Authored by Aysha Siddika Mukta*,
Abstract
Objective: To explore functional visual assessment, pattern of presentations and refractive status of angle closure glaucoma.
Method: A hospital based prospective study was carried out at the glaucoma clinic of Chittagong Eye Infirmary and training complex for ophthalmic studies for the period of one year. 50 PACG patients were included in this study. Visual acuity, objective and subjective refraction, IOP, slit lamp biomicroscopy, visual field examination, contrast sensitive, color vision, gonioscopy, indirect ophthalmoscopy was done and types of glaucoma were recorded.
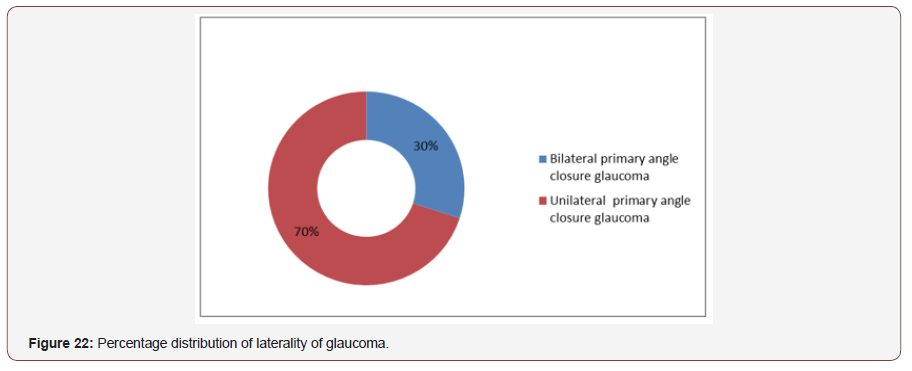
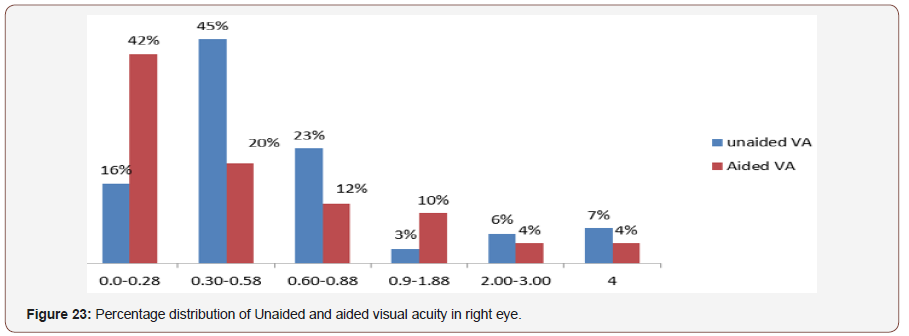
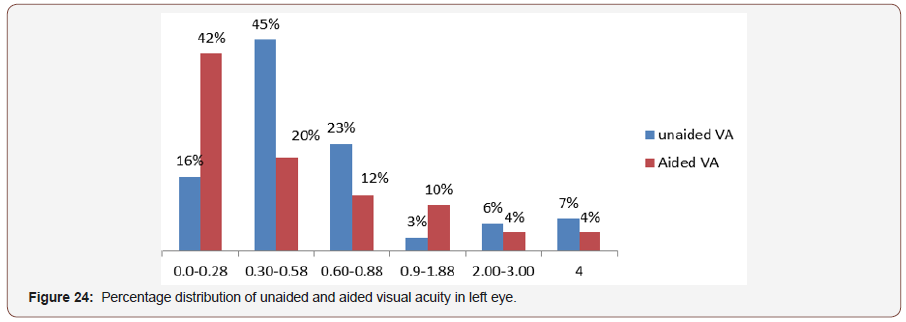
Result: The mean age was 52.6 and the standard deviation was 8.13. The most frequent range of unaided visual acuity in right eye in log mar chart in this study was 0.3-0.8 and the percentage was 49% and in the left eye was the 0.3-0.8 and the percentage was 52%. The frequent range of visual acuity after spectacle correction in right eye was (0.0 log unit) and the percentage was 50% and in the left eye was (0.0 log unit) and the percentage was 45%; which was strongly statistically significant. In our study significantly found 63% patients were hyperopic in PACG group which was more identical. Maximum patients came with moderate to severe increased of intra ocular pressure ranges from 30-70mmHg and more than 40% had enlarged C:D ratio 0.9:1. 40% patients were come with tubular field loss in right eye and 28% was in the left eye with advanced glaucomatous field defects. 75% patients had tritan defect in both eyes and 30% patients had bilateral primary angle closure glaucoma and 70% had unilateral angle closure glaucoma with other glaucoma subtypes.
Conclusion: Most of the PACG patient was associated with Hypermetropia. Most of them presented with advanced visual field defect, severe increased in IOP, advanced glaucomatous changes, poor contrast sensitivity and tritan color vision defect in both eyes. Identifying risk factors, early diagnosis, appropriate investigations and proper management in time could prevent the prognosis of the diseases.
Keywords: Primary angle closure glaucoma; Intra ocular pressure; Color vision; Cup disc ratio; Visual acuity; Contrast sensitivity; Hypermetropia
Introduction
Glaucoma is a characteristic acquired atrophy of the optic nerve due to gradual loss of retinal ganglion cells and their axons, which leading to blindness. This damage also affects the visual function and quality of life of an individual. Angle closure glaucoma (ACG) is a group of diseases in which there is reversible (appositional) adhesion (synechial) closure of the anterior chamber angle. The angle closure may occur in an acute or chronic form. In the acute form, the IOP rises rapidly as a result of relatively sudden blockage of the trabecular meshwork ™ by the iris via papillary block mechanism. The chronic form may develop after acute angle closure where synechial closure of the angle persists, or it may develop over time as the angle closes from prolonged or repeated contact between the peripheral iris and the TM, which often leads to peripheral anterior synechiae (PAS) and functional damage to the angle.
The glaucoma patients were classified into three main subtypes.
• Primary angle closure suspects (PACS): Greater than 270 degree of irido-trabecilar contact plus absence of peripheral anterior synechiae (PAS) plus normal IOP, disc, and visual field.
• Primary angle closure (PAC): Greater than 270 degree of irido-trabecular contact with either elevated IOP and or PAS normal disc and visual field examinations.
• Primary angle closure glaucoma: Greater than 270 degree of irido-trabecular contact plus elevated IOP plus optic nerve and visual field damage.
In other words, angle closure manifests the criteria of closure above, plus demonstrable and/ or visual field changes. The angle is abnormal in structure and function with optic neuropathy. shaffers et al. In the term of pathophysiology angle closure occurs when the peripheral iris is in contact with the trabecular meshwork (TM) either intermittently (appositional closure) or permanently (synechial closure) According to world health organization (WHO) the glaucoma is the second commonest cause of worldwide blindness which affects 6.7 million people [1]. The proportion of blindness caused by angle closure glaucoma (ACG)is greater than that caused by open angle glaucoma. Queigley QH [2] estimated that the number of people with bilateral blindness from ACG will be 5.3 million by 2020 [3]. more than 80% of ACG patients resides in Asia, and around 50% lives in china.
According to WHO about 4 crore people in the world are blind while 24 crore are suffering from low sight [2]. Early diagnosis as well as proper treatment at the early stage could minimize the damage of 80% of the glaucoma patients. According to national blindness prevalence survey, among the total blindness in Bangladesh approximately 5, 86,000 people (40 years and older) have definite or probable glaucoma. A survey report by Bangladesh Glaucoma Society (BGS) states that 95% of the Glaucoma patients unaware that they were suffering from this disease.
Although according to the national blindness survey 3% of the total blindness is due to glaucoma but the numbers of glaucoma suspect people (PACS, PAC) are probably several times higher those are out of glaucoma care [2].
Those Glaucoma suspect people are usually out of glaucoma care due to lack of health care facilities and their lack of awareness results in development of advanced followed by blindness. In case of chronic angle closure glaucoma is often discovered incidentally during routine examination or during examination for another reason. ACG can also present with intermittent symptoms, change in vision, or severe acute symptoms such as pain in the affected eye, headache, associated with nausea or vomiting. patients who suspected of having ACG should be referred to ophthalmology care immediately.
Optometrist through their clinical education, training, experience and broad geographic distribution can provide an effective primary eye and vision care for the patient with primary angle closure glaucoma. According to American optometric association there are some roles of optometry in PACG. Those are to identify patients at risk of developing and accurately diagnose PACG, preserve the gains obtained through treatment inform and educate patients and other health care practitioners about the visual complications ,risk factors, treatment options and adverse reactions to treatment associated with ACG16.there is currently no nation –wide programme to tackle the diseases in the country .The study aims at determining the burden and presentation patterns PACG ,using hospital based data to highlight the need to develop nationwide intervention to tackle the diseases.
Methodology
Study period: 1year october2014-september 2015.
Study place: Glaucoma clinic. Chittagong eye infirmary and training complex.
Study design: Hospital based prospective study.
A hospital based prospective study was designed in order to evaluate the Functional visual assessment, pattern of presentations and refractive status of Primary Angle closure Glaucoma patients presenting to the glaucoma clinic of Chittagong Eye Infirmary & Training Complex, Bangladesh who was newly diagnosed and had previous attack as Primary Angle closure Glaucoma. 50 subjects of over 40 years of age were examined. The patients were informed about the study. For data collection consent was taken from them including their age, gender, occupation, educational qualification etc by face to face interview with the patient in the clinic. Primary Angle closure Glaucoma was defined as an intra ocular pressure of more than 35 mmHg or higher in presence of typical glaucomatous optic disc changes with close angle in Gonioscopy. Patients with age of lower than 40 years and other ocular abnormalities like mature cataract, corneal edema, acute inflammation and infection in the eye, pathological conditions of the optic nerve other than glaucomatous changes and history of any ocular surgery other than cataract surgery were excluded from this study.
Visual acuity without correction, with correction, and with pinhole will be measured with Bailey Lovie Log MAR vision chart. Objective refraction was performed with the retinoscope (Beta 100, Heine, Germany).
The intra ocular pressure was measured by Goldman Applanation tonometer.
• Slit lamp biomicroscopy will be done by the consultant in glaucoma clinic.
• Visual field will be assessed in Hamphery visual field analyser.
• Contrast sensitivity test will be recorded with Bailey Lovie 10% contrast sensitivity chart.
• Color vision test will be done fransworth dichotomous D-15 hue test.
• Gonioscopy was done with 4 mirror goniolens.
• Gonioscopic angle grading was done by the consultant of the clinic and was documented accordingly
• Indirect Ophthalmoscope (Volk lens, 90 D) will be used to measure the vertical cup to disc ratio.
• Finally, the diagnosis of glaucoma will be recorded with the help of the consultant of the glaucoma clinic.
Statistical analysis will be performed with SPSS (for windows XP; SOSS 16.0 Inc, Chicago, IL, USA).
• Graphical presentation of data will be done with Microsoft office excel sheet.
Descriptive statistics will be used for analysis of data.
Result
Demographic Characteristics
Age distribution of the patients: The mean age of studied population was 52.6 and the standard deviation was 8.16 (Figure 1).
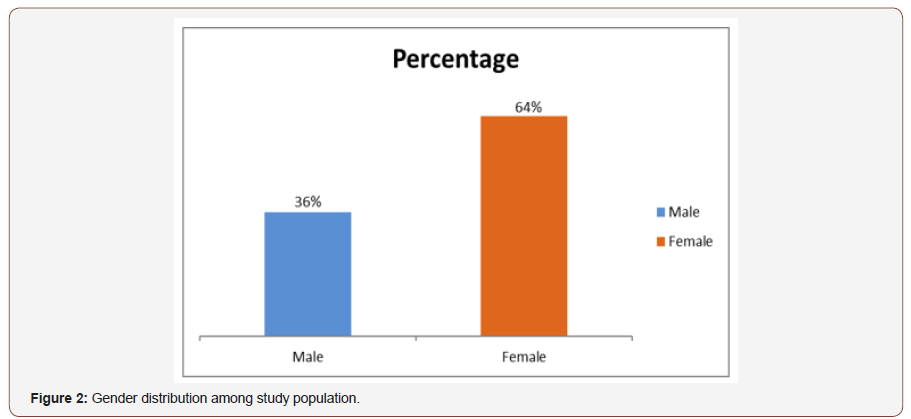
Gender distribution of the respondent: The study included 100 eyes of 50 primary angle closure glaucoma subjects. Among them 36% were males and 64% were females (Figure 2).
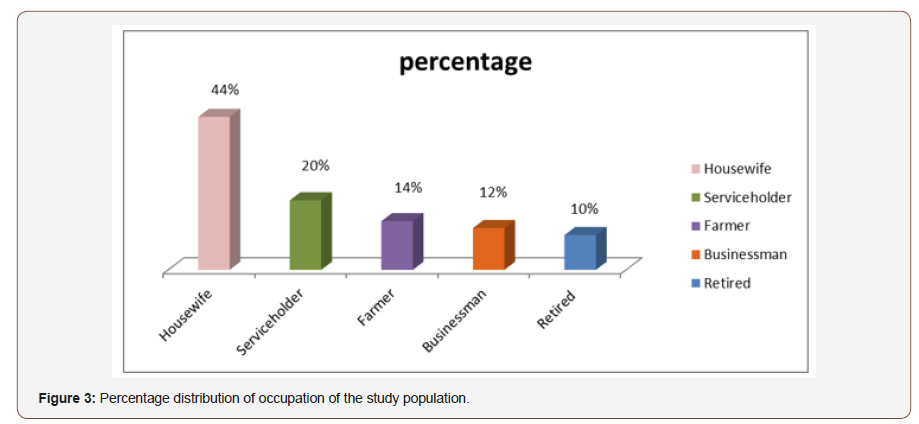
Occupation distribution of ACG patient: Out of 50 subject 10% was dependent on their families, 44% were housewife, 20% were service holder, 14% were farmer and 12% were businessman (Figure 3).
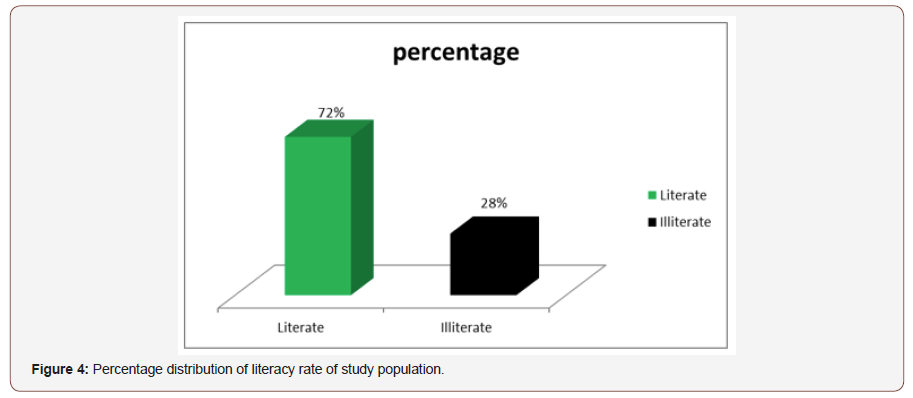
Literacy rate distribution of the study population: Among 50 patient 36(72%) were literate and 14(28%) were illiterate (Figure 4).
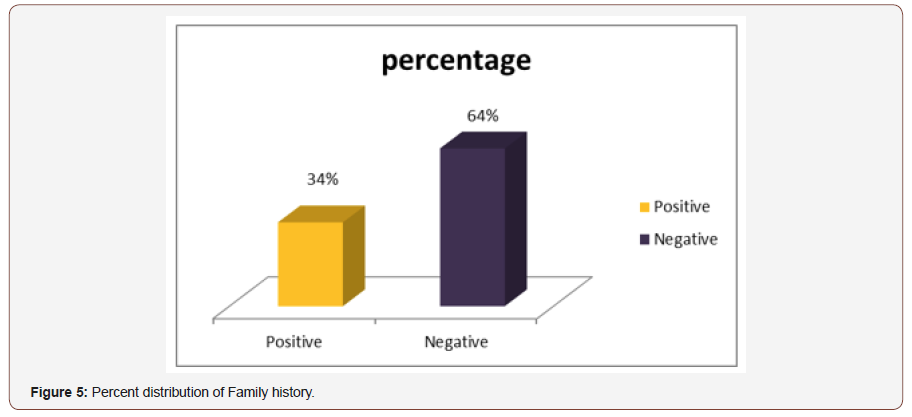
Family History of respondent: Among 50 patient 64% family history was positive and 34% was negative (Figure 5).
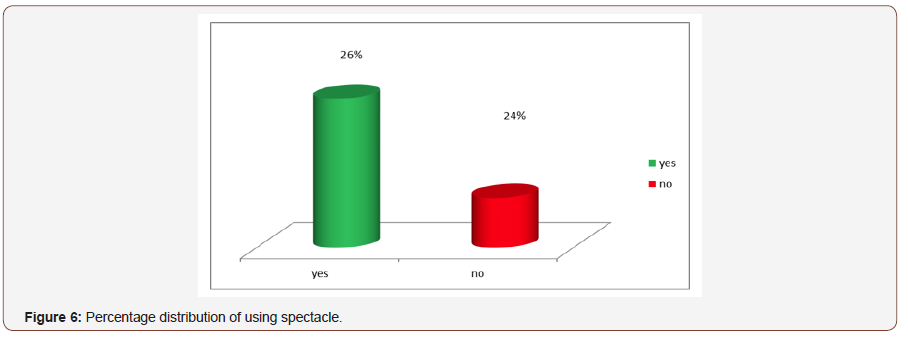
History of using spectacle of the patient: Among 50 patient 26% were using spectacle and 24%had no history. Maximum patient was using spectacle for near distance (Figure 6).

Clinical Characteristics
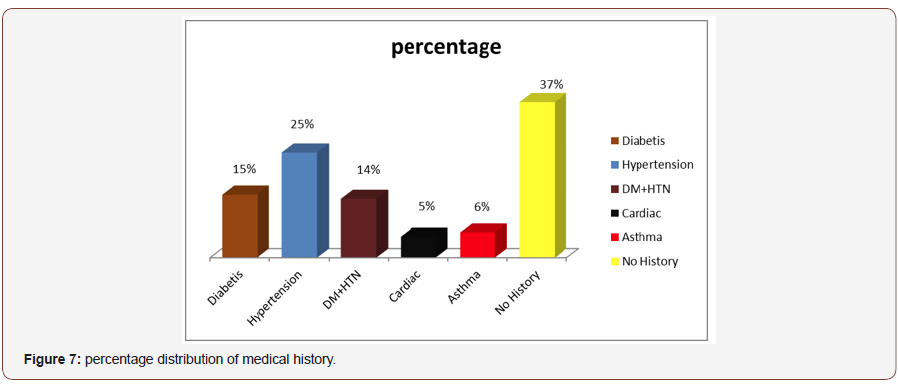
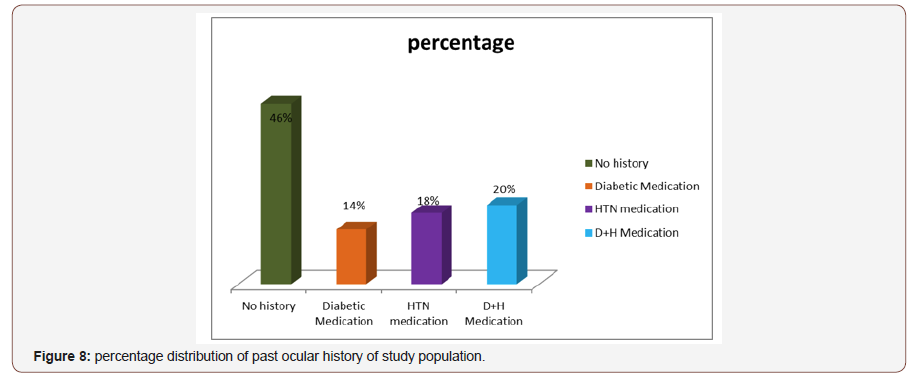
Past Ocular History of the respondent: Maximum patient had no past ocular history (46) but 18% were hypertension medication,20%were diabetes and hypertension medication,14% were only diabetic medication (Figure 8).
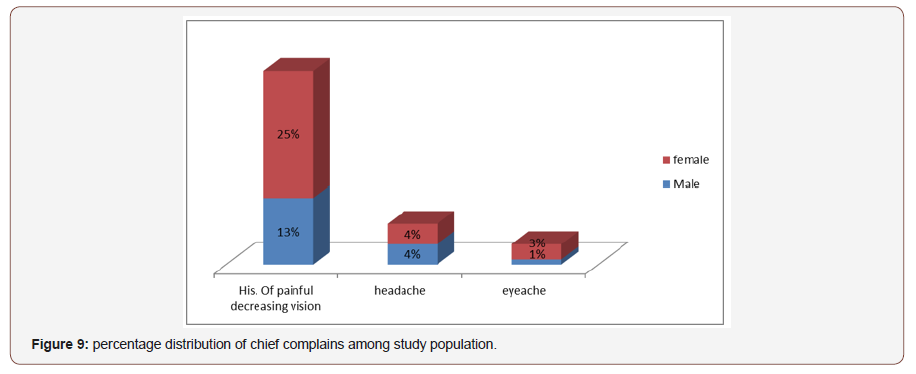
Percentage distribution of Complain with age:Most Patients complaining of decrease vision at both near and distance where female are comparatively more affected where 25% were female 4% male and female percentage were same with the complain of headache.3% were female and 1% were male with the complain of eye ache (Figure 9).
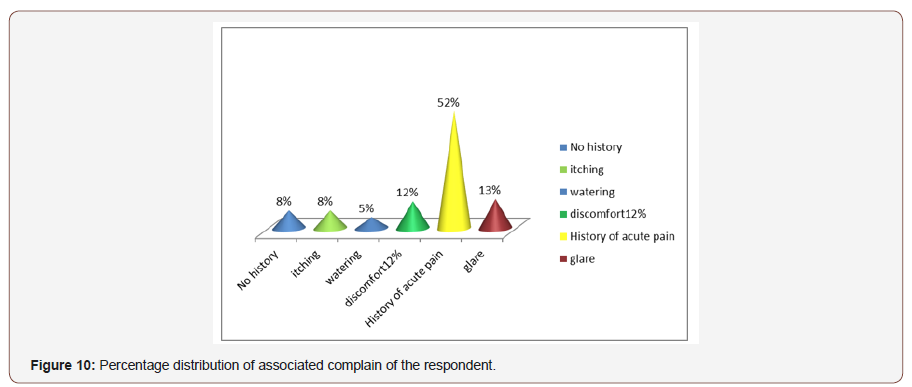
Associated Complain the population:Maximum patient had a history of acute pain 52%, others were 13% glare,12% discomfort, itching 8%, watering 5% and 8% had no history (Figure 10).
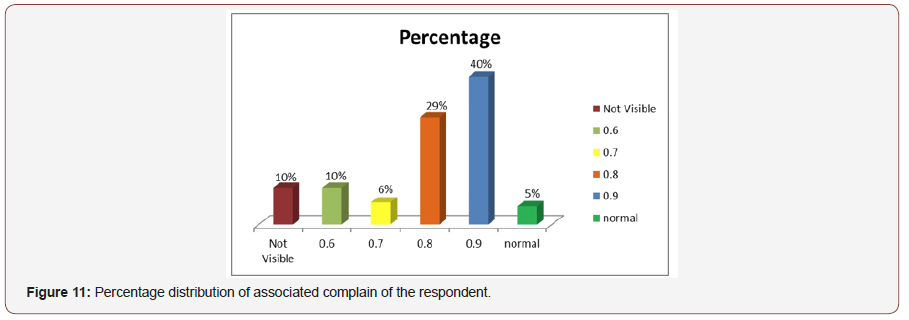
Distribution of cup disc ratio of right eye:40% patient had cup to disc ratio was 0.9 in right eye.0.8% Was 29% cupping,10% was o.6 cupping ,6% was 0.7 cupping,5% normal and 10% were not visible due to corneal edema or cataract (Figure 11).
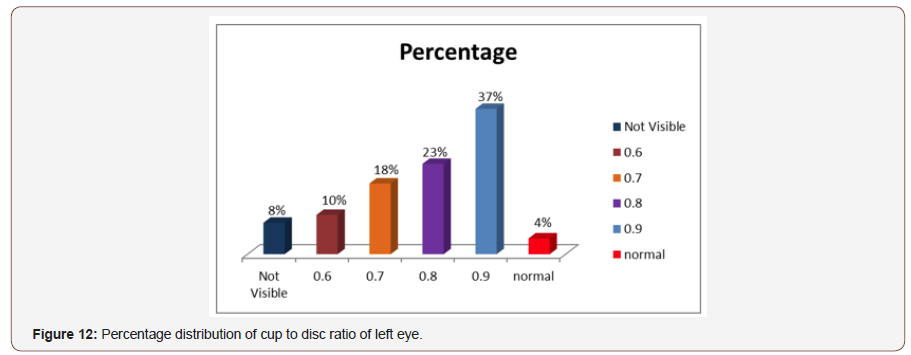
Distribution of cup disc ratio of left eye:Maximum 37% patients had cup to disc ratio awe 0.9 in left eye.23% was 0.8 cupping, 18% was 0.7 cupping, 10% 0.6 cupping and 8% not possible due to corneal oedema or cataract (Figure 12).
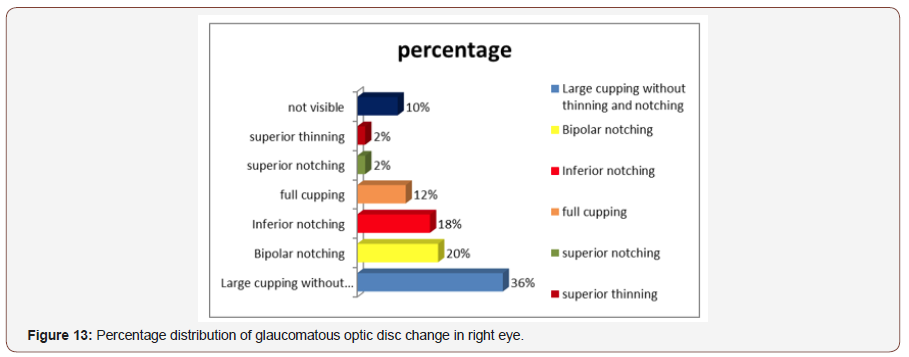
Distribution of glaucomatous changes in right eye:About 36% patients were presented with large cupping without thinning and notching, while 20% with bipolar notching, 18% inferior notching,12% full cupping,25 with superior and superior notching and 10% were not visible due to cataract or corneal haziness (Figure 13).
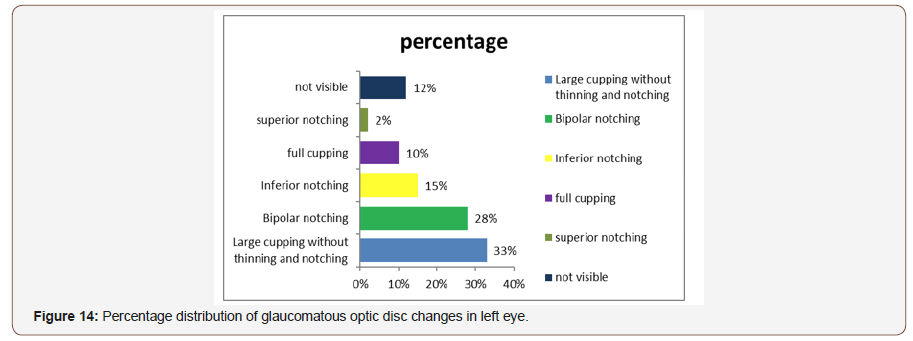
Distribution of glaucomatous changes in left eye:Maximum patient were come to the clinic with large cupping without thinning and notching (33%) while bipolar notching was 28%,15% inferior notching,10% full cupping, 25 were superior notching and 12% was not visible due to cataract or corneal haziness (Figure 14).
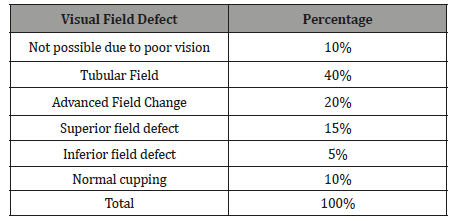
Status of Visual field defect in right eye: Out of 50 respondent 40% were come with tubular field in right eye 20% were advanced field defect, 15% were superior field defect,5% were inferior field defect, 10% were normal cupping and 10% were not possible due to poor vision (Table 1).
Table 1: Status of field defect in right eye.
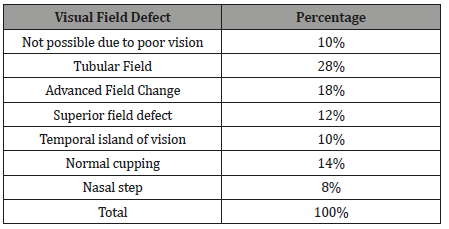
Status of Visual field defect in left eye:In the left eye out of 50 patients 28% were come with tubular field in the left eye at the clinic while 18% were advanced field defect 14% were normal cupping,12% were superior field defect 10% were temporal island of vision , 8% were nasal step and 10% were not possible due to poor vision (Table 2).
Table 2: Visual field defect in left eye.
Status of color vision in right and left eye:Out of 50 patient 50% had tritan defect in right eye and 40% in left eye, 12% deutran defect in right eye and 18% in left eye, 2% protan defect in right and left eye, 4% only blue colour defect in right eye and 2% in left eye, 2% only yellow color defect in right eye and 10% in left eye, 22% normal color vision in right eye and 20% in left eye, rest are not possible due to poor vision (Figure 15).
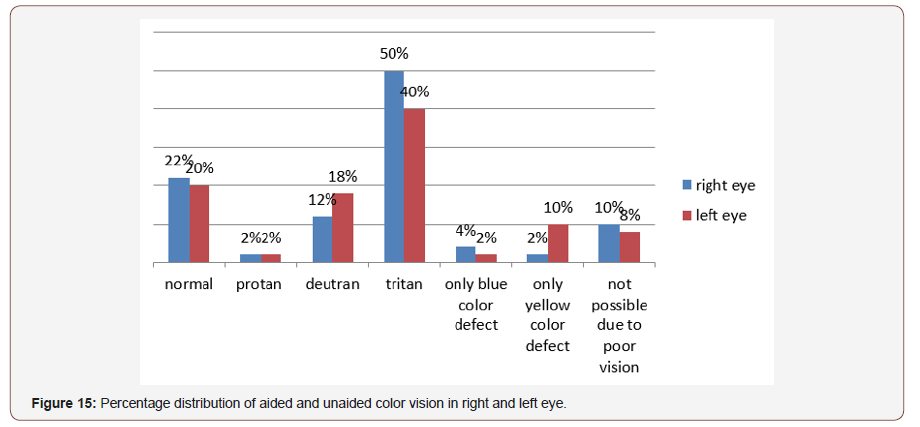

Status of color vision in both eye:43% patients were came with tritan defect bilaterally at the clinic. 19% patients had deutran defect, 7.60% had only yellow color defect, 3.80% had only blue color defect. Color vision could not examine in 24.10% patients due to their poor vision (Figure 16).
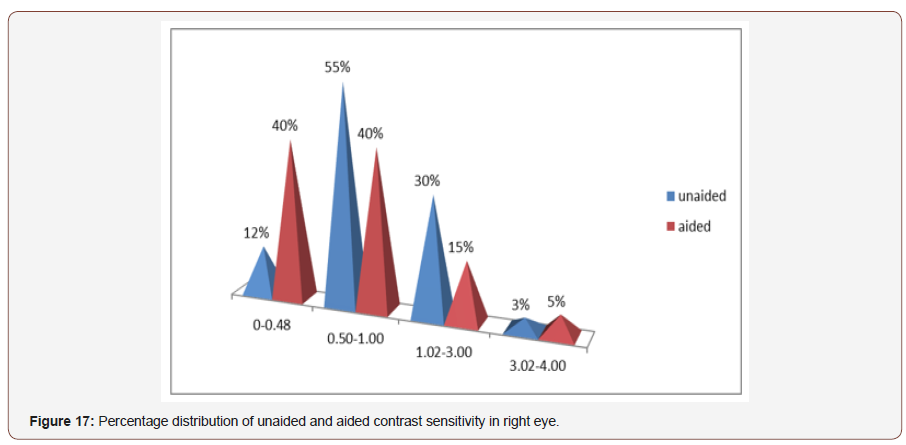
Distribution of contrast sensitivity in right eye:Among the study population the most frequent range of unaided contrast sensitivity in right eye was 0.5-1.00 log units and median was 0.82 log units, where the aided contrast sensitivity was 0-0.48 log units and the median was 0.60 which was statistically significant (p>0.00, at 0.1 level) (Figure 17)
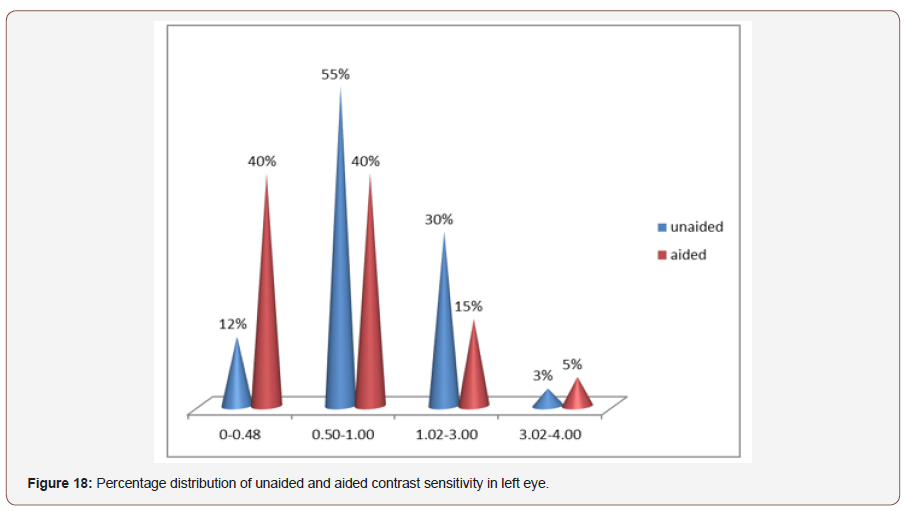
Distribution of contrast sensitivity in left eye: In left eye the most frequent range of aided contrast sensitivity was 0.50-1.00 log units and the median was 0.84 log units where the aided contrast sensitivity was also 0.50-1.00 log units and the median was 0.52 log units ,which was statistically significant(p<0.001) (Figure 18).
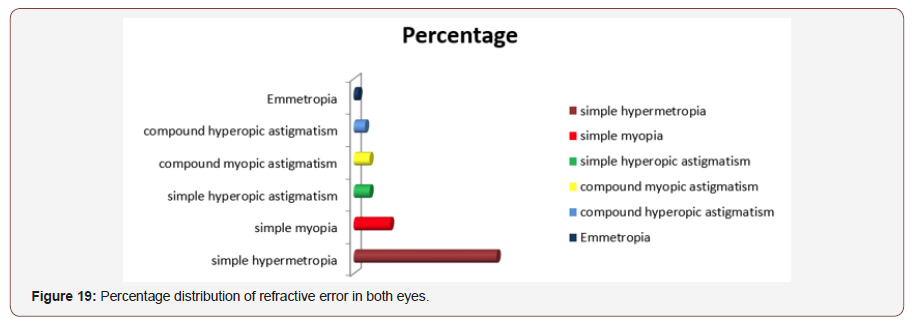
Percentage distribution of Refractive status of both eyes: Out of 50 patients 63% patients had simple hypermetropia in both eyes,16% had simple myopia,7% had both simple hyperopic astigmatism and simple myopic astigmatism,5% had compound hyperopic astigmatism, and 2%had mixed astigmatism (Figure 19).
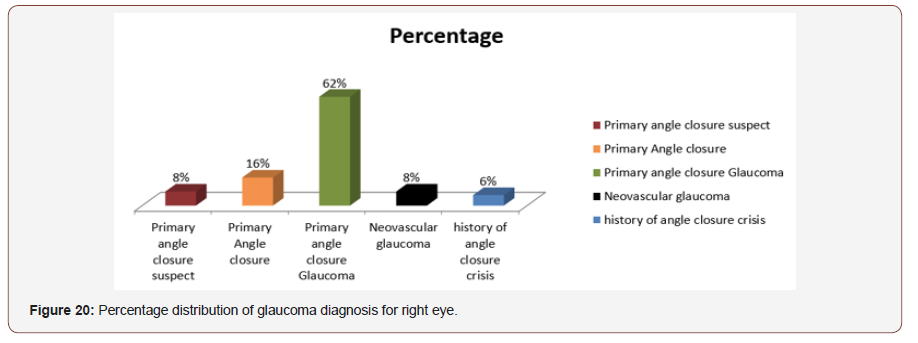
Diagnosis pattern for right eye: Out of 50 patients 62% had primary angle closure glaucoma, 16% had primary angle closure, 8% had primary angle closure suspect and neovascular glaucoma and 65 had angle closure crisis (Figure 20).
Diagnosis pattern for left eye:Out of 50 patients’ maximum patients (55%) had primary angle closure glaucoma,27% had primary angle closure, 10% had neovascular glaucoma, 6% had primary angle closure suspect and 2% had primary open angle glaucoma (Figure 21).

Status of laterality of diagnosis:Out of 50 patients, among them 30% had bilateral primary angle closure glaucoma and 70% had unilateral primary angle closure glaucoma (Figure 22).
Distribution of visual acuity
Visual acuity in right eye-: The most frequent range of unaided visual acuity inright eye was 0.30-0.50 log unit and the percentage were 45% where the aided visual acuity was 0.0-0.28 log unit and the percentage were 42%; which are statistically significant (p value=0.00) (Figure 23).
Visual acuity in left eye:In the left eye the most frequent range of unaided visual acuity in left eye was also 0.30-0.50 log unit and the percentage were 45% and the aided visual acuity was 0.o log unit in log Mar chart and the percentage was 42% which was str0nglt statistically significant(p=0.00) (Figure 24).
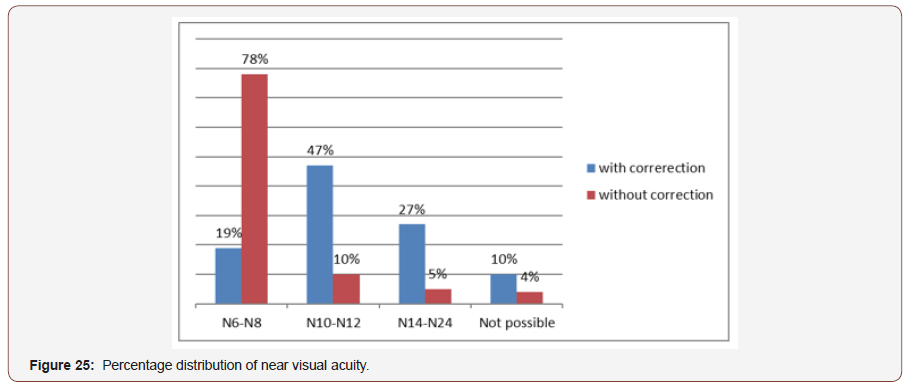
Near Visual Acuity in both eyes: The most frequent range of unided near visual acuity without correction was (N10-N18) where the aided visual acuity was (N6-N8) which are strongly statistically significant(p value=0.00) The mean of near visual acuity without correction was N12 and with correction was N8 and standard deviation as +2 (Figure 25).
Discussion
The purpose of the study was to determine how primary angle closure glaucoma affects the functional vision, pattern of presentation, and refractive status.
[4] reported that patient came with primary angle closure glaucoma in Chinese ethnicity with a mean age of 69.8 years at enrollment (1). In my study I found the mean age of study population was 61 year. [5] reported The influence of gender where female are more affected in angle closure subtype like PACS(59/93; 63%) as well as PAC(201/312; 64.5%),but IN PACG category males(235/409; 57.5%) significantly outnumbered females (174/409; 42.5%) with total population of 814.in my study I found female are more affected in all subtype of glaucoma because of their hormonal effect, lack of health care facility, lack of health education and their self-ignorance.
Leske MC et al. reported that family history of glaucoma is the risk factor for PACG. In my study I found 34% had positive family history and 64% had negative family history which is not similar to the result. It may because of their illiteracy and ignorance of the study population and their family members. HM Von Romude et al. did an assumption that hyperemia would be a strong risk factor for PACG. But hyperopic was not statistically significantly more prevalent in PACG group than in the control group.
Since then several studies relationship between PACG and hyperopic was found in Indian urban area12.The Beijing study found a relationship between hyperopic and anterior chamber angle, suggesting that hyperemia is a predominant risk factor. In my study I also found the evidence of increased risk of primary angle closure glaucoma among hyperopic was stronger in all subtypes of hyperopia among them 70% were hyperopes which is, more identical to that study. I didn’t do any genetic analysis to find out correlation. [6] reported ACG occurred maximally in the sixth decade (12) in their study 269 patients were less than 50 years old and 54 were less than 40 years of age, which is in agreement with the study by [6]. But in my study, I found the mean age of the total population was 52.6 [6] documented that diminution of vision and ocular pain were common in PACG Than PAC and PACS. where Pain was the chief presenting complaint (62.1%) and subacute grouos (45.5%) But in my study I found most of the patient had diminution of vision at near and distance and history of acute pain and there percentage was 25% and 52% respectively.
Almost the angle closure subtypes, PACGwas the most common seen in 402 patients (n=814; 49.4%) followed by PAC in 323 patients (39.7%) and PACS in 93 patients (11%). In patients with different subtypes of angle closure in both eyes the eyes with the higher degree of angle closure was used for categorization. In my study I also found PACG as a most common occurance among all subtypes with 30% bilateral PACG and 70% were the rest [5-14] M Gyasi et al. showed that more than 70% eyes had cup disc ratio greater than 0.8 while 54.9% had a cdr of 1,in my study I found 55% patints had cup disc ratio n was 0.9. Intra ocular pressure remains the most significant risk factor for the glaucomas and indeed the onlt one than can currently be modulated in my study I also found that maximum patients were present with high intraocular pressure ranges from 30-70 mmHg. 37% patients in my study were presented with tubular vision at the clinic but the abnormality was not self-reported due to their lack of ides about visual field defect. Another more significant finding of my study was the contrast sensitivity and color vision defect among the patient with PACG.75% patient had tritan defect bilaterally that is exception of kollners rule. among the study population the most frequent range of unaided contrast sensitivity in both eyes was 0.05-1.00 LOG UNIT, where the aided contrast sensitivity was also 0.5-1.00 LOG UNIT in left eye and was 0.48 in LOG UNIT in right eye. The most frequent range of unaided visual acuity in right eye in LOGMAR chart in this study was 0.3-0.8 log unit and the percentage was 50% and in left eye was 0.3-0.8 log unit and the percentage was 45%.The frequent range of visual acuity after spectacle correction in right eye was 0.0 log unit and left eye was 0.0 log unit which was strongly statistically significant(p=0.00).The most frequent range og unaided visual acuity in both eye wasN10- N12 and the aided near visual acuity was N6-N8 which was strongly statistically significant(p=0.00). In our study we got 30% cases there was bilateral PACG and 70% unilateral PACG. In unilateral cases I have examine the other eye, which are at the risk of glaucoma and I got 8% PACS, 16% PAC, and 8% NVG, it means these are also case of PACG where vascular insufficiency results in NVG.
Conclusion
In the developed country like Bangladesh most of our populations are very much unaware about their eye care due to their lack of education and remoteness of eye care center and lack of eye care facilitie in the rural area and aggrevates the crisi. Doing this study, we found the most of our patients in PACG are at the advanced stage and hyperopia was the risk factor and all are presented with morderate to high IOP and tritanopia [15-20]. The data also provide strong evidence that the riek of patients over 50 years with PACG Presenting to the hospital eye service with advanced visual field defect is independently associated with age, gender, headache, smoking, hypertension and diabetes. Humphery visual field, color vision, contrast sensitivity measurement should be include in the comprehensive ocular examination because accurate measurement of these examination has direct impact on screening diagnosis and management of PACG. Early diagnosis in primary eye care center followed by proper referral to the highest centre in time could prevent their advancement conditions. Early diagnosis in primary eye care center followed by proper referral to the higher center in time can prevent their advancement.
To read more about this article...Open access Journal of Ophthalmology & Vision Research
Please follow the URL to access more information about this article
To know more about our Journals...Iris Publishers
To know about Open Access Publishers





No comments:
Post a Comment