Authored by Mohammad AA Al-Najjar*,
Abstract
The human eye is an organ that is exposed to the environment continuously, which makes the ocular surface subjected to different types of pathogenic and non-pathogenic microorganisms. Different types of microorganisms can be found naturally in each layer of the eye, such as the Grampositive bacteria (i.e., the Coagulase-negative staphylococci including S. epidermidis and Bacillus sp), the Gram-negative bacteria (as Pseudomonas sp. including P. aeruginosa) and fungi. Apparently, bacteria are considered to be the major causative agent of ocular infections that are believed to be a global problem. Unfortunately, Ocular infections, if left untreated, may lead to damage in the structure of the eye with possible complications such as blindness and visual impairments. Scientists highlighted the importance of studying the ocular microbiome, which indeed has been accelerated recently. In this review, we aim to overview ocular microbiota and the factors that may affect it, the diagnosis of ocular infections, and the available treatment so far.
Keywords: Eye microbiota; Gut microbiota; Eye infection
Eye Microbiota
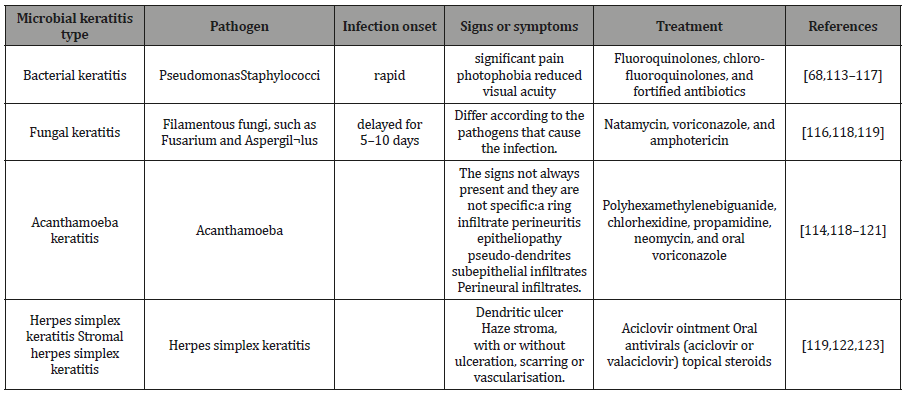
The human eye is a very complex organ which consists of three layers: tear film, lacrimal glands, and eyelids [1–3]. The outer section consists of the cornea and the sclera, where cornea protects the eye against infection [3]. The ocular surface is frequently exposed to the environment and to different types of microbes starting from birth time and throughout life. If a swab was taken from different parts of the ocular surface, many types of microbes can be isolated and examined by culture [4,5]. Interestingly, the microbial composition could be (i) gram-positive bacteria such as Staphylococcus aureus and staphylococciepidermidis, (ii) gram-negative bacteria such as Pseudomonas aeruginosa, and [4,5], (iii) fungi such as Aspergillus spp, Curvularia sp., Penicillium sp., Helminthosporium sp., Candida albicans, C. guilliermondii, C. parapsilosis, Saccharomyces cerevisiae, Hormodendrum sp., and Rhodotorula rubra [6–9] (Table 1 & 2).
Table 1: The tablet is a summary of the Ocular microbiota of conjunctiva, eyelid, and tears, adopted from [4-10].
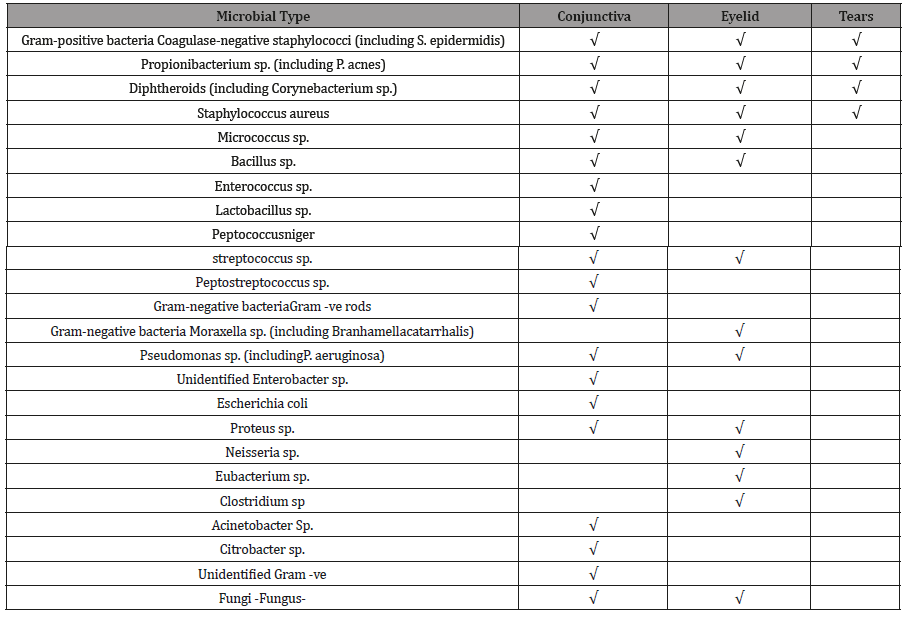
Table 2: Clinical features of keratitis types.
Effect of The Gut Microbiome on Ocular Disease
Relevant to ophthalmologist’s studies, gut bacteria can influence immunity at distant sites, including the eye. Some ocular conditions have been associated with gut microbiome abnormalities including Sjögren’s associated dry eye, glaucoma, and macular degeneration. Patients have infectious keratitis, Patients with bacterial keratitis had higher relative abundances of Proteobacteria and Firmicutes in the gut comparing them with healthy individuals [11].
Dry eye
Sjögren’s is a disease caused by lymphocytic infiltration of the lacrimal and salivary glands disorder which as consequence will cause dry eye and mouth [12]. Studies demonstrated that commensal bacteria variation in the gut provokes a worse dry eye phenotype, while the normalization of the improvement of the microbiome can cause improvement in the dry eye phenotype [13,14].
Autoimmune uveitis
The results of studies were done on patients with posterior segment uveitis have shown that these patients have gut microbiome disturbance [15,16]. Compared to healthy individuals there were increased abundances of Fusobacterium and Enterobacteriaceae [17]. This alteration in the commensal gut bacteria believed to alter the immune privilege status of the eye and thus prompted toward uveitis. A series of actions potentially relate the microbiome to uveitis; consist of loss of immune tolerance to commensal microbiomes increased inflammation and permeability of the gastrointestinal tract and translocation of microbial antigens to extraintestinal sites such as the eye [15,16,18].
Glaucoma
Studies investigated the link between the microbiome and different sub-types of glaucoma, as they revealed that alterations of gut microbiome were related to primary open angle glaucoma (POAG). This infection was correlated with the raise abundance of Bacteroides and Prevotella [19,20].
Age-related macular degeneration (AMD)
Age-related macular degeneration (AMD) is a deactivating eye condition that affects the slow decrease of central visualization [21,22]. This eye disorder influences a central part of the retina well-known as the macula, which controls critical central vision that is necessary for daily actions as reading, watching television, driving and facial recognition. Even though AMD does not normally indicate to absolute loss of sight (peripheral vision is retained), failure of central vision possibly will have the main effect to an individual’s conventionality and value of natural life [23]. Although in this disorder the exact pathogenesis of AMD is poorly understood, it is believed to be an inflammatory component related to innate immunity. These inflammatory pathways consist of complement and Toll-like receptors, pathways adjusted by the microbiome [17].
Stages of AMD: AMD has three stages all of which will appear in the eye retina. The early AMD in which the size of drusen is medium and the patient vision will not be lost. In the intermediate AMD, the drusen size will be larger; this stage is asymptomatic although the patient may have an abnormality in the retinal pigment. The last stage is the late AMD, which is characterized by having two types the wet AMD and the dry AMD, and at this stage, the size of drusen is large too but the patient may loss his central vision [23]. Patients with neovascular AMD had to gut microbiota that was supplemented with Anaerotruncusspp., Oscillibacter spp., Ruminococcus torques, and Eubacteria ventriosum, whereas the microbiota of a healthy person was dominated by Bacteroideseggerthii. The latter microorganism could be a defensive anti-immune-mediated disease, which could be due to the variations in bacterial genes associated with type of metabolic pathways. Especially those involving the diminished amount of genes included in fatty acid elongation and supplementation of genes associated with L-Alanine fermentation, glutamate degradation, and Arginine biosynthesis [24].
Preventive treatment of AMD: There has been wider agreement on the relevance of food supplements (i.e., vitamins) in the improvement and restriction of AMD. For example, antioxidant and mineral supplementation may be used in early and intermediate AMD [25]. These supplements, such as vitamin E, may contain (α-tocopherol) and C (ascorbic acid), zinc, glutathione, and especially macular carotenoids, such as lutein and zeaxanthin [26–28]. Recently studies have discussed that lutein and zeaxanthin may be more effective in the suppression of lipofuscin pigments photo-oxidation than α-tocopherol because they have the capability to quench singlet oxygen. This represents a potential protective effect for these two-component against harmful photo-oxidative processes proceeding in the path of lipofuscinogenesis with its impact on AMD development [28,29].
Effect of Ocular Diseases on the Ocular Microbiota on the Eye
Previous studies demonstrated that the surface eyes microbiota has a vital role and it may affect the local immune response and pathogenesis. Thus, many eye disorders can be caused if there was any imperfection in the microbiota [24].
Eye microbiota and contact lenses
Contact lenses, which worn on either daily disposable, daily wear or extended wear bases, usually made of many different types of polymers such as polymethyl methacrylate (PMMA) [30], hydroxyethyl methacrylate (HEMA) [31], or the silicone hydrogel materials [32]. Contact lenses are considered to be a risk factor for infection. Several studies were done in order to determine the types of microbiota isolated from contact lenses after wearing them especially their effect on the microbiota of the conjunctiva and lids [33].
The most isolated microbes from contact lenses after wear are coagulase-negative staphylococci, Propionibacterium sp. and Corynebacterium sp. Almost no difference was noticed on the eye microbiota when comparing the effect of different types of polymers and the wear schedule [5,34-38]. Even when examining the effect of long term extended wear of HEMA-based lenses, the results showed that this type of polymers did not change the conjunctiva or lid microbiota. However prolonged wearers were more commonly colonized on these two surfaces by pathogenic microbes that have the capability to cause infection (such as Gram-negative bacilli). Nevertheless, daily wear of HEMA-based lenses was associated with an increase in colonization incidence of the conjunctiva and lids by bacteria such as coagulase-negative staphylococci [39].
A new study shows that the eye microbiota of lens wearers is different from that of non-wearers. According to the result of cultures from contact lenses, the presence of Staphylococcus, Propionibacterium, Corynebacterium, Bacillus, Micrococcus, Rothia (previously assigned to Stomatococcus)[35,39–45], and Pseudomonas have been reported [46–48] .In more than half of the sample, the relative abundance of some “taxa” in contact lenses was detected was 1%. Streptococcus [49], Methylobacterium, and Acinetobacter, and members of families Oxalobacteraceae and Enterobacteriaceae were detected in these samples [50]. On the other hand, some studies state that the use of contact lenses does not change the ocular microbiota; due to the use anesthetic eye drops such as topical proparacaine hydrochloride anesthetic before sampling, which may decrease the detected ocular microbiota diversity. Usually, this topical anesthetic may cause dilution of the bacteria or be washed away from the ocular surface [50].
Contact lenses effect on eye bacterial biofilms: Biofilms are defined as a community of bacteria held together by a polymeric extracellular matrix [51-54]. They provide a defense mechanism against the environmental stress, antimicrobial agents, the host immune cells, and the invasion by other microorganisms. Contact lenses and the placement of intraocular lenses, which are two procedures used to manage those eye abnormalities and vision problems, provide the bacteria with a new surface on which many pathogens can form biofilms[51-53,55].Unfortunately, many types of bacteria that can form biofilms may lead to poor visual outcomes and occasionally loss of sight. Examples of these infections are acute bacterial endophthalmitis and corneal ulceration. Endophthalmitis infection is caused by Coagulase-negative staphylococci and Propionibacterium acnes and it can affect patients who intraocular lens and posterior capsules [56–64]. Keratitis which frequently may affect patients who use contact lenses caused by Staphylococci, Pseudomonas spp. [65–67], Fungi Acanthamoebaless [68].
Infectious diseases associated with contact lenses: Contact lenses use has been recognized as a risk factor for the development of eye infections such as giant papillary conjunctivitis and keratitis [69,70]. Tearing and the corneal epithelium are inherent protective mechanisms to protect the eye from the pathogenic microorganisms. The tear fluid and blinking remove pathogens from the cornea [71–73]; moreover, it contains antimicrobial components such as lysozyme and lactoferrin. In addition, the epithelial cells produce innately antimicrobial peptides and mucins [74], and their tight junctions work as a physical barrier to microbes [71,72,75]. Nevertheless, Contact lens wear disrupts some of these innate defenses and renders the cornea more susceptible to infection [76].Contact lens wear has also been shown to change the corneal epithelium, to carry organisms to the ocular surface and to limit natural clearance mechanisms [77,78]. In addition, biofilms which are less susceptible to the normal antimicrobials defense mechanisms of the tears will be formed on the posterior contact lens surface place bacteria close to the epithelium [75,78]. The contact lenses will cause mechanical damage of the epithelium, punctate epithelial erosions, and reduced tear exchange [79–82]. Microbial keratitis (MK), which is the most an ophthalmic emergency visionthreatening disease and severe complication [83], is a broad term that includes bacterial keratitis (BK), fungal keratitis (FK), and Acanthamoeba keratitis (AK) [84,85]. The MK in contact lens wearers is usually related to some risky behaviors owing to the “noncompliant “or bad hygienic practices [83,86]. However, daily disposable lenses do not reduce the risk of MK though; the use of this type may be a lower risk of vision loss when compared with the other type [87,88].
Bacterial keratitis: The bacterial infection is the most frequent cause of infectious keratitis. Usually, the underlying types of bacteria involved in the infection are staphylococci, Streptococcus pneumoniae, and Pseudomonas spp [89,90] Patients can experience pain, photophobia, blurred vision, corneal cloudiness or pus inside the eye [91]This type of infection can be treated with topical antibiotics include monotherapy of fluoroquinolones or combination therapy of aminoglycoside/cephalosporin [92,93].
i. Fungal keratitis: Fungal keratitis, which occurs because of Filamentous fungi, such as fusarium and Aspergil¬lus tend to be most often related with contact lens wear and trauma, [94,95], while those with the ocular surface disease are more prone to yeasts [96]. Fungal biofilms are the expected cause of Contact lens-related Fungal Keratitis, where the fungi can be strongly attached to the posterior side of the lens or extend into the lens matrix [97]. The clinical appearance of Fungal Keratitis depends on the causative pathogens. Corneal infections due to Candida often similar to Bacterial Keratitis [98].However, mycotic keratitis that is associated with Feathery borders, satellite lesion, and necrotic slough is due to Fusarium or Aspergillus[99].The management Fungal keratitis includes the use of antifungal agents such as Natamycin, voriconazole, and amphotericin [100].
ii. Viral keratitis: Herpes simplex keratitis can be classified according to the layer involved to epithelial, stromal, endothelial or mixed, epithelial herpes simplex characterized with a dendritic ulcer [101], and it typically can be treated with acyclovir ointment; however, at the early stage of the herpetic epithelial keratitis topical corticosteroids should be avoided[102]. On the other hand, endothelial keratitis is characterized by the presence of keratitis precipitates on the endothelium and corneal edema, while cloudiness Stromal herpes simplex keratitis characterized by the presence of cloudiness of the stroma, with or without ulceration, scarring or vascularization [101,103]. In the case of the stromal and endothelial keratitis, the treatment would be oral antivirals (acyclovir or valaciclovir) [102,104,105].
iii. Parasitic keratitis: Contact lens-wearing individuals who expose their lenses to water through swimming, hot tubs, trauma with contaminated water, or care for their lenses with water are at greater risk of infection [106]. The largest risk factor for contact lens-related AK is poor compliance with lens care which leads to subsequent biofilms formation [106,107].The signs of this infectious disease not always present and they are not specific but some signs such as a ring infiltrate perineuritis, epitheliopathy, pseudodendrites, subepithelial infiltrates and Perineural infiltrates may indicate the patient has the Acanthamoeba keratitis [108,109]. This type of keratitis can be treated with polyhexamethylenebiguanide, chlorhexidine, propamidine, neomycin, and oral voriconazole [69,108–112].
Ocular Infections
Infectious conjunctivitis
Conjunctivitis is the most events that reasons for the expansion of the conjunctival blood vessels and causes in inflammation. In which one or both eyes become red or pink and might be sticky or watery [124,125]. Method to detect and treats conjunctivitis, according to the signs and symptoms. Evaluation should involve examination visual perception and investigation with a torch or lamp. Fluorescein droplets must the conjunctival sac and the eye observed with the cobalt blue light of the fundoscopy, to investigate out any signs of corneal ulceration or infection. Cold sores should be searched for and the patient observed for cold sores or a vesicular rash incident the infection is due to herpes simplex or zoster virus [125,126].
Bacterial conjunctivitis: Bacterial conjunctivitis is a less common origin of conjunctivitis [127], is more frequent in kids and babies [128]. The most frequent bacteria are Haemophilus influenza, Streptococcus pneumoniae, and Staphylococcus aureus [129]. The Chlamydial conjunctivitis infection is one of the most common bacterial conjunctivitis [130], symptoms of this infection mostly include conjunctival hyperemia, mucopurulent discharge and lymphoid follicle growth [126]. Usually, treatment with oral antibiotics as Azithromycin or doxycycline is recommended to manage the infection [131].Gonococcal conjunctivitis, which Occurs via Neisseria gonorrhoeae, is a rare case of infection but it should be measured in neonates and sexually active adults[124].In order to treat the infection, Antibiotic treatment is the suggested therapy and the drug of choice ceftriaxone [132]. Also, patients should lavage the infected eye with saline [132-134].
Viral conjunctivitis: Pinkeye is the most common condition occurs by adenovirus; this infection is most common in adult than in children. Frequently, herpes simplex or zoster virus is responsible too. Usually, viral conjunctivitis is self-limiting and there is no need for antibiotics, for the relief they can use cold compresses, artificial tears or topical antihistamines [132], If there is a herpes simplex or zoster virus then antiviral should be given, such as acyclovir ointment or ganciclovir gel [126,132].
Infectious endophthalmitis
Is an inflammation inner eyes that can occur by infection thru microbes, involving bacteria or fungi [135]? It is an infrequent condition and its occurrence according to the reason. Risk factors for endophthalmitis involve cataract surgery, intravitreal injections (for age-related macular degeneration), and filtering bleb (for glaucoma) [136,137]. After the surgery is done, an ocular infection may be developed, the most frequent incident of infection is endophthalmitis, it caused by bacteria and it is found within seven days of surgery [137].
Conclusion
Ocular surface has a broad diversity of the composition of the microbiota, the distribution of the microbiota differ according to the ocular layers, Many factors may affect the microbiota and the ocular infection development, for example, contact lenses wearing considered to be a key factor for the biofilms formation and as a result the development of ocular eye infection. According to many types of research, both Gram-positive and Gram-negative bacteria may cause ocular infections and ophthalmic tissues damage in some cases. Still, Gram-positive bacteria are the main contributor of ocular infections, many types of ocular infection involves as conjunctivitis, keratitis, and endophthalmitis, some of these infection caused by the bad hygienic practice or the limited knowledge such as the infections caused by the contact lenses use, In spite of this, more investigation must be done in this field to find ways to prevent the infections, and create methods to eradicate the probability of biofilms formation and eliminate the microorganisms resistant.
To read more about this article...Open access Journal of Pharmacy & Pharmacology Research
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers





No comments:
Post a Comment