Authored by Alec Seidman Sorsby*,
Abstract
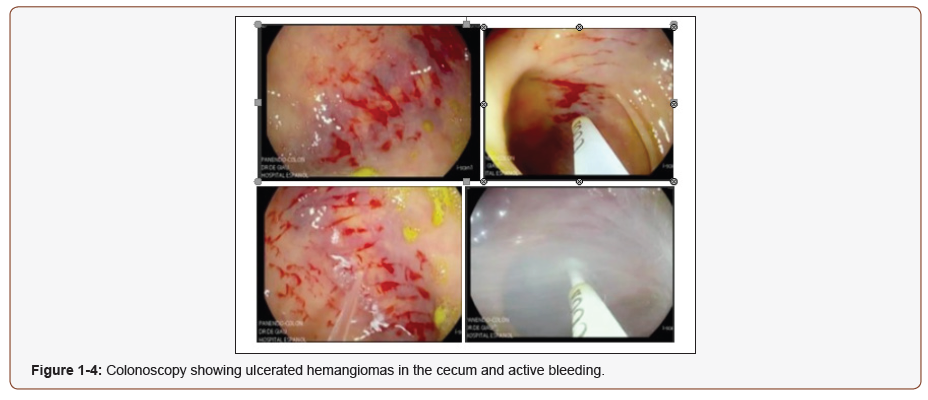
Angiodysplasia is the most frequent vascular abnormality on the gastrointestinal tract. It is an abnormal accumulation of dilated vessels with a thin and fragile wall that can easily break. Normally found in the right colon and measures between 2 and 5 mm. We describe a case of a 72 year old woman with a giant right colonic angiodysplasia of 3.5 cm of width with intraluminal and retroperitoneal hemorrhage. The patient had a history of consumption of antiplatelet drugs due to a prior myocardial infarction and three episodes of hematochezia. The colonoscopy showed ulcerated cecum hemangioma, active bleeding and management with hemospray. The treatment of the angiodysplasia was a right hemicolectomy and a laparoscopic mechanical ileotransverse anastomosis.
Keywords:Angiodysplasia; Intraluminal hemorrhage; Gastrointestinal Hemorrhage; Vascular Surgery; Vascular Abnormality
Introduction
Angiodysplasia is the most frequent vascular abnormality found on the gastrointestinal tract and it can be defined as the finding of tortuous, clustered, with a lack of smooth muscle layer, ectatic blood vessels in the mucosal and submucosal layers of the GI tract [1]. It is generally diagnosed with endoscopy, by the characteristic visualization of a classical red mucosal vascular lesion, usually less than 10 mm. [2]. Most of these abnormal blood vessels are identified in patients older than 60 years old. The main problem is the facility they have to break, which can lead to a small compensating bleed or in some cases, life threatening. The most frequent site these abnormal blood vessels are found is in the colon (80%) and in the stomach (5%) [3,4]. The pathophysiology of the disease is not completely understood, but it is believed to be secondary to lower oxygen levels and an aging process within the bowel wall. Some of the following risk factors have been identified: aortic stenosis, Von Willebrand disease and chronic renal failure. In case of having chronic renal failure, the presentation of angiodysplasia can be much younger, compared to the rest of the population [4,5].
Considering the location can vary, the clinical presentation of the gastrointestinal bleeding can be different depending on the location. Treitz angle is used a reference to determine whether the bleeding is of the upper Management will depend on the clinical context, incidental finding with no clinical manifestations of bleeding, do not require treatment, but in case of requiring treatment, different options both surgical and non-surgical are available, depending on the size, site and number of lesions. Here we describe a case of a giant right colonic angiodysplasia of 3.5 cm of longitude, with transmural affection and a retroperitoneal bleeding [4-6].
Case Presentation
72 year old woman presented to the hospital with lower gastrointestinal bleeding, which did not respond to non-surgical medical treatment. She had a prior history of a myocardial infarction, which was treated with a stent and double antiplatelet drug therapy. She presented with three episodes of hematochezia, indicative of lower GI bleeding. On physical examination a rectal examination was performed in which blood remnants were identified. A complete blood count initially showed a hemoglobin of 13.3 g/dl and 24 hours later of 9.4 g/dl. A colonoscopy was performed, ulcerated hemangiomas were identified in the cecum and an active bleeding was reported which was treated with hemospray (Figures 1-4).
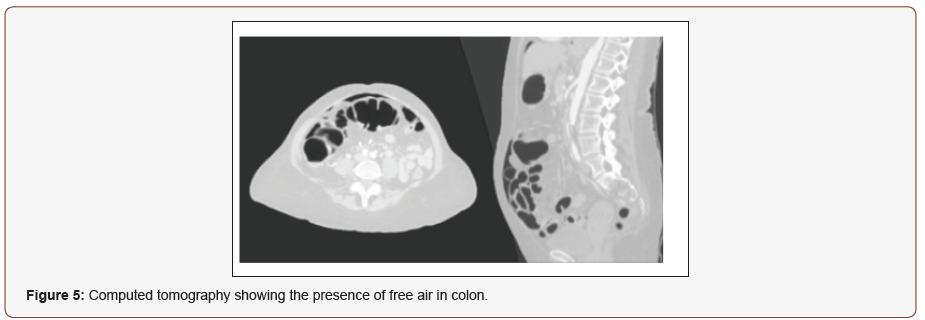
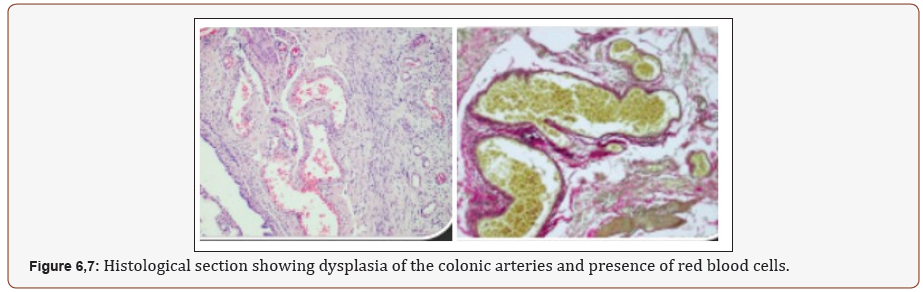
After the colonoscopy the patient referred intense pain in the abdomen, which was identified as an acute abdomen. A CT was performed, which showed the presence of free air, as a result of a perforation of a hollow abdominal viscera (Figure 5). The histological report showed dysplasia of the colonic arteries with recent thrombosis in the cecum and in the major arteries nonacute thrombosis was identified (Figure 6,7). The management of the patient included a right hemicolectomy with a mechanical laparoscopic ileotransverse anastomosis.
Discussion
Gastrointestinal angiodysplasia (GIAD) is a vascular abnormality which can be found on the gastrointestinal tract, which is characterized by pathologically dilated communications between veins and capillaries. GIAD are most frequently found in patients older than 60 years, but chronic kidney disease patients may present GIAD at an earlier age. It is characterized by lesions smaller than 10 mm and tend to be asymptomatic, in case of complication, signs and symptoms of GI bleeding will be present] The severity of GI hemorrhage may range from being chronic and well compensated to acute and life threatening. Angiodysplasia represents the most common cause of small bowel bleeding in patients older than 40 years old.
Several risk factors and associated conditions have been related to GIAD, such as aortic stenosis (AS), being prevalent in up to 25% of GIAD patients. Nevertheless, the relation between AS and GI bleeding remains controversial. Von Willebrand disease has been linked to GIAD due to alterations in adhesion and aggregation of platelets to the sub-endothelium. Although colonoscopy is considered the first-choice method in order to diagnose GI hemorrhage, as a result of new implemented diagnostic strategies such as capsule endoscopy and deep enteroscopy, the ability to diagnose angiodysplasia has drastically improved. The most common location these abnormalities can be found is the colon, specifically the right colon. Nevertheless, incidental finding of GIAD in locations such as the small bowel and stomach has drastically increased, leading to many asking the question, if the colon is the most frequent place for GIAD [3].
Normally the size of these abnormal blood vessels tends to be small (<10 mm) and are observed in mucosal and submucosal layers of the gut. In our patient, she had an angiodysplasia that measured 35 mm, which is three times larger than the normal angiodysplasia typically identified [6,7]. Histologically, dilated vessels lined by endothelium with little or no smooth muscle can be found. Giant angiodysplasia compared to the classic GIAD, does not resemble telangiectasias, the giant angiodysplasia looks more like a vascular tumor with tortuous vessels and capillaries [4,8].
The management of GIAD will depend on the clinical context, treatments should be individualized, depending on the lesion’s features, such as size and location. In some cases, treatment will not be required. Some of the therapeutics available for the management of GIAD are endoscopic therapies, angiography with embolization, surgical resection and pharmacological therapy [3,8].
Conclusion
Angiodysplasia is the most frequent vascular abnormality on the gastrointestinal tract, and it is defined as an abnormal accumulation of dilated vessels with a thin and fragile wall that can easily break. The most frequent location is the right colon, and they normally measure between 2-5 mm. It is fundamental to diagnose and treat gigantic angiodysplasia due to high risk of hemorrhage. Endoscopic treatment is an effective therapeutic strategy to stop the bleeding, although risk of perforation with free air is a possible complication. The definitive treatment is the resection of the affected organ, which in the case of the patient was the colon.
To read more about this article...Open access Journal of Anaesthesia & Surgery
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers
To know about Open Access Publishers





No comments:
Post a Comment