Authored by Machado AE and Sander BQ*,
abstract
Introduction: Obesity is a public health problem of global proportions that has shown alarming growth rates, including among children and adolescents. The clinical treatment of obesity has very expressive success rates, but with a very high recurrence rate. The Intragastric Balloon (IGB) is an option for these patients.
Methodology: Data were selected from individuals attending a private obese outpatient medical center. All patients were certified by telephone and invited to participate in the study. During data collection, the following questions were asked: Follow-up with a nutritionist; followed up with a psychologist. Performed regular physical activity; Presence of comorbidities; Used/uses medications; performed any surgical procedure; Using the IGB helped to acquire new habits; was satisfied with the use of the IGB; If they could have done something different to avoid regaining weight; would use the IGB again.
Result: In the present study, 150 patients treated with the IGB regained some weight, which corresponds to 68.49%. In the descriptive analysis of the variables that impact on weight regain, it can be observed in the group of patients in which there was weight regain that, in relation to nutritional monitoring, there was a decrease in 34% of patients who underwent this monitoring during treatment for after treatment, while in the group with no weight regain, this decrease was 28%. Psychological follow-up also showed a 50% drop between during and after treatment, but in both groups.
Conclusion: For treatment success, it starts with the acceptance and understanding that obesity is a disease, as well as an understanding of the harms that this condition brings throughout life. The change in habits must be progressive and constantly evaluated. Increasing consumption of fruits and vegetables, as well as increasing the practice of physical activity.
Keywords: Intragastric balloon; Lifestyle change; Obesity; Weight regain
Introduction
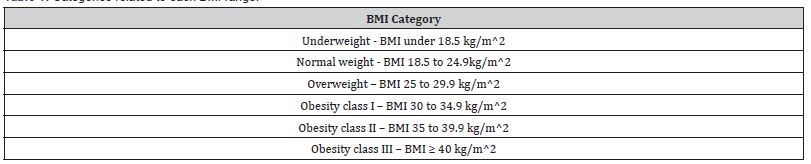
Obesity is a public health problem of global proportions that has shown alarming rates of growth, including among children and adolescents. Since 1980, the prevalence of overweight and obesity has doubled, and it is currently estimated that one third of the population is overweight [1]. According to the World Health Organization (WHO), in 2015, more than 1900 million adults, aged over 18 years, were identified as overweight, of which more than 600 million were obese. The projection is that, in 2025, around 2.3 billion conditioned adults will be overweight: and more than 700 million obese [2,3]. In 2018, Brazil reached the highest prevalence of obesity in the last 13 years, with 19.8% of adults in the country being classified as obese. This percentage grew 67.8% between 2006 and 2018. Taking into account the prevalence of overweight, the scenario is worrying, given that in the group of 26 capitals and the Federal District, the frequency of overweight was 55.7 % [4]. A simple and effective index for diagnosing nutritional status is the Body Mass Index (BMI), which is calculated by dividing body weight in kilograms by the square of height in meters. An individual with a BMI ≥ 30 kg/m2 is considered obese [5] (Table 1).
Table 1: Categories related to each BMI range.
The basis for combating overweight and obesity is found in the promotion of healthy eating and the practice of physical activity. Therefore, the clinical approach is based on a multidisciplinary treatment that seeks to change the lifestyle [5]. Due to this fact, there are many difficulties to carry out a successful intervention. The clinical treatment of obesity has very expressive success rates, but with a very high recurrence rate. The Intragastric Balloon (IGB) is an option for these patients. The natural history of obese patients is cyclic, with moments of success and failure of clinical treatment. Many studies [6-8] show successful weight loss after using IGB for approximately 6 months, another study shows long-term weight gain in a large cross-section of patients treated with IGB [9]. However, no study analyzed the factors that led to weight regain in these patients after the removal of the IGB. This study aimed to assess the factors of long-term weight gain in patients treated with IGB.
Methodology
For the present study, the data used were approved by the Research Ethics Committee (Brazilian equivalent to the Research Ethics Committee) of the Federal University of Minas Gerais (CAE no 42995915.4.0000.5132), as part of the postgraduate program in Science of Adult Health. Data were selected from individuals seen at a private outpatient medical center for the obese. All patients were certified by telephone and invited to participate in the study. Inclusion criteria for the study were: correct and truthful completion of the questionnaire (Table 2), use of IGB for at least 5 months, absence of bariatric surgical procedure after removal of the IGB, and no history of pregnancy after removal of the IGB. Data from 219 patient records were validated, which were submitted to a semi-structured interview, personally obtained by professionals trained for physical anamnesis and qualitative assessment of the treatment. Conscripted patients were divided into groups according to post-discharge follow-up time, 2 years (n = 28), 3 years (n = 114) and 4 years (n = 77).
Concepts and Procedures
In data collection, the term followed up with a nutritionist/ psychologist was defined as follows, as if the patient was followed up, during use of the balloon, and at least one year after removal. The practice of physical activity was validated if the patient practices at least 30 minutes of daily physical activity. The term presents comorbidities as if the patient has two or more diseases related to obesity. The term drug use refers to patients who were using drugs to control chronic diseases, such as diabetes and high blood pressure. The term undergoing surgery refers to any type of surgery, except bariatric ones. Besides that, if the use of IGB helped the patient to acquire new habits as if the patient acquired a balanced diet with regular exercise practices. All collected data were transferred to an Excel spreadsheet (Microsoft) and later transferred to the statistical package STATA (Version 13.0). Frequency of all data was performed to analyze possible outliers.
Result
In the present study, 150 patients who put the IGB on regained weight, which corresponds to 68.49%. In the descriptive analysis of the variables that impact weight regain, (Table 3), it can be seen in the group of patients in which there was weight regain that, in relation to nutritional monitoring, there was a decrease in 34% of patients who underwent this follow-up during treatment for after treatment, while in the group with no weight regain, this decrease was 28%. Psychological follow-up also showed a 50% drop between during and after treatment, but in both groups. The percentage of individuals who stopped practicing physical activity was higher in the group of patients who regained weight.
Table 2: Instrument for collecting the variables that impact weight regain
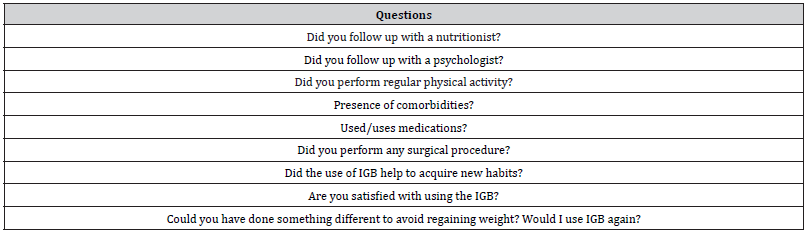
Table 3: Percentage distribution of the sample for statements investigated as variables that impact weight regain
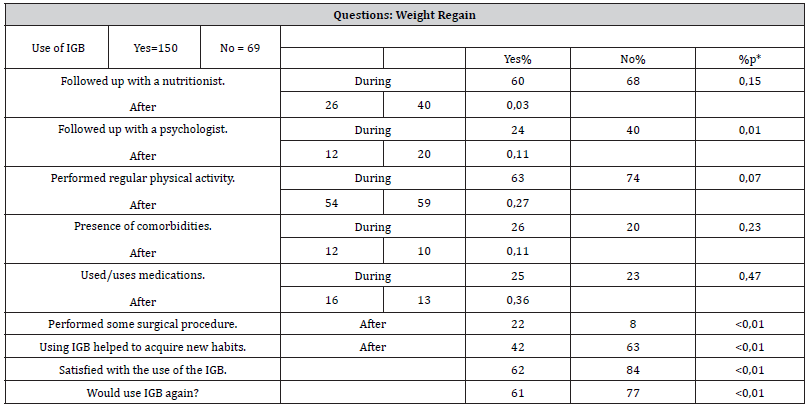
In the group in which there was no weight regain, the percentage of patients who stated that the use of the IGB helped to acquire new habits was 21% higher than in the group in which there was weight regain. Among the patients who reported not having acquired new habits, 45% and 73% of them did not follow up with a nutritionist during and after treatment, respectively. Regarding the new procedure, 61% who had regained weight and 77% of patients who had not regained weight, said they would undergo it again. More than 50% in both groups were satisfied with the treatment.
Discussion
For treatment success, it starts with the acceptance and understanding that obesity is a disease, as well as the understanding of the harm that this condition brings throughout life. Psychological and family support is essential, as it involves changing behavior and lifestyle habits. The triggering of depressive symptoms and anxiety crises can lead to weight fluctuations and treatment dropout [10,11]. In addition to the psychological approach, strategies compatible with the reality of each individual should be tried. Very complex diets and very intense physical training plans tend to fail. Changing habits must be progressive and constantly evaluated. The schemes below depict some practices that can be adopted so that obesity and overweight are treated and even prevented:
Increasing consumption of fruits*, vegetables** and legumes***
Consume daily:
3 servings of fruits and 3 servings of vegetables.
Consume fruits, vegetables for breakfast, snacks and/or dessert.
Consume fruits, vegetables and raw vegetables with peel and pomace, whenever possible.
Scheme 1 - Guidelines on food consumption (*Fruits: acerola, cashew, orange, apple, banana, papaya, etc. **Leaf Vegetables: watercress, lettuce, chicory, kale, cauliflower, spinach, mustard, cabbage, etc. ***Vegetables: carrots, beets, zucchini, pumpkin, etc.).
Source: Manual of Guidelines for Combating Obesity in Supplementary Health.
Increasing Physical Activity Practice
Children and young people: 5 to 17 years old
Minimum 60 minutes of physical activity of moderate * to ** intensity daily.
Young and Adults: 18 years or older
Minimum of 150 min of moderate-intensity aerobic physical activity per week. In individuals with physical limitations, stays as physically active as possible.
Scheme 2 - Guidance on the practice of physical activity (*Eg walking, dancing, swimming, etc. **Eg running, tennis, incline cycling, etc.).
Source: Manual of Guidelines for Coping with Obesity in Brazilian Supplementary Health 2017.
We conclude that the treatment with the balloon is expected to decrease body mass, as long as a negative energy balance is achieved. However, there is much disagreement about the best way to promote this caloric reduction. In this sense, the importance of a multidisciplinary work involving professionals in the nutritional area is highlighted. The reduction in caloric intake should be associated with measures to increase caloric expenditure and, whenever necessary, with drug treatment [11].
To read more about this article...Open access Journal of Gastroenterology & Hepatology
Please follow the URL to access more information about this article





No comments:
Post a Comment