Authored by Amal Abd elsamea Elsokary*,
Summary
The study aimed to evaluate the value of management of placenta accrete using step by step approach using case series clinical study. This study was conducted on 74 pregnant females, who were selected to suffer from placenta accrete either diagnosed antenatal by MRI or Doppler U/S or both. Or diagnosed intraoperative .and the patients were excluded if the patient had previous four or more cesarean scars. Or If the patient is 40 years old or more.
The patients were submitted to steps by step approach for management of placenta accrete from step one to step five in order, but they will not proceed from any step to the next step except if this step fails to control the condition. The data from this approach regarding the duration of the step ,amount of bleeding ,units of blood used intraoperative ,any surgical complication, postpartum sepsis ,need of postpartum ICU were recorded.
This study enrolled 74 patients. six cases were found intraoperative to suffer from placenta percreta ,and 29 cases were found to suffer from placenta increte ,the range of preoperative and postoperative HB in non-complicated cases was 1-2.6gm (mean 1.628) and the range of no of needed units for intraoperative blood transfusion in non-complicated cases was 0-3 units (mean 1.04), the total operative time was range from 18-108 minutes (mean 46.08 minutes), 12 cases (16%) were complicated by bladder injury, 6 cases (8%) were complicated by uterine atony, 21 cases (28%) were complicated by sepsis, 9 cases (12%) needed ICU admission.
So, step by step approach should be used in management of placenta accrete as it has shorter operating time ,less intraoperative blood loss and shorter hospital stay ,it also has less intraoperative and postoperative complications despite being insignificant.
Keywords: Placentas accrete; Hysterectomy; Step by step; Bleeding
Introduction
Placenta accrete refers to an aberrant placental implantation as the anchoring villi invade to the myometrium, rather than being contained by decidual cells. There are many types of abnormally adherent placenta according to the degree of invasion of villi to the myometrium or to the serosal layer or extend beyond the uterus, but term placenta accretes collectively describe all of these [1].
The most important risk factors are placenta previa and prior uterine surgery, mainly cesarean section. So, the incidence of placenta accrete is increasing with the rising rate of cesarean section. It reaches about 25% to 50% incidence of placenta accrete in patients with placenta previa and prior cesarean delivery [2]. It is well noticed that the rate of placenta accrete in Egypt is high and increasing, yet there is no reported statistical data or documented study to evaluate the incidence of placenta accrete in Egypt . the most important actor for increasing rate of placenta accrete in Egypt is high rate of cesarean section in Egypt ,which also increasing [3].
Conservative management of the uterus turns into a surgical challenge in case of placenta accrete. Many surgeons tried many techniques including non-removal of the placenta and cut the cord short with postoperative methotrexate [4], resection of placental adhesion site also had been tried in selected cases [5], systematic devascularization of the uterus [6-8], transverse B lynch [9].
Stepwise technique had been developed in conservative management of placenta accrete ,and it passes through one step technique [10], two step technique [11] and reach to the simplest three step technique [12].
But placenta accrete is a potential emergency which couldn’t be managed by single technique or single approach. The authors think the condition mostly like postpartum hemorrhage which couldn’t be managed by single approach or single technique.
Also, conservative management of all cases is not possible and also non predictable, as every case has its own characteristics and its own randomly arranged placental vessels and the severity of adhesion cannot be diagnosed accurately except intraoperive.
So surgical management of placenta accrete couldn’t be managed by single surgical technique. And we suggest management begins with simple technique and if the condition is not controlled we proceed to another more complicated technique and so on to end with hysterectomy if not controlled.
Methods
Study design
Case series clinical study
Setting
This was conducted at tertiary care hospital (Department of Obstetrics and Gynecology of Tanta University- Egypt), in the period from October 1, 2017 to September 31, 2020.
Eligibility
This study was conducted on pregnant females, who were selected to suffer from placenta accrete either diagnosed antenatal by MRI or Doppler U/S or both. Or diagnosed intraoperative .and the patients were excluded if the patients:
• Had severe attack of bleeding before operation affecting patient’s general condition.
• Had previous four or more cesarean scars.
• was 40 years old or more
As in the last two conditions there is no need to expose the female to surgical hazard of conservation, and the safe surgical option for those patients is to perform hysterectomy without attempting to remove the placenta.
All patients selected for the study were counseled thoroughly about the procedure, its value and its hazards, written consent was taken from every patient.
If U/S and MRI suspected the presence of placenta accrete preoperative, then intraoperative the placenta was found to have normal adhesion to the uterine wall, this case was excluded.
Interventions
All patients in were submitted to the following surgical steps (each step doesn’t interfere with any other steps) in the following order, but they wouldn’t proceed from one step to the next step except if the previous step fails to control the condition.
Step 1:
1. Dissection of the bladder from anterior wall of lower uterine segment as much as possible
2. Transverse incision of the uterus at a higher level at upper border of placenta
3. Before fetal extraction ecbolic are administrated as oxytocin (syntocinon, Novartis) 20 IU i.e. infusion as a direct dose, methergin 0.1mg as maximum dose and rectal misoprostol up to 100 micrograms.
4. Extraction of the baby
5. Bilateral uterine artery ligation below the level of uterine incision
6. Removal of placenta, if there is line of cleavage total placenta removed or either piece meal according to the degree of placental invasion
7. Haemostatic quadruple sutures at lower uterine segment as many as the uterine wall could stand.
Step 2:
If step 1 failed known by difficult in removal of placental tissue or by still uncontrolled bleeding:
1. If the lower uterine segment is long enough, excision of wide part of lower uterine segment which may hold greater part of invaded placenta (segmental uterine wall resection)
Step 3:
If step 2 fails known by lower uterine segment is too short for application of step 2, or still uncontrolled bleeding:
1. Second bilateral uterine artery ligation below level of uterine incision and below level of first uterine artery ligature
2. Third Bilateral uterine artery ligation above the level of uterine incision.
3. Over sewing of placenta bed with sutures from outside the uterine cavity ,and other sutures may be taken intracavitary at the placental bed to control bleeding.
Step 4:
If step 3 failed known by still uncontrolled bleeding:
1. Insertion of intrauterine pack inside uterus with its lower end passing through opened cervix, the pack must be impacted in lower part of the uterus to ensure compression of placental bed
2. Closure of uterine incision only
3. observe the amount of vaginal bleeding, fundal level and vital measures of patient
Step 5:
If step 4 failed known by excessive vaginal bleeding, rising Fundal level or unsure vital measures for patient:
1. Total abdominal hysterectomy without oophorectomy after vaginal removal of the pack
Methods
All patients’ demographic data were taken, operation time (the duration of step 1 measured from the beginning of dissection of the bladder till the end of the step ether failed or succeeded ,then the duration of next steps measured later on), preoperative HB level, immediate postoperative HB level ,HB difference ,units of blood used intraoperative ,any surgical complication, any postoperative complications and postoperative hospital stay.
Outcomes of Study
primary outcomes include: (a) operation time (b) amount of bleeding known by HB difference
The secondary outcomes include: (a) amount of units of blood needed intraoperative for transfusion (b) intraoperative complications like (bladder injury, uterine atony) hysterectomy wasn’t considered as a complication as it was a part of the surgical steps, step 5) (c) postoperative complications like sepsis, need of ICU. (d) Duration of postoperative hospital stay.
Ethical Approval and Clinical Trial Registration
This study was approved by local ethical committee of Tanta University before the start of this study and registered on Pan African Clinical Trials Registry (pactr) under the code of PACTR201712002774233 All patients were informed about study design, interventions, and risks. All patients signed written consent. Privacy and security were maintained all over the duration of study.
There were no unexpected risks during the course of research.
Results
This study enrolled 74 patients who were assessed for eligibility. After selection according to inclusion and exclusion criteria for eligibility.
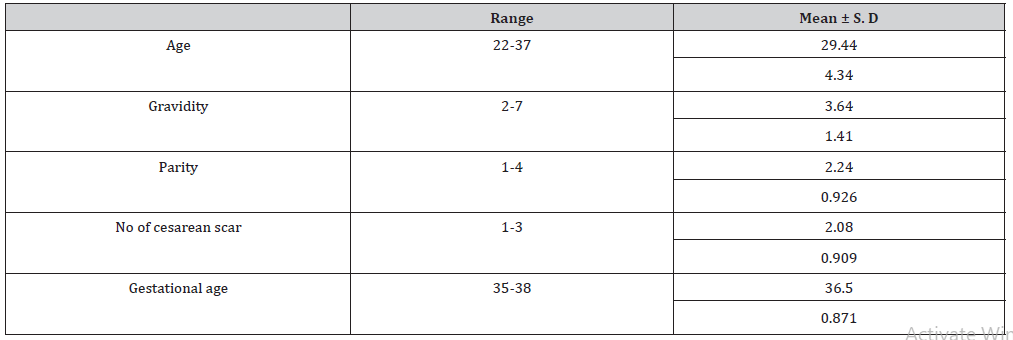
The mean age of selected patients was 29.44 and mean gestational age at time of cesarean section was 36.5 weeks gestation ,the whole demographic data of enrolled patients were demonstrated in Table 1.
Table 1: Shows distribution of cases according demographic data of selected patients.
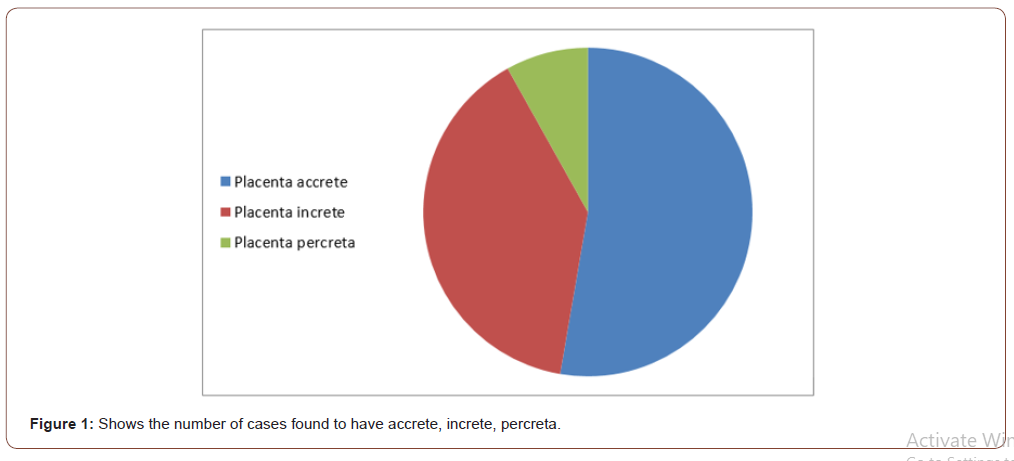
Only six cases were found intraoperative to suffer from placenta percreta ,and 29 cases were found to suffer from placenta increte ,and 39 cases were found to suffer from placenta accrete as shown in Figure 1
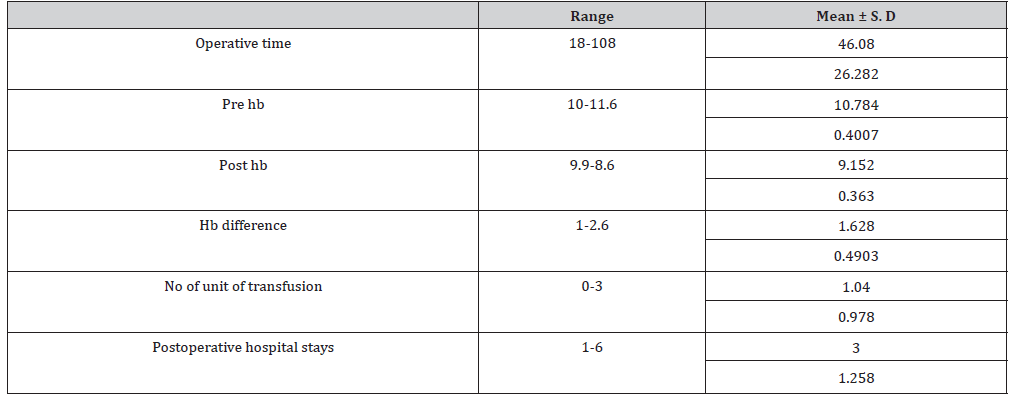
Regarding the operative data the range of preoperative and postoperative HB in non-complicated cases was 1-2.6gm (mean 1.628) and the range of no of needed units for intraoperative blood transfusion in non-complicated cases was 0-3 units (mean 1.04) ,it was noticed that 26 cases didn’t need intraoperative blood transfusion ,the range of postoperative hospital stay in noncomplicated cases was1-6 days (mean 3 days) as shown in Table 2.
Table 2: Show operative data of selected patients.
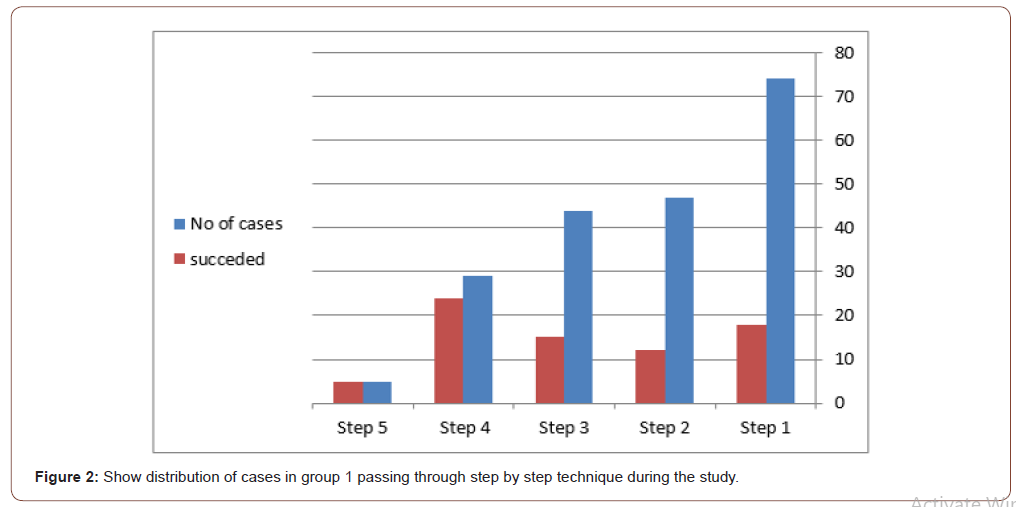
Studying the operative time for each step (step by step technique) ,it was found that from 74 cases was submitted to step 1 only 18 cases didn’t need further step the mean operative time was 18.84±1.97 min. ,from 47 cases submitted to step 2 (as 9 cases skipped this step) only 12 cases didn’t need further step the mean operative time was 5±1.032 min., from 44 cases was submitted to step 3 only 15 cases didn’t need further step the mean operative time was 18.266±3.411 min., from 29 cases was submitted to step 4 only 24 cases didn’t need further step the mean operative time was 25.8±1.813 min. the remaining 5 cases was submitted to step 5 ( hysterectomy step) with mean operative time was 35.5±7.778 min. as shown in Figure 2.
The total operative time was range from 18-108 minutes ( mean 46.08 minutes) as shown in table 2
Intraoperative complications, 12 cases (16%) were complicated by bladder injury and the urological team repaired them ,6 cases (8%) were complicated by uterine atony and the conservative management succeeded in each case ,but with the need of more units for blood transfusion (3-6units) and more decline of postoperative HB (2.6-4.5gm) . as shown in Table 3.
Table 3: Show intraoperative and postoperative complications of selected patients.
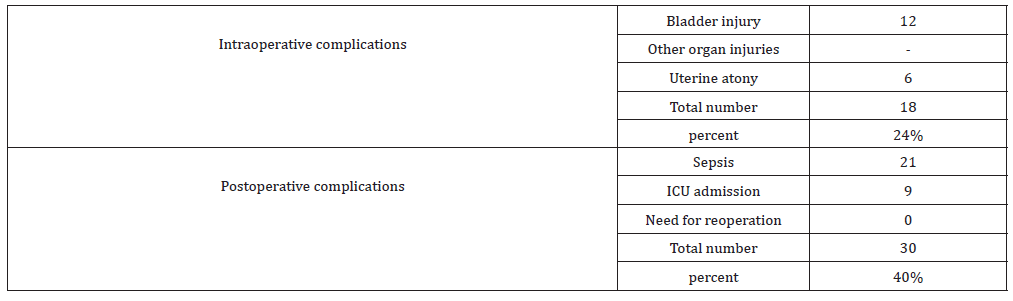
As regard Intraoperative complications, 12 cases (16%) were complicated by bladder injury and the urological team repaired them, 6 cases (8%) were complicated by uterine atony and the conservative management succeeded in each case ,but with the need of more units for blood transfusion (3-6 units ) and more decline of postoperative HB( 2.6-4.5 gm) . as shown in Table 3.
As regard postoperative complication, 21 cases (28%) were complicated by sepsis ,all of these cases were surgical skin infection ,and only 1 cases were complicated with pyometra ,which was managed by conservative treatment successfully (catheter drain, ecbolic and antibiotics), 9 cases (12%) needed ICU admission with longer stay at hospital (8-12 days ) as shown in table 3.
Discussion
Placenta accrete is considered a long term complication from cesarean section, with increasing incidence due to increasing rate of cesarean section [2], management of placenta accrete considered a surgical challenge to any obstetrician and shouldn’t be managed with single maneuver or single technique, it is more or less like any obstetric hemorrhage which should be managed with an ordered lines of interference taking in consideration that saving life of patient is a priority ,and the second priority is to conserve the uterus.
This study was case series clinical study.to study step by step approach for management of placenta accrete ,seventy four patients were enrolled in the study selected from women who attended Tanta university hospital –Egypt which is considered a tertiary hospital and referral hospital for difficult cases like placenta accrete.
Every steps (5 steps) in step by step approach could be done in every patient and not interfere with any of other steps ,the steps were ordered to jump from one step to the following step according to the patient condition until to reach to the final step which was hysterectomy step.
Sefa Kelekci, et al [13] tried a surgical procedure in conservative treatment of placenta accrete (uterine incision away from the placenta, bilateral ligation of The hypogastric arteries and uteroovarian anastomosis branches ,placental separation ,placental bed with squarely shaped suturing of placental bed and an inflated balloon of 3-ways 20F Foley catheter) it was a case series study on 12 cases only, their mean operation time was longer 110 ± 20 minutes (46.08 26.282 min in our study). And they needed more units of blood transfusion with a Median 4 (2–7) units transfused intraoperatively and postoperatively (1.04±0.978 intraoperative units in our study). The mean hospitalization time was longer also 4.2 ± 0.4 days (3±1.258) [13].
Zhu L, et al. [14] tried a modified suture to treat postpartum bleeding among patients with complete placenta previa (a Foley catheter balloon to compress the hemorrhage site and an absorbable suture was placed around the lower uterus segment). They measured amount of blood loss which wasn’t the case in our study but with no data about postoperative HB or needed units of blood transfusion .The median estimated blood loss during surgery was 1250 mL (range 1000-1500) for women with placenta accreta [14].
Palacios Jaraquemada, et al. [15] tried a technique for placenta percreta on a total of 68 patients (A retro vesical and parametrial dissection, Hemostasis with selective vascular ligature, the anterior wall defect was repaired using a suture, fibrin glue and polyglycolic mesh. Finally, a non-adherent cellulose layer applied over this reconstruction). 18 cases had failed conservative management by this technique (27%) compared by 5 cases in our study needed step 5 operation (6%) which also considered a part of our technique. Also, the high complications rate of the other 50 successful cases (13 case represent 26%) compared by low complication rate of our approach [15].
Shabana A, et al. [16] conducted a prospective observational study over 71 patients with placenta percreta; they were subjected to a stepwise surgical approach. this technique had similar results to our approach as it failed in only 6 cases (8.5%) compared by 5 cases in our study needed step 5 operation (6%) which also considered a part of our technique. Also, same result of bladder injury (14.1%, 16% in this study compared to our study respectively). But this technique needed more blood units intraoperative with a median 4U (1.04 unit in our study) and longer operation time 85 min (46.08 ±26.282 min in our study) [16].
Ansar A, et al. [11] studied outcome of interval (delayed) hysterectomy as compared to cesarean (immediate) hysterectomy in cases of placental invasion in previous cesarean sections on 28 women, it was noted that in both group of patients in this study they needed larger volume of blood transfused (9.76 vs. 2.9) and longer hospital stay (10.69 vs. 32.86 days) and even One maternal death occurred in each group. And this can justify the benefits of our approach as making hysterectomy decision at a proper time without delay to preserve life and health of patient [11].
Iwata A, et al. [17] found that there were no benefits from internal iliac ligation as a bleeding control during cesarean hysterectomy for placenta accrete. Among 23 cases, as the mean blood loss during the operation and the length of hospitalization after the operation, with or without internal iliac artery ligation (IIAL) were not significantly different [17].
Li GT, et al. [18] assessed the efficacy and safety of longitudinal parallel compression suture to control heavy postpartum hemorrhage (PPH) in patients with placenta previa/accrete among Fifteen women, the failure rate of this procedure was 13.3% compared by 5 cases in our study needed step 5 operation (6%) which also considered a part of our technique [18].
Teixidor Viñas M, et al. [19] evaluated the Triple-P procedure involving placental non-separation, myometrial excision and reconstruction of the uterine wall among 30 patients the Estimated mean blood loss during the procedure was 2.17 L. but postpartum hemorrhage occurred in 15.8% of cases compared by 8% in our study complicated by uterine atony, but in their study 0% of cases needed hysterectomy and this may be attributed to only 13 cases proved to have placenta accrete intraoperative from 30 cases [19].
Xuhua Duan, et al. [20] had studied the effect of intermittent aortic balloon occlusion during CS, it was found that less blood loss (597±359 mL) less transfusion requirements (498±195 mL), no cases needed hysterectomy from 22 cases subjected to this procedure, they had a similar operation time (63.8±12.3 min) and similar rate of complications, but this method need high equipment and availability of C-ARM in the operation theater [20].
Dawood AS, et al. [21] had a retrospective study where the files of 91 cases of placenta accrete managed by three-step technique were reviewed ( bilateral uterine artery ligation ,homeostasis of lower uterine segment t then use of balloon of triple way Foley’s catheter) The technique failed in only 5% of cases to conserve uterus and similar hospital stay (3.065±1.04 days) in our study hospital stay was (3±1.258 days). And also, low rate of complications, but this technique had a longer mean operative time (81.65±15.68 min.) compared to our study (46.08±26.282 min) [21].
Shih JC, et al. [22] had studied ‘Nausicaa’ compression suture in case of postpartum hemorrhage in general, and in the course of his study 43 cases were suffering from placental adhesive disorders, so it was difficult to interpret the results as 25 cases also were not suffering from placenta adhesive disorders, but no case needed hysterectomy in his their study [22].
Conclusion
Step by step approach should be recommended in management of placenta accrete as it has shorter operating time ,less intraoperative blood loss and shorter hospital stay ,it also has less intraoperative and postoperative complications.
Step by step approach organize the effort for management of placenta accrete taking in consideration that the first priority is to save life of patient and make the decision of hysterectomy timely proper not delayed or rushed, and more organized.
To read more about this article.....Open access Journal of Gynecology & Womens Health
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers





No comments:
Post a Comment