Authored by Felipe de Jesús Montelongo*,
Abstract
Objective: To describe the placement of ultrasound-guided central venous access in the prone position in patients with severe acute respiratory distress syndrome due to COVID-19.
Design: Transverse and prospective, with reports of cases of hospitalized patients.
Setting: Adult intensive care unit, of a second level teaching hospital in Ecatepec, State of Mexico.
Participants: Hospitalized patients diagnosed with severe PNEUMONIA due to COVID-19, who required prone position and placement of central venous access, were included from March to September 2020.
Primary outcome measures: Placement of central venous access in prone position guided by ultrasound.
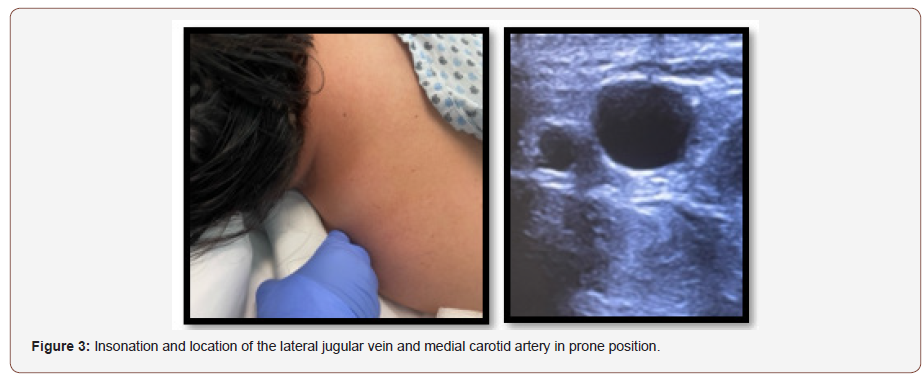
Result: Three patients were included, with predominance of the male sex, with a grade II obesity in 66%, grade III obesity in 33%, with an average of 6 days in the prone position, two required the change and placement of catheter due to obstruction and one case for requiring the installation of a hemodialysis catheter due to the initiation of continuous slow therapy to replace renal function. The number of operators was one to two and the most common site of vascular insertion was the left jugular. The number of punctures was 1.6 times, with a puncture time to insertion of the metal guidewire of 45 to 55 seconds. None had complications.
Conclusion: The placement of central venous accesses in the prone position with ultrasound support is a procedure that facilitates insertion and is apparently fast and safe. However, it is a procedure of which there is little description within the international medical literature.
Background
COVID-19 is an emerging viral disease, which was detected in Wuhan, China in December 2019, with first cases being identified as pneumonia of unknown cause [1-3]. In February 2020, the World Health Organization described it as COVID-19 and the disease was declared an international emergency on January 30, 2020 [4]. Atypical pneumonia due to SARS-CoV-2 generally presents with severe acute respiratory distress syndrome (ARDS), producing an alteration in gas exchange. Patients with a < 150 PaO2/FiO2 ratio and a fraction of inspired oxygen requirements greater than 60% are considered as candidates for initiation of the prone position strategy, which seeks to improve the posterior lung recruitment to improve hypoxemia and the PaO2/FiO2 ratio, as well as the prognosis and survival of these patients. This is carried out for a 16-hour periods that can be prolonged for up to 72 hours (still considered as prone safe) when the withdrawal criteria are not met. After this time, the risk of complications increases [4,5].
Case Descriptions
Herein, we present three cases of patients with critical pneumonia due to COVID-19 who developed severe ARDS and were admitted to the adult intensive care unit of the Hospital General de Ecatepec “Las Américas,” ISEM, State of Mexico, Mexico. These patients were intubated under mechanical ventilation in a prolonged prone position, with a 6-day mean, due to refractory hypoxemia. Two patients had to have the central venous catheter removed because of lumen obstruction and a 7 French tri-lumen catheter was placed. The third patient had a 12 French hemodialysis catheter installation as they developed acute renal failure and met criteria for initiation of renal replacement therapy (Table 1).
Table 1: Characteristics of the patients who underwent vascular access in the prone position. No patient presented complications to the post-procedure ultrasound scan.
Procedure and Technique
The purpose of the authors is to describe the performance of central venous access with the jugular approach in the prone position guided by ultrasound following personal protection measures for SARS-CoV-2. After obtaining the relatives’ consent for the procedure, the doctors proceeded to put on the personal protective equipment that consisted of a Tyvek suit, double gloves, surgical boots and cap, anti-fog goggles, and/or full-face mask. They also wore a sterile surgical gown and an extra pair of sterile gloves as barrier measures. It should be noted that these steps represent an additional degree of difficulty to the procedure.
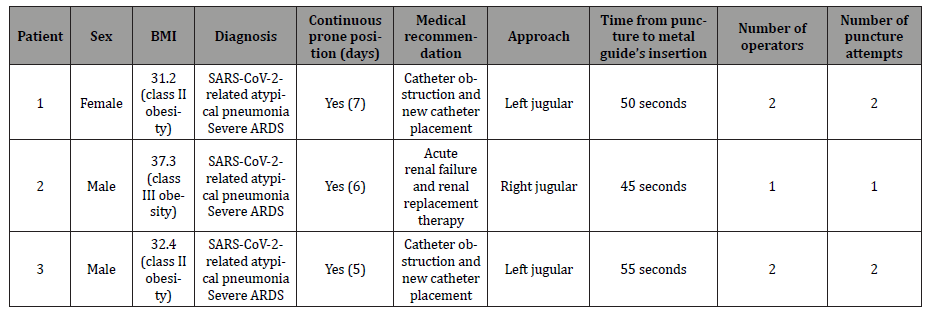
1. First, the patient in the prone position is placed in Trendelenburg position (Figure 1).
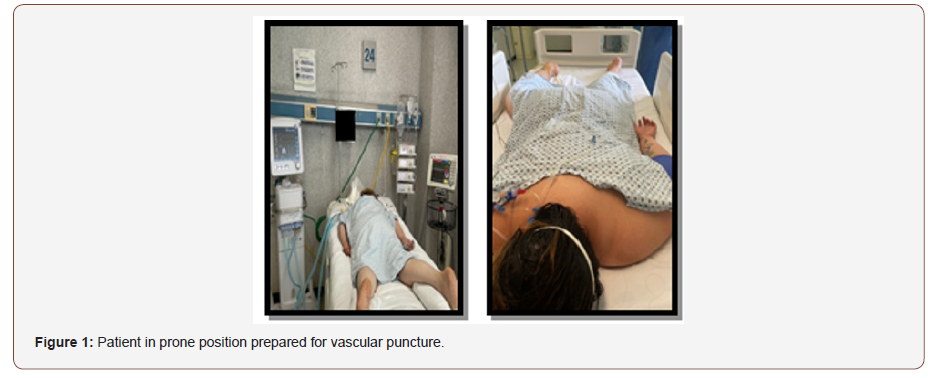
2. Then, the head is rotated to the opposite side of the chosen site to perform the jugular approach or, if there are head and face protections for the prone position, the head is left in a neutral position (facing the bed). During the procedure, both arms are placed close to the thorax, and are returned to a swimmer’s posture when the procedure is completed (Figure 2).
3. Site insolation should be performed before puncturing to ensure that the vessel exists and to confirm its position and/or possible anatomical abnormalities. Asepsis of the neck chosen for approach is performed and sterile drapes are placed on the back and head.
4. A 7-13 Hz linear transducer is used; sterile gel or sterile saline solution is placed on it using a sterile piping bag or pads to cover the transducer probe (Figure 2).
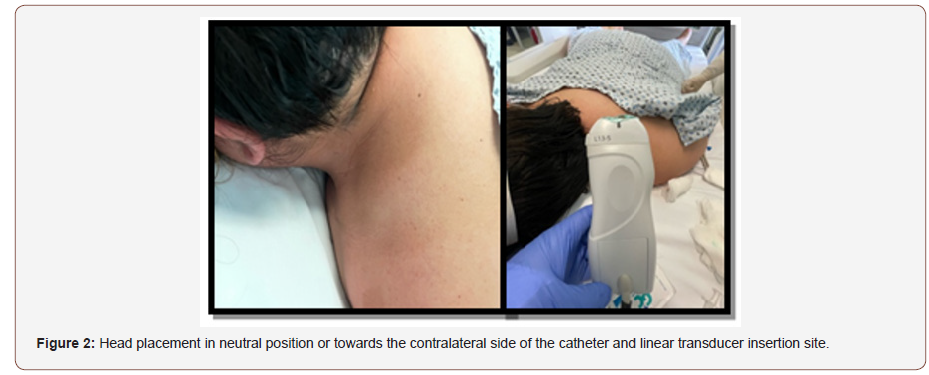
5. The traditional material for central venous access is prepared.
6. After identifying the area of the neck to be insolated, the linear transducer is positioned directing the mark towards the anterior region of the neck to identify the vessels in a transverse position since the external jugular vein is (often irregularly) completely compressible with the transducer and the pulsatile carotid artery has thick and usually round walls. Then, the mark is directed to a cephalic position to identify the longitudinal vessels (Figure 3). The subcutaneous cellular tissues and sternocleidomastoid muscle’s structures are identified with the vein in its longitudinal trajectory above the longitudinal trajectory of the carotid with a depth of about 1.5-to-3-cm. The site to be punctured is identified and local anesthesia is placed with 1% lidocaine. Afterwards, the puncture is carried out after visualizing the needle and the vein in the plane; the entry of the needle into the venous vessel is observed, thereby confirming the return of blood by aspiration and the insertion of the metal guide. The transducer is removed, and the dilator is inserted. The central venous catheter insertion is continued while the metallic guide is withdrawn. Once the venous catheter is inside the vessel, insolation is performed and its presence and venous return by lumens are confirmed. Lastly, the catheter is fixed, and the procedure is finished. The same technique is used for the hemodialysis catheter.
7. Finally, an ultrasound scan is performed on the vessel and puncture site, to evaluate the catheter position and rule out the presence of bruises, catheter knotting, etc. A pulmonary ultrasound is also done to evaluate the presence of pneumothorax, hemothorax or subcutaneous emphysema. This allows us to evaluate complications quickly and avoids the need to move the patient for a radiology study.
Patient and Public Involvement
Due to the nature of the pandemic and the severity of the disease in hospitalized cases, patients and the public were not involved in the development of the research, results, or in the design, recruitment, and conduct of the study.
Discussion
The severe acute respiratory distress syndrome due to COVID-19 requires handling strategies to improve the hypoxemia it generates. Among these strategies mentioned in the literature are the use of prone position, which recently has been used early and for a long time in patients with severe pneumonia in the intensive care unit. During this pandemic, it has been observed that patients cannot supinate because they do not meet the criteria or because when they are back in the supine position, they develop refractory hypoxemia. Therefore, being able to place a central venous access, which is very necessary in this type of patient, is problematic; so, the performance of the ultrasound-guided central venous access placement procedure in the prone position was considered as a solution.
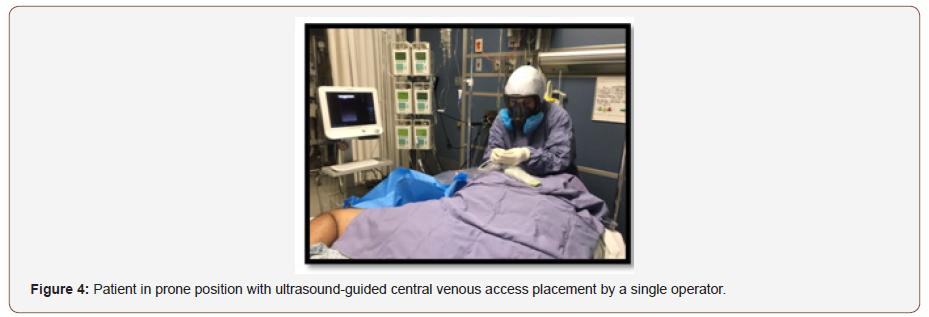
The benefits found in this technique are keeping the prone position, safety after ultrasound identification of the vessel to be punctured and, probably, less vascular puncture attempts and less time in the duration of the procedure. It is very important to take this last detail into account since personal protective equipment is worn, which increases technical difficulty, tiredness, and fatigue. The disadvantages found were the same as for the standard technique, such as the fact that, in obese patients or patients with a short neck, the adipose tissue makes placement difficult by reducing the space to maneuver the transducer and the puncture needle. In addition, in the case of personnel with little experience with ultrasound, it requires someone in charge of guiding the transducer and another person or operator performing the puncture and catheter placement (Figure 4). The use of personal protective equipment in this series of cases increased the technical difficulty, but the puncture time (50 seconds in average) and the presence of complications, such as local hematoma, pneumothorax, or subcutaneous emphysema, were the same.
Conclusion
The central venous access placement in prone position guided by ultrasound is a procedure that has not been widely described in the medical literature. Performing this approach by ultrasound facilitates placement with an approximate time of 0.5 to 1 minutes from puncture to insertion of the metal guide.
To read more about this article...Open access Journal of Cardiology Research & Reports
Please follow the URL to access more information about this article





No comments:
Post a Comment