Authored by Yazan Kadkoy*,
Abstract
Pigmented villonodular synovitis (PVNS) is a subtype of tenosynovial giant cell tumor. Such tumors are rare and locally aggressive, though benign, with an average annual incidence between 1.8 and 9.2 cases per million in the U.S. [1] This low incidence of disease makes clinical trials difficult to conduct. Clinically, PVNS is separated into localized (LPVNS) and diffuse (DPVNS) disease. Surgical options include open, arthroscopic and combination arthroscopic/ open approaches for disease involving both anterior and posterior compartments of a joint. Despite surgical resection being the most common treatment modality for PVNS, recent medications have been developed targeting the colony stimulating factor 1 receptor (CSF1R) pathway.[2] In our case series, we selected 53 patients meeting inclusion criteria and treated between 2002-2019,
(29) with DPVNS and (24) with LPVNS. Patients were first categorized by the local or diffuse subtypes of disease, followed by anatomic location anterior, posterior, or both. Surgical treatment method was stratified by the following categories: (1) mini open incision (<4cm) (2) arthroscopy (3) arthroscopy with open incision
(4) open. Mean follow up was 33months ±12months. Open synovectomy was utilized for 23 patients (79%) with DPVNS and 5(21%) patients with LPVNS. Nine patients (38%) with LPVNS and 1(3%) patient with DPVNS underwent arthroscopic synovectomy. Patients treated with open synovectomy had significantly larger tumor volume (196.1+/-311.0 cm3 vs. 42.7+/- 64.6 cm3; p=0.0350). For the diffuse treated group 3/5 treated arthroscopically assisted and 8/23 treated open recurred. The overall rate of recurrence was 37% for DPVNS, and 4% for LPVNS. Further analysis revealed significantly higher rate of recurrence in patients with DPVNS (OR 15.1; p=0.002). Additionally, infection rates were similar for diffuse versus localized disease at 6% versus 5% respectively. The overall complication rate for patients treated with open synovectomy was 38% which was significant (OR 5.2; p=0.019)
Keywords: Pigmented; Villonodular; Synovitis, LPVNS, DPVNS
Abbreviations:
PVNS: Pigmented villonodular synovitis
LPVNS: Localized pigmented villonodular synovitis
DPVNS: Diffuse pigmented villonodular synovitis
CSF1R: Colony stimulating factor 1 receptor
Introduction
Pigmented villonodular synovitis (PVNS) is a subtype of tenosynovial giant cell tumor characterized by the presence of synovial stromal and fibroblast cell proliferation, hemosiderin deposition, and multinucleated giant cells. PVNS most commonly affects the knee, and typically presents with swelling and discomfort of the affected joint. [3] Such tumors are rare and locally aggressive, though benign, with an average annual incidence between 1.8 and 9.2 cases per million in the U.S. [1] This low incidence of disease makes clinical trials difficult to conduct. Clinically, PVNS is separated into localized (LPVNS) and diffuse (DPVNS) subtypes. The localized form is nodular and can be found in and around the joint. [4] The diffuse form affects the entire synovium and invades extraarticular structures such as muscle and tendon. [5-8] This distinction is useful for determining management, with open surgical resection being the gold standard for DPVNS. Synovectomy can be performed arthroscopically, open, or with a combination of both. [9-12] post- operative goals include maximizing knee function through preserving structures, while limiting rate of recurrence with a thorough debridement. Despite surgical resection being the most common treatment modality for PVNS, recent medications have been developed targeting the colony stimulating factor 1 receptor (CSF1R) pathway. Use of these medications as well as tyrosine kinase inhibitors have shown promise in the treatment of recurrent disease or that which is refractory to surgical intervention [2].
The goal of this study was to further elucidate outcomes of operatively treated PVNS with arthroscopy, open surgical resection, or a combination of both. We hypothesize that DPVNS will have a higher incidence of recurrence and complications when compared to LPVNS.
Materials and Methods
After acquiring an IRB approval, a retrospective review of records from a single institution was performed with records dating from 2002-2019. The main inclusion criteria consisted of patients that underwent surgical excision of PVNS or nodular synovitis that was localized to the knee. A cohort of 53 patients that met the criteria was selected, (29) with DPVNS and (24) with LPVNS. Patients were then categorized by the local or diffuse presence of PVNS, followed by anatomic location anterior, posterior, or both. Surgical treatment method was stratified by: (1) mini open incision (<4cm) (2) arthroscopy (3) arthroscopy with open incision (4) open, regarding the anatomical location and diffuse versus local nodular PVNS.
Patient data was collected for age, gender, tumor volume, overall complication rate, recurrence rate, and infection rate. Nonparametric analysis of categorical information was performed using a chi-square test, unless an expected value was less than five, in which case Fischer’s exact test was utilized. Odds ratios were generated with computation of confidence intervals utilizing the Baptista-Pike method. Non-parametric analysis of continuous variables was performed using a Mann-Whitney U test. All analyses were performed using GraphPad Prism version 7.00 (GraphPad Software, La Jolla, California, USA, www.graphpad.com). In all tests, significance was set at p < 0.05.
Results and Discussion
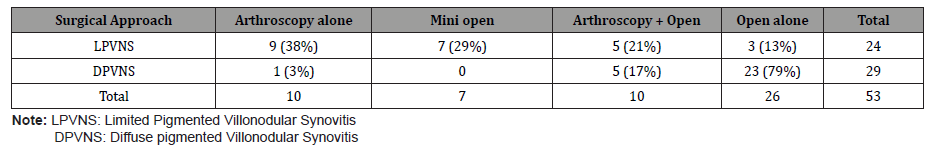
From 2002-2019, we found 53 patients who underwent open, mini-open, arthroscopic, or combination synovectomies for PVNS. Mean follow-up was 33months ±12months. Mean patient age was 42.0 (SD 14.1) years with 39 female and 14 males. Of these, 24 patients were diagnosed with localized disease and 29 with diffuse disease. The mean tumor volume was 18cm3 for localized and 228cm3 for diffuse. Anatomic location also varied, as 28 patients had anterior disease, 9 had posterior disease, and 16 had disease anteriorly and posteriorly. For LPVNS, 9 (38%) were treated with arthroscopy alone, 7 (29%) with mini open, 5 (21%) with arthroscopy and open, and 3 (13%) with open alone. This is in contrast to DPVNS where 23 (79%) were treated open, 1 (3%) with arthroscopy, and 5 (17%) with a combination of anterior arthroscopy, and posterior synovectomy. (Table 1) It should be noted that patients with localized, single compartment disease were treated arthroscopically unless the lesion was too large to be removed as a single piece in which case a mini open incision was made to assist with removal from the joint.
Table 1:Surgical intervention breakup by disease type.
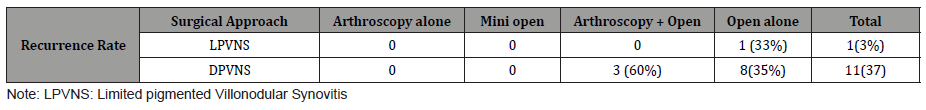
Recurrence, infection, and complication rates were also analyzed. For LPVNS the recurrence rate was 1 (3%), which occurred in the open treated group. For the diffuse treated group 3/5 that were treated arthroscopically assisted and 8/23 that were treated open recurred. The overall rate of recurrence was 37% for DPVNS, and 4% for LPVNS. There were no recurrences seen on the arthroscopy alone, and mini open groups for localized or diffuse disease. It should be noted that no patient with DPVNS was treated with mini open and only one patient with DPVNS was treated with arthroscopy alone. Further analysis revealed significantly higher rate of recurrence in patients with DPVNS (OR 15.1; p=0.002). (Table 2) Patients who suffered recurrence had a higher mean tumor volume than patients without recurrence (57.5±93.9 versus 139.8±166.9; p=0.039). Additionally, infection rates were similar for diffuse versus localized disease at 6% versus 5% respectively. The overall complication rate for patients treated with open synovectomy was 38% which was significant (OR 5.2; p=0.019). The largest complication was related to local disease recurrence
Table 2:Recurrence rate by surgical intervention and disease type.
After a review of the recent literature, recurrence rates of arthroscopic versus open synovectomies were analyzed. A large multicentered cohort study on the surgical treatment of LPVNS found a recurrence rate of 12% and a complication rate of 4% among 941 treated patients. This same group also demonstrated a recurrence rate of 44% and a complication rate of 12% amongst 906 patients with DPVNS. [13,14] These rates are similar to the rates observed in our case series.
As seen in our study and described in prior studies, the variability in presentation of and lack of a standardized approach to PVNS leads to challenges in analyzing outcomes following treatment. Overall, patients with localized disease at the anterior knee did well with both a mini-open incision and with arthroscopy. Frequently in these cases, arthroscopy was first performed with the occasional need to make a mini-open incision to sufficiently remove the entirety of resected synovium as a unit. In cases of diffuse disease both anteriorly and posteriorly, treatment decision-making becomes more complex and diverse.
Caution should be taken with choosing combined treatment of arthroscopic synovectomy anteriorly followed by open treatment of posterior PVNS, due to the high (67%) rate of recurrence. Despite this, a diagnostic arthroscopy may aid in thorough localization and detection of disease prior to synovectomy.
Tumor volume plays a substantial role in evaluating recurrence risk, regardless of treatment performed. However, readers must be cautioned against strict interpretation of this finding, as patients with larger tumor volume are more likely to have diffuse disease, inherently increasing their risk for recurrence. However, within the subgroups of open and arthroscopic treatment, patients with larger tumor volumes had a higher recurrence rate. Unfortunately, this study lacks sufficient power to determine a “cutoff” tumor volume for which patients could be treated successfully with arthroscopy alone.
Conclusion
PVNS remains a difficult condition to manage and treat. The low incidence makes it difficult to perform clinical trials. DVPNS poses a greater challenge for treatment given its higher likelihood to invade locally as well as the higher incidence of recurrence when compared to localized disease.
In our series, diffuse disease, which we defined as tumor in multiple compartments of the knee, had a high correlation with large tumor volume. We treated this either open or with an anterior arthroscopic debridement and posterior open synovectomy. Here, surgical intervention correlated to the overall size of tumor, with large tumors being treated open. The purpose of utilizing arthroscopy was two- fold: (1) decrease the injured structures, and (2) minimize arthropathy. Despite the rationale for choosing a given surgical intervention, the rate of recurrence and complication remained the same for all patients with DPVNS.
There were several limitations to this study. Given the retrospective nature of this case series we were not able to formally assess functional outcomes for patients after surgical intervention. Additionally, our average follow-up time of 33 months may have been too soon to detect disease recurrence.
Given these results, we offer an algorithm for synovectomy. LPVNS should be treated either arthroscopically or with a mini open. DPVNS should be treated open or in a combined approach, which ever minimizes disruption of surrounding structures and allows for faster return to baseline function; however, use of arthroscopy comes with an increased risk of recurrence. This should also come with an understanding that the likelihood of recurrence is high. Future studies will look to assess the impact of novel biologics on the recurrence rate of disease as well as try to further elucidate a more concise protocol for the treatment and management of disease.
To read more about this article...Open access Journal of Rheumatology & Arthritis Research
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers





No comments:
Post a Comment