery. Our findings are consistent with other studies that have evaluated non-elective surgery in the setting of suspected ovarian cancer. For example, in a population-based analysis of 5,475 Medicare patients in a Surveillance, Epidemiology and End Results (SEER)-Medicare linked database, Thrall and colleagues noted that 15.6% of patients presented for emergent surgical treatment, with 20.1% mortality for patients undergoing urgent or emergent surgery compared to 5.6% in patients who had planned, elective surgery [10]. While this study population represents women 65 and older, it similarly found that non-elective surgery was associated with worse outcomes.
In our large study, we observed patients presenting nonelectively were more likely to undergo bowel resections with establishment of an ileostomy or colostomy, but less likely to undergo more extensive extracolonic resections often observed in planned tumor debulking procedures for ovarian cancer. It is likely that these procedures were not performed by gynecologic oncologists and the intent of the surgery was stabilization of patients with acute presentation, rather than tumor cytoreduction, possibly in the setting of very advanced disease. Patients undergoing non-elective surgery for suspected ovarian cancer likely have more acute presentation due to severity of disease or inability to access care sooner. To account for potential confounding variables in our two cohorts, we controlled for various comorbidities and known markers of advanced disease such as weight loss. Additionally, considering that over 75% of ovarian cancer patients present with advanced disease [6], women with significant tumor burden make up the majority of patients who undergo elective and non-elective surgical intervention.
We found that low income and non-private insurance were significant predictors of non-elective surgical presentation. Patients within the bottom two income quartiles were more likely to have emergent or urgent surgery. These findings demonstrate that women of color, patients with public insurance, and lower income status are less likely to receive standard of care in ovarian cancer treatment and have worse outcomes [13-17]. A metaanalysis including 130,801 patients performed by Karanth and colleagues found that there was a 15% reduction in standard of care ovarian cancer treatment in women with lower socio-economic status (SES) compared to higher, as well as an increased risk in mortality for lower SES patients [17]. Increased likelihood for an emergent procedure may be a reflection of sociodemographic barriers preventing entry into a healthcare system, perhaps with only moderate vague symptoms, or lack of access to primary care services providing this type of evaluation.
Many studies have reported that increasing age is associated with decreased likelihood of standard of care treatment, increased emergent presentation, and worse outcomes. However, in many of these studies, age categories are inconsistently defined, relatively broad, or focused exclusively on older patients [10]. Díaz-Montes and colleagues found that patients greater than 80 years old had longer hospital stays, higher costs and high mortality compared to all patients less than 80 years old in an analysis of a state-wide discharge database [15]. In our study, we found that younger patients were actually more likely to present for emergent or urgent surgery. One reason this finding may have emerged is due to the construction of age categories in previous studies, or the emphasis on patients greater than 80 years old. According to the National Cancer Institute’s SEER Cancer Statistics, 17.5% of new ovarian cancer diagnoses are in patients aged 45-54, with 9.6% (approximately 1,342) annual deaths [1]. Based on our findings, younger patients, with low income, and publicly insured or uninsured patients, represent an important understudied population in ovarian cancer research. Prospective pathways to improve access to gynecologic primary care and dismantling barriers to entry for routine care in these patient populations may reduce the rates of sudden, severe, and non-elective presentation late in the disease course and ensure more equitable cancer treatment.
There are several limitations to this analysis, including those that are inherent to retrospective analysis of a national database. While the NRD contains a large, nationally representative sample size, it does not provide granularity regarding timeline of diagnosis and outpatient treatment regimens, including neoadjuvant or adjuvant treatment. Although the majority of ovarian cancer patients present with stage III or IV disease, the NRD does not provide information on the stage or grade of ovarian cancer, which further limits our assessment of the clinical context underlying these treatment decisions. The NRD does not code for patient race or ethnicity, limiting our ability to draw conclusions on racial disparities in this population. Finally, we are limited by the accuracy of coding and may only comment on trends and associations rather than establish causality. Nonetheless, we used statistical and coding best practices established by prior work in order to reduce the impact of such limitations.
In conclusion, using a large national database, we found that the rate of non-elective surgery in patients with ovarian cancer is high, with significantly increased patient mortality and resource utilization. Patients presenting for non-elective surgery are more likely to be younger, have lower income, and are more likely to have public insurance highlighting the urgent need to improve access and earlier entry into primary care. Further research should examine institutional-level data of patients presenting for urgent or emergent surgical intervention and further investigate possible interventions to prevent unplanned surgeries and hospital admissions for this patient population.
To read more about this article.....Open access Journal of Gynecology & Womens Health
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers





No comments:
Post a Comment