Authored by Melissa G Hunt*,
Introduction
Background: IBS is a highly prevalent, chronic gastrointestinal (GI) disorder of gut-brain interaction that can lead to considerable distress and disability. Although IBS does not respond particularly well to standard medical care, empirically supported treatments exist, including CBT and the low FODMAP diet. Many patients with IBS seek self-help and adjunctive treatments to supplement traditional medical care. Therefore, it is important to rigorously test some of those publicly available options to see if they provide measurable benefit to consumers.
Aims: This study compared the efficacy of 2 self-help books (one cognitive-behavioral therapy or CBT book and one low FODMAP diet book) for irritable bowel syndrome (IBS).
Method: This study was a randomized, controlled, optional cross-over, single-blind, non-inferiority trial of 2 popular self-help books with 3 months of longitudinal follow-up. The books were Reclaim Your Life from IBS and The Complete Low FODMAP Diet Book.
Result: Immediately post-treatment, participants in both conditions showed significant improvement in health-related quality of life (HRQL), GI symptom severity, catastrophizing, anxiety about visceral sensations, and depressive symptoms. There were no significant between-group differences at post-treatment in HRQL; although, the low FODMAP group did show greater declines in GI symptom severity. By 3-month follow-up, both groups continued to show significant improvement over baseline in HRQL, and there were no significant between group-differences on any measure.
Conclusion: Reading either book with no professional guidance resulted in substantial improvement in patients with self-reported IBS.
Keywords: Irritable bowel syndrome; Cognitive behavioral therapy; Low FODMAP diet; Health related quality of life; Self-help
Introduction
Irritable bowel syndrome (IBS) is a highly prevalent, chronic gastrointestinal (GI) disorder of gut-brain interaction that can lead to considerable distress and disability. When strict diagnostic criteria based on the Rome IV consensus [1] are used, prevalence rates approach 6%. However, self-reported IBS is 3 times more prevalent, and is associated with similar health care utilization and impaired health related quality of life (HRQL), and even greater impact on absence from work [2]. IBS with predominant diarrhea (IBS-D) in particular is associated with impaired HRQL, significant occupational and social impairment, and substantial indirect costs [3].
From a medical perspective, first-line treatments for IBS typically include lifestyle changes followed by supplementation with soluble fiber, osmotic laxatives or polyethylene glycol for constipation, loperamide for diarrhea, and antispasmodics such as hyoscyamine for cramping abdominal pain, with the addition of neuromodulators such as amitriptyline if necessary [4]. Unfortunately, standard medical care is often insufficient to obtain both symptom relief and restoration of quality of life, and both patients and their physicians show low levels of satisfaction with the outcomes [5, 6]. Indeed, concurrent psychological distress is often the best predictor of HRQL long term, over and above GI symptoms themselves [7, 8].
The vast majority of patients with IBS believe that diet is directly linked to their symptoms [9]. As a result, many turn to restrictive and elimination diets in an attempt to manage their IBS. Unfortunately, fear and avoidance of food are associated with increased symptom severity and reduced HRQL overall [10]. Most restrictive diets (e.g., lactose or gluten free) do little to improve IBS symptoms over and above placebo response rates [11, 12].
One possible exception is the low FODMAP diet, which restricts all fermentable carbohydrates that are co-digested by symbiotic bacteria in the gut [13]. FODMAPs (Fermentable Oligosaccharides, Disaccharides, Monosaccharides And Polyols) are a series of short-chain carbohydrates that are poorly absorbed by the small intestine and ferment in the gut [14]. The low-FODMAP diet requires eliminating a wide array of foods including legumes, dairy, wheat, onions and garlic, and many fruits and vegetables. Such foods do reliably increase the gas and water contents of the gut, which is problematic in the context of the visceral hypersensitivity experienced by patients with IBS [15-16]. Eliminating high FODMAP foods does lead to reductions in GI symptoms, and thus potentially improved quality of life [17-19].
Unfortunately, the low-FODMAP diet presents many challenges. It is very difficult to follow, especially without professional guidance and can compromise nutrition [20], especially without adequate support from a knowledgeable dietician. Even when implemented correctly, it can also lead to increasing dysbiosis [21, 22]. It can also substantially interfere with social eating and traveling [23] and is almost impossible to follow for patients who do not control their own food production, such as college students eating in cafeterias. Nevertheless, many, if not most patients with IBS have at least tried the low FODMAP diet at some point, often simply googling information about it [24]. There are numerous consumer-oriented books for sale that enumerate the basic principles of the low- FODMAP diet and provide recipes and sample meal plans. One such book, The Complete Low-FODMAP Diet by Sue Shepherd and Peter Gibson was written by the originators of the approach. Far better than a simple one-page handout of forbidden or allowed foods, the book provides the rationale and some structure and guidance for individuals interested in trying to follow the low-FODMAP diet. Importantly, the book encourages the systematic, phased re-introduction of high FODMAP foods after 6 weeks, potentially resulting in a less restrictive diet long term, which is important for long term maintenance [25].
The other main IBS treatment approach comprises psychotherapies targeting psychological processes and the gut-brain interface [26], including gut directed hypnotherapy [27] and cognitive behavioral therapy [28]. CBT has been tested rigorously in a number of randomized controlled trials, and typically results in substantial improvement in GI symptom severity and health related quality of life, gains which are typically maintained and consolidated over time [28-30]. CBT for IBS typically includes psychoeducation about the gut-brain axis, the role of stress and arousal in exacerbating GI symptoms, relaxation training, the role of visceral hypersensitivity, and the degree to which experiential and behavioral avoidance maintain and exacerbate disability and distress. The efficacy of CBT for IBS has been shown to be partially mediated by reductions in visceral anxiety and sensitivity [31, 32] and by reductions in maladaptive, illness related cognitions [33] and GI specific catastrophizing [34]. Exposure to IBS symptoms and related situations seems to be a core component of effective treatment [35] and works in large part by reducing gastrointestinal specific anxiety [36].
Despite the efficacy of CBT for IBS, there are significant barriers to access and dissemination, including the cost of treatment and the lack of sufficient numbers of practitioners knowledgeable about both GI processes and CBT [37, 38]. Several smartphone applications offer self-help versions of psychological approaches to IBS. One, the Nerva App, delivers gut directed hypnotherapy. The other, Zemedy, delivers a full CBT for IBS protocol, and also incorporates some gut directed hypnotherapy scripts, mindfulness and attention training. Zemedy was found to be efficacious in an RCT against a waitlist control [39]. Despite the increasing popularity of apps, self-help books remain in high demand [40]. Reclaim Your Life from IBS [41] is a self-help CBT protocol for IBS written for consumers. A randomized, controlled clinical trial prior to publication demonstrated its efficacy as a standalone self-help therapy with no therapist guidance [34].
Overall, there is considerable evidence that guided self-help interventions for IBS can be quite effective [42], but it remains unclear which interventions patients should choose. In particular, the low FODMAP diet and CBT for IBS work via opposite and competing mechanisms. The low FODMAP diet attempts to eliminate the sensations to which people with IBS are hypersensitive (by restricting foods that increase those sensations). CBT attempts to reduce the underlying hypersensitivity itself (by changing catastrophic cognitions and anxiety, and reducing avoidance, including avoidance of foods and sensations). Thus, testing the two leading self-help books in each domain directly against each other might be expected to yield useful information about relative efficacy, as well as potential moderators and mediators of treatment outcome.
The current study compared the impact of The Complete Low- FODMAP Diet and Reclaim Your Life from IBS on GI symptom severity, HRQL and depressive symptoms in a randomized, controlled, single-blind, optional cross-over, non-inferiority trial with three-month longitudinal follow-up. We predicted that the diet book would result in greater reductions in GI symptom severity short term, but that the CBT book would result in greater reductions in catastrophizing, visceral anxiety and depression short term. Long term, we expected fear of food to decrease in the CBT condition, but not in the diet condition. We expected both books to result in improved HRQL, but via different mechanisms.
Material and Method
Participants
Participants with self-reported IBS were recruited through online messages and posts on IBS support group websites (Reddit, HealingWell, Facebook etc.) along with in-person recruitment at a gastroenterology department at a major university hospital medical center. A total of 176 potential participants completed informed consent online prior to completing baseline screening measures. Twenty-seven people met exclusion criteria, leaving 149 who met inclusion criteria and were offered randomization. Twenty-six of those individuals were lost to follow-up prior to randomization. A total of 123 (the intent-to-treat sample) were randomized via the coin toss function of random.org. Sixty-seven participants were assigned to the CBT condition and 56 were assigned to the diet condition. The allocation sequence was concealed to participants until they were enrolled and assigned to the intervention. Research personnel remained blinded throughout the intervention, followup and data cleaning and analysis phases. See (Figure 1) for Consort Diagram of participant flow throughout study. See (Table 1) for participant demographics
Figure 1:Consort Diagram.
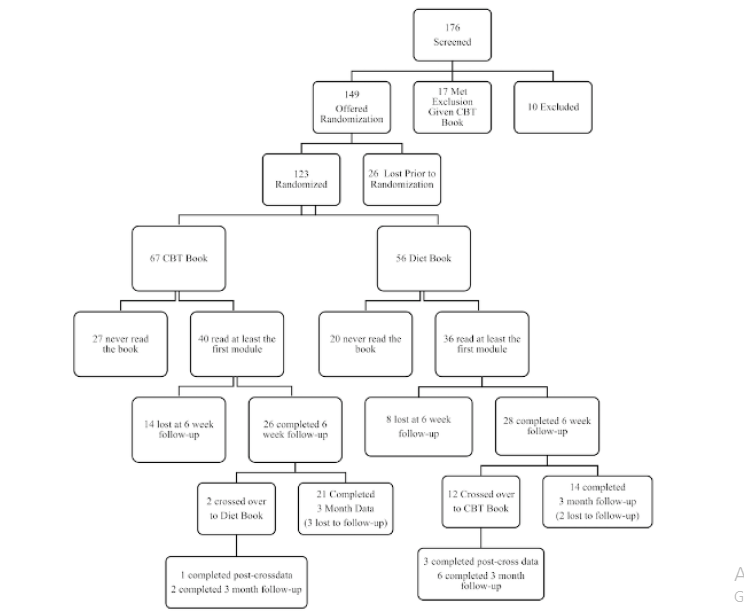
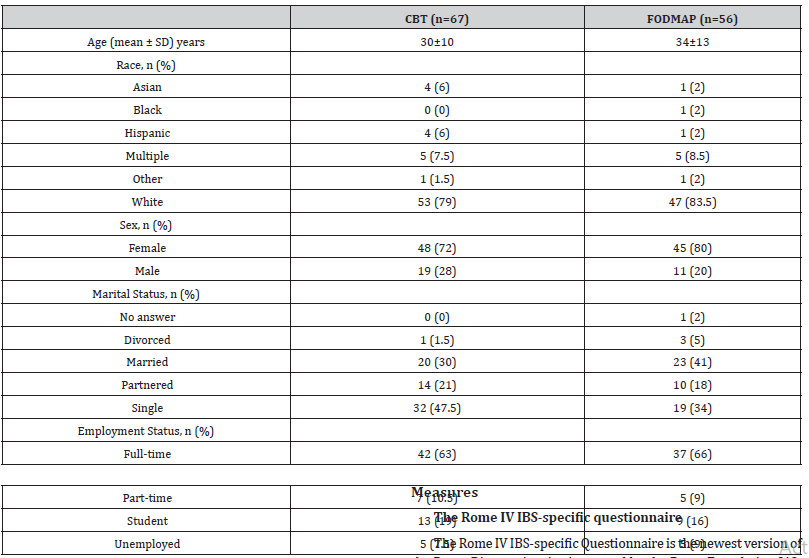
Table 1:Participant Demographics.
Inclusion and exclusion criteria
Inclusion criteria included being at least 18 years of age and reporting a previous IBS diagnosis from a medical professional. Exclusion criteria included reporting any other GI disorder (e.g., celiac disease, inflammatory bowel disease), and/or current pregnancy. Participants who reported currently following a strict low FODMAP diet for at least 6 weeks or having tried the diet fully for at least 6 weeks in the past were also excluded but were offered a copy of Reclaim Your Life from IBS at no cost. Recruitment occurred between 2016 and 2018. Thus, many participants may have been originally diagnosed under Rome III criteria. However, all but 2 fulfilled stringent Rome IV diagnostic criteria by self-report.
Blinding
The protocol utilized a single blind design, since it was impossible to blind participants to which book they were reading. The blind was managed by a research assistant who was not affiliated with the study and an administrative assistant in the lead author’s department. Study personnel randomized each incoming participant to “book 1” or “book 2” and informed the unaffiliated assistant of the assignment. The assistant then gave the participant’s contact information and book assignment to the administrative assistant, who ordered the correct book from Amazon, shipped directly to the participant. All data were cleaned and analyzed fully blinded to study personnel. The blind was only lifted once the data set was locked and all primary analyses were completed.
Measures
The Rome IV IBS-specific questionnaire
The Rome IV IBS-specific Questionnaire is the newest version of the Rome Diagnostic criteria created by the Rome Foundation [43; 1]. For brevity, a modified, 13-item version of the questionnaire was used, including all items necessary to determine if the participant reported current symptoms consistent with a diagnosis of IBS. It also allowed calculation of severity score. Note that many individuals enrolled in the study would have been diagnosed by their physician using older Rome III criteria.
Gastrointestinal symptom rating scale - IBS (GSRS-IBS)
GI symptom severity was measured using the GSRS-IBS. This 13 item self-report scale has five dimensions: bloating, diarrhea, constipation, pain, and satiety [44]. Participants rate how much they have been bothered by a specific symptom in the past week, on a scale of 0 (no discomfort at all) to 6 (very severe discomfort). Possible scores range from 0 to 78, with higher scores reflecting greater symptom severity. Each dimension has demonstrated high internal consistency, with Cronbach’s alpha ranging from 0.74 (pain) to 0.85 (satiety) [44]. The scale also demonstrates high testretest reliability between the five factors (all r = 0.55 to 0.70), and high construct validity [44].
Irritable bowel syndrome quality of life (ibs-qol)
The IBS-Qol contains 34 self-report items rated on a 5-point Likert scale ranging from 1 (not at all) to 5 (a great deal/extremely) [45]. The items are summed and then transformed such that final scores range from 0 to 100, with higher scores reflecting more impaired quality of life. The IBS-Qol has been demonstrated to have high internal consistency (Cronbach’s a = 0.95), high test–retest reliability (ICC= 0.86), and a good construct validity [45].
Visceral sensitivity index (VSI)
The VSI is a widely used unidimensional 15-item scale measuring GI symptom-specific anxiety. terms are totaled with a range of scores from 0 to 75, with higher scores reflecting greater anxiety [46]. Preliminary and follow-up studies found high internal consistency for the VSI, reporting a Cronbach’s alpha of about 0.93 and mean inter-item correlation of 0.47, along with a good criterion, construct, and predictive validity [46].
Gastrointestinal Cognitions Questionnaire (GI-Cog)
The GI-Cog comprises 18 self-report items rated on a 5-point Likert scale, ranging from 0 (hardly) to 4 (very much). Items are totaled, and scores range from 0 to 64, with higher scores reflecting more catastrophic thinking. The GI-Cog has been shown to have a high internal consistency (α = 0.92) and test-retest reliability (r = 0.87, p < .001), along with good criterion and construct validity [34].
Fear of food questionnaire (FFQ)
The FFQ is an 18 item self-report questionnaire measuring fear, avoidance of food, and life interference and loss of pleasure from restrictive eating [47]. Items are rated on a 6-point Likert scale ranging from 0 (not at all) to 5 (absolutely). Scores range from 0 to 90, with higher scores reflecting more fear of food. The FFQ has been found to have good factor structure, high internal consistency (α = 0.95), high test-retest reliability (r = 0.93, p < .01), and good validity, including known-groups validity.
Beck depression inventory (BDI)
The BDI is a widely used depression measure that assesses symptom severity and is sensitive to treatment gains [48]. A total of 21 items are rated from 0 to 3 in terms of intensity. Total scores range from 0 to 63, with higher scores reflecting more severe depressive symptoms. The BDI demonstrates high internal consistency (α = 0.94), and good test-retest reliability (r = 0.93) in the absence of treatment [49].
Weekly quizlets
In order to assess engagement with the material and measure “dose,” participants were asked to complete brief, humorous quizlets every week for the 6 weeks of treatment implementation. Questions covered general themes from the week’s reading material. Quiz completion was used to assess progress through the material, while quiz scores were used to assess engagement with the material.
Procedures
Participants were emailed a link (if recruited in-person) or followed a link in an online post (if recruited via social media) to the consent form and baseline questionnaires. They read the consent form online and consented by clicking the “I consent” radio button and were then directed to questionnaires. The study team then confirmed that they were at least 18 years old, not pregnant, did not have a comorbid GI disorder, and that they had never seriously tried the low-FODMAP diet for 6 weeks or more. They were then randomly assigned to receive Reclaim your Life from IBS (CBT condition) or the Complete Low-FODMAP Diet workbook (diet condition). Participants had 6 weeks to complete their assigned book, and weekly quizlets were emailed to confirm their continued participation. At 6 weeks (post-treatment), participants completed another round of the same measures administered at baseline. Participants were then offered a chance to cross over and receive the other book. Three months after post-treatment assessment, participants were asked to complete the same measures again.
Interventions
Reclaim Your Life from IBS [41]
Reclaim Your Life from IBS was written to function as a standalone CBT treatment protocol with no therapist involvement. In a previous RCT against a waitlist control, it yielded significant improvement in HRQL and GI symptom severity, mediated by reductions in GI-specific anxiety and catastrophizing [34]. The book takes a fairly standard cognitive behavioral approach, starting with psychoeducation and relaxation training, then introducing the cognitive model and applying it to IBS, recognizing and overcoming avoidance and encouraging behavioral experiments, and progressing to exposure to feared situations and sensations.
Chapter 1:Differential Diagnosis, defines IBS and discusses important differential diagnoses, including lactose intolerance, celiac disease, and the inflammatory bowel diseases. It encourages readers to review their medical history and confirm their IBS diagnosis with their doctor.
Chapter 2:The Biopsychosocial Model of IBS, explains the etiology and maintenance of IBS to give a clear treatment rationale for targeting its emotional and behavioral components. Patients are reassured that physical symptoms are indeed real, but that the gut is highly reactive to stress and sympathetic arousal through numerous biological mechanisms.
Chapter 3:Relaxation Training, provides instructions for diaphragmatic breathing, progressive muscle relaxation, and imagery. It encourages readers to practice each of the three different approaches and to pick the one (or two) that work best and use them daily.
Chapter 4:The Cognitive Model of Stress Management, introduces the cognitive model of stress, including identifying situations, thoughts and feelings, and begins to teach how to identify distorted beliefs and review the evidence for and against them.
Chapter 5:Applying the Cognitive Model to IBS Symptoms, instructs users to identify IBS specific catastrophic beliefs, to consider benign alternatives, and to evaluate the evidence for and against various beliefs. An example of an IBS-specific distorted belief is “If I get up to use the bathroom in the middle of a movie, everyone around me will be exceedingly annoyed.”
Chapter 6:Behavioral Experiments, challenges readers to engage in some behavioral experiments and to test their predictions for certain situations. An example would be to go to a movie theater, sit in the back, and observe how many people actually get up during the movie and how others react to them, followed by intentionally getting up a few times themselves.
Chapter 7:Eliminating Avoidance, focuses on behavioral avoidance and encourages graded exposure to feared situations. For example, an individual who fears being trapped in the car and needing to get to a bathroom might try driving around their neighborhood for 20–30 min until their anxiety habituates. After successfully completing that behavior, they are encouraged to gradually expand the range until they can drive to a meeting an hour away with their boss.
Chapter 8:Diet and IBS, reviews the scientific evidence for and against the often-contradictory advice about using diet to manage IBS. It encourages a healthful, whole foods diet that mixes soluble and limited insoluble fiber and discourages people from “demonizing” particular “danger” foods or food groups.
Chapter 9:Summary and Review, reviews the treatment and provides encouragement and suggestions for relapse prevention and further improvement.
The Complete Low-FODMAP Diet [50]
The Complete Low-FODMAP Diet, written by originators of the approach, is a comprehensive approach that explains the rationale behind the restrictions and maps out a detailed plan for a strict elimination phase, followed by careful, phased re-introduction of foods. Part One of the book explains how the low-FODMAP diet can help relieve IBS symptoms and outlines how to follow the diet. Part Two of the book features a wide range of low-FODMAP recipes with clear instructions and appealing photos of finished dishes. As was the case in the CBT self-help book condition, they knew they had 6 weeks to complete the workbook and implement the diet, but they were not given any strict schedule for reading the book.
Part I
Chapter 1:How Food Can Trigger Gut Symptoms, introduces different types of GI disorders, such as Inflammatory Bowel Disease, Celiac Disease, and IBS, and explains how different foods are digested and affect GI symptoms and sensations.
Chapter 2:What is IBS?, outlines causes, symptoms, and treatment of IBS. The causes and symptoms of IBS are explained, and treatment options for the syndrome are outlined.
Chapter 3:All About the Low-FODMAP Diet, defines what FODMAPs are, and then explains that poor absorption in the gut has been proven to be linked to IBS symptoms.
Chapter 4:Implementing the Low-FODMAP Diet, outlines different methods of beginning the low-FODMAP diet, including the wisdom of consulting with a registered dietitian. It also overviews appropriate reintroduction of FODMAP foods.
Chapter 5:Putting the Low-FODMAP Diet into Practice, offers tips on implementing meal substitutions, from beverages to baking, as well as guidelines for low-FODMAP for vegans and vegetarians, children, and patients with Diabetes or Celiac Disease.
Chapter 6:Low-FODMAP Menu Plans, comprises various Low-FODMAP menu examples, including lacto-ovo vegetarian, vegan, low-fat, dairy-free, and more.
Chapter 7:Making Low-FODMAP Diet Easier outlines helpful tips on learning how to avoid FODMAP foods, including tips for reading food labels. It lists specific foods that must be avoided in certain situations, as well as suitable and to-avoid food additives.
Chapter 8:Special Occasions and the low-FODMAP diet, focuses on how to handle eating at restaurants or friends’ homes, hosting parties, and traveling while on the low-FODMAP diet. It suggests calling ahead to restaurants to learn more about menu items and bringing food from home when eating out. It provides party menu suggestions and substitutes to bring to restaurants.
Part II
The balance of the book is a traditional cook-book format with sections on appetizers, salads, soups and stews, casseroles and baked dishes, pasta, noodles and rice, a variety of entrées, breads and baked goods, cookies and bars, cakes and tarts, puddings, custards and ice cream.
Result
Baseline characteristics
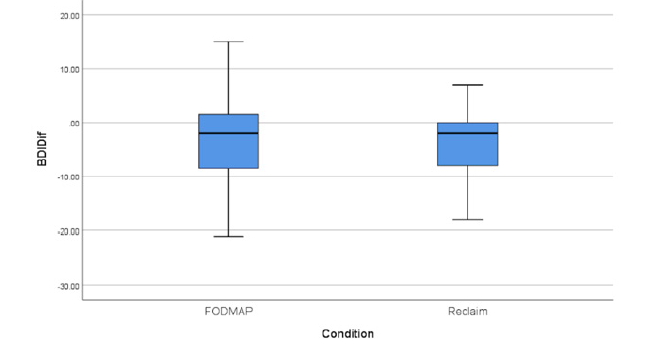
At baseline there were no significant between-group differences on the primary measures of HRQL and GI symptom severity or on fear of food or visceral anxiety [all t (121) < 1.2, all ns]. However, there were significant differences in GI-specific catastrophizing and depression, with participants in the CBT group showing slightly higher scores on average on both measures [t (121) = 2.06, p = .04 and t (121) = 2.19, p = .03 respectively]. Thus, baseline symptoms were controlled in all analyses. While the design should have yielded low risk of bias from randomization, the slight differences at baseline suggest some concerns about randomization, according to the Cochrane risk of bias tool [51]. There were several univariate outliers at baseline (standardized residual < -3 or > 3) including one individual with very low Rome severity, two with very low visceral anxiety and one with a high depression score. None of them proved to be multivariate outliers, however, so their data were retained in all analyses. On average, the sample was in the moderate range of distress across HRQL, GI symptom severity, visceral anxiety, and catastrophizing. 27% of the sample endorsed mild depressive symptoms (BDI > 13), with 22% endorsing moderate symptoms (BDI > 20) and another 17% endorsing severe depressive symptoms (BDI > 30). See (Table 2) for all outcome measure means at Baseline and Post-Treatment, as well as at 3-month follow-up for individuals who elected not to cross over. See (Figures 2-7) for graphs of change scores from baseline to post-treatment by condition.
Table 2:Outcome Measures at Baseline, Post-Treatment and 3 Month Follow-Up.
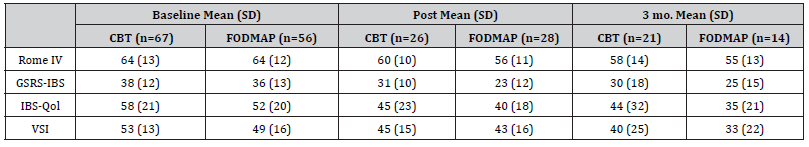
Figure 2:Change in HRQL.gure 1: Consort Diagram.
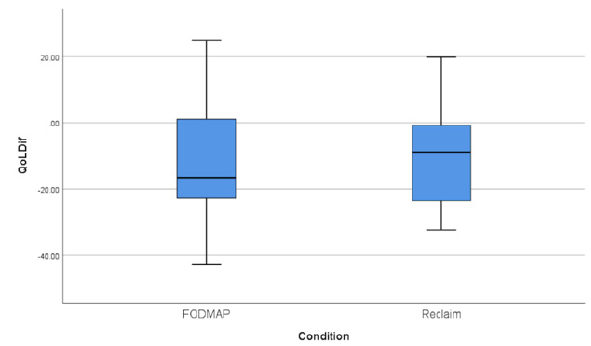
Figure 3:Change in GI Symptoms.
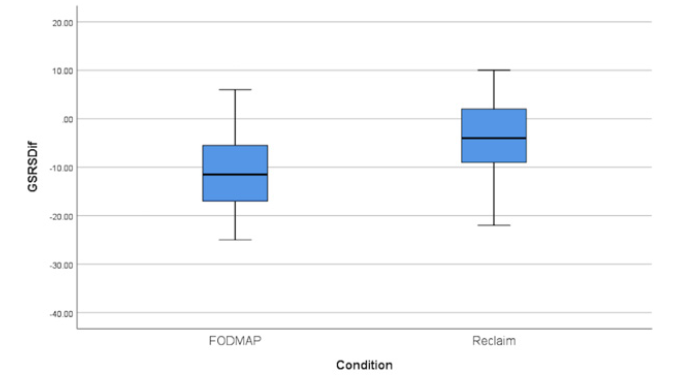
Figure 4:Change in Catastrophizing.
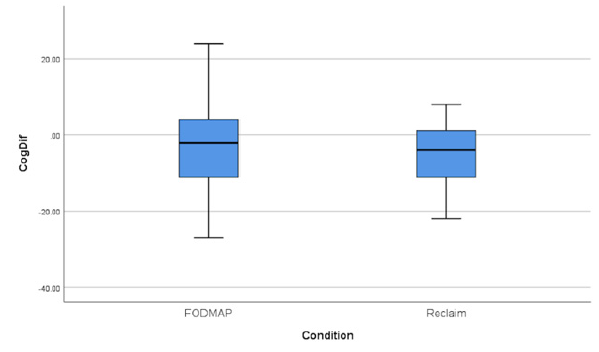
Figure 5:Change in Visceral Anxiety.
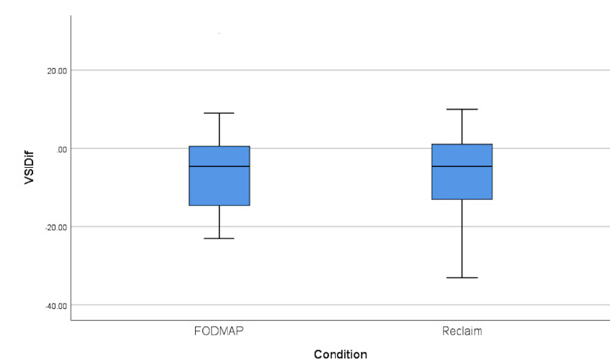
Figure 6:Change in Fear of Food.
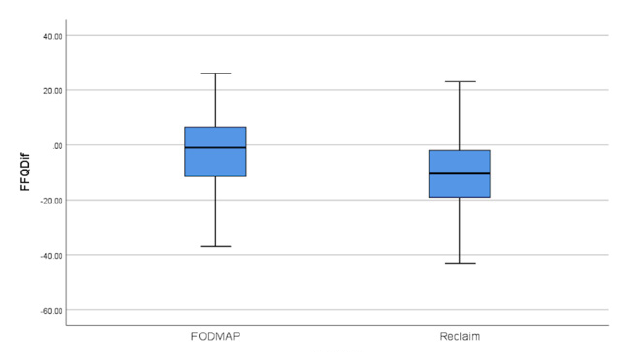
Figure 7:Change in Depressive Symptoms.
Attrition
There was significant attrition during the study, as expected from an online study of a self-help treatment. In the CBT condition, 27 individuals never completed any quizlets and were lost to followup. Another 14 participants completed at least the first quizlet but were lost to follow-up at post-treatment. Two individuals elected to cross over to the diet book, both of whom completed the 3-month follow-up. Of the 24 who did not, 3 were lost to follow-up at 3 months. Thus, of the 67 participants initially randomized to the CBT condition, only 39% completed the post-treatment survey and only 34% completed the three-month survey. In the diet condition, 20 individuals never completed any quizlets and were lost to followup. Another 8 participants completed at least the first quizlet but were lost to follow-up at post-treatment. 12 individuals elected to cross over to the CBT book, 6 of whom were lost to follow-up at 3 months. Of the 16 who did not, 2 were lost to follow-up at 3 months. Thus, of the 56 participants initially randomized to the diet condition, only 50% completed the post-treatment survey and only 36% completed the 3-month survey. Chi-square tests of attrition across condition were non-significant. Several baseline characteristics were associated with attrition at post-treatment. Those who dropped out were more depressed [t (121) = 2.28, p = .02], had worse GI symptoms [t (121) = 2.20, p = .03] and were marginally more prone to catastrophic cognitions [t (121) = 1.90, p = .06]. None of the baseline or post-treatment variables predicted attrition at 3 months.
In most clinical trials, multiple imputation would be used to account for attrition and allow for full intent-to-treat analyses. In this case, doing so would simply confound the acceptability of the treatments with the efficacy of the treatments. It may be that about half of individuals who pick up or buy a self-help book for IBS never make much progress with it, and this simply reflects how selfhelp books are used (or not) in the real world. Of course, it is also possible that some participants simply wanted the free book and never really intended to participate in the trial. This is a separate question from whether individuals who actually start reading and working through the book can benefit from it substantially. Thus, a strategic decision was made to report both detailed attrition results (to gauge acceptability) and completer analyses (to gauge efficacy), but not to report multiple imputation results, which confound the two.
Post-Treatment
First, paired-sample t-tests were conducted separately for each group to gauge change across all outcome measures from baseline to post-treatment. The diet group showed significant improvement on both primary outcome measures of HRQL [t (27) = 3.51, p = .002] and GI symptom severity [for the GSRS, t (27) = 5.17, p < .001, for the Rome IV t (27) = 4.45, p < .001]. They also showed significant reductions in visceral anxiety [t (27) = 2.57, p = .016]. However, they showed only marginally significant improvement in catastrophizing [t (27) = 1.72, p = .097] and depression [t (27) = 1.91, p = .067]. Unsurprisingly, their fear of food did not change significantly [t (25) = 0.87, p = .39].
The CBT group showed significant improvement on HRQL [t (25) = 3.51, p = .002] and GI symptom severity as measured by the GSRS [t (25) = 2.35, p = .027] but not as measured by the Rome IV questionnaire [t (25) = 1.42, p = .17]. However, the CBT group showed significant improvement on all other measures, including visceral anxiety [t (25) = 3.15, p = .004], catastrophizing [t (25) = 2.70, p = .012], depression [t (25) = 2.21, p = .037] and fear of food [t (25) = 3.11, p = .005].
Univariate analysis of covariance, including the baseline measure as a control, revealed no significant between-group differences in HRQL at post-treatment, but did show a significant difference in GI symptom reduction as measured by the GSRS favoring the diet book [F(1,53) = 8.2, p = .006] and marginally as measured by the Rome IV questionnaire [F(1,53) = 3.18, p = .08]. There were no significant between-group differences on visceral anxiety, catastrophizing or depression. There was a marginally significant difference in fear of food favoring the CBT book [F (1,53) = 2.89, p = .095].
Clinically significant change/
In terms of clinically significant change we used Criterion B (falling within 2 SD of the healthy mean) which is more conservative than Criterion A (falling 2 SD below the pathological mean) [52]. For GI symptoms, the mean GSRS score for healthy controls is 12 with a standard deviation of 11, leading to a cut point of 34. In the CBT group, 14 of 26 participants (54%) met this criterion at posttreatment. In the diet group, 24 of 28 (86%) met this criterion at post-treatment. For HRQL, the mean IBSQoL score for healthy controls is 5 with a standard deviation of 11, leading to a cut point of 27. In the CBT group 7 of 26 (27%), and in the diet group, 6 of 28 (21%) met this criterion at post-treatment. Looked at another way, the qualitative range for minimal-to-mild impairment on the IBSQoL is 0-31. An additional 1 participant in each group would meet this slightly less stringent criterion, leading to a total of 31% of CBT group participants and 25% of diet group participants showing an excellent response. With respect to depressive symptoms, we examined change in categories of minimal, mild, moderate and severe symptoms. In the CBT group, of the 19 participants with at least mild depressive symptoms at baseline, 8 (42%) showed no change, while another 8 (42%) showed improvement and 3 (16%) showed worsening symptoms. In the diet group, of the 15 people who started with at least mild depressive symptoms, 5 (33%) showed no change, 8 (53%) showed improvement and 2 (13%) showed worsening symptoms.
Adherence
Our mechanism for judging adherence was completion of the weekly quizlets, each of which referenced material from one chapter of a participant’s assigned book. Unsurprisingly, participants who were lost to follow-up at post-treatment completed far fewer quizzes (M = 1.3, SD = 2.1) than those who continued to participate (M = 5.1, SD = 1.8) [t (121) = 10.64, p < .001]. However, there was no significant difference in quiz completion between groups for participants retained at post-treatment, with both groups completing on average about 5 of 6 quizzes. (For the diet book, M = 4.96, SD = 1.9; for the CBT book M = 5.19, SD = 1.6). This actually represents a fairly robust “dose” of treatment, especially for the CBT book. All of the major change elements in the book are covered by material in the first 5 weeks. The final week covers diet (and encourages eating as non-restrictive a diet as possible) and a summary chapter. Adherence did seem to matter to participants in the diet book condition. Quiz completion was correlated with reduction in both GI symptoms (r = -.57, p = .001) and depression (r = -.44, p = .018). For the CBT group, quiz completion was marginally significantly correlated with improvement in catastrophizing (r = -.37, p = .064), but not for any other measure.
There was a significant between-group difference in the overall quiz scores, with the CBT group generally scoring higher than the diet group [t (52) = 4.06, p < .001]. However, since the quizzes comprised different content from different sources, it is difficult to know what to make of this difference. For the diet group, quiz scores were significantly correlated with improvement in GI symptoms [r = .59, p = .001] and depression [r = .52, p = .005] and marginally correlated with improvement in HRQL [r = .36, p = .06] and reductions in catastrophizing [r = .32, p = .10]. For the CBT group, quiz scores were correlated with reductions in catastrophizing [r = .40, p = .045] but no other outcome measure.
Three-month follow-up for individuals who did not cross-over
Paired sample t-tests from post-treatment to 3-month followup revealed no loss of treatment gains for the CBT group across all measures [all t (17) < 1.0, all p >=.50]. For the diet group, there was no significant loss of gain on any measure. If anything, the group showed a trend toward further reduction in catastrophizing from post-treatment to 3-month follow-up [t (9) = 1.82, p = .10]. Univariate analysis of covariance, including post-treatment as a control, showed no significant between group differences at 3-month follow-up on any measure.
Optional cross-over results
Far more people who were initially assigned to the diet book elected to cross-over to the alternative book at post-treatment than people initially assigned to the CBT book [χ2 = 10.29, p = .001]. There were no significant differences in any measures at either baseline or post-treatment that predicted cross-over. Since only 2 CBT participants elected to cross over, no further analysis of their data was attempted. Of the 12 individuals who crossed over from the diet book to the CBT book, 6 completed 3-month follow-up data. For those 6 individuals, there was a significant reduction in fear of food from post-treatment, when they had only read the diet book, to 3 months, when they had a chance to read the CBT book as well [t (5) = 2.97, p =.031].
Discussion
The purpose of this study was to compare the efficacy of two evidence-based self-help books for IBS derived from two different empirically supported but competing approaches - CBT and the low FODMAP restrictive diet. Completer analyses found that both books yielded statistically and clinically significant improvement in the primary outcome measures of health-related quality of life and GI symptom severity. Moreover, both books resulted in significant improvement in depressive symptoms, catastrophizing and GI-specific anxiety, with gains typically maintained 3-months post-treatment. The only between-group differences at posttreatment were that the diet group showed greater reduction in GI symptom severity, while the CBT group showed marginally greater reductions in fear of food. Both of those between-group differences disappeared by 3-month follow-up, although participants who crossed over from the diet to the CBT book showed significant further reductions in fear of food.
In terms of clinically significant change, 54% of treatment completers in the CBT group and 86% of the diet group improved in GI symptom severity at post-treatment. For HRQL, about 30% of the CBT group versus 25% of the diet group significantly improved. These outcomes yield number-needed-to-treat (NNTs) of between 1.2 and 4. While these numbers may not be as robust as desired, it is nevertheless remarkable that two self-help books with no clinician guidance resulted in such substantial gains. Compare this to the NNT of 10 for rifaximin, an antibiotic commonly used to treat small intestine bacteria overgrowth and IBS [53]. It suggests that gastroenterologists would be well advised to recommend either (or both) of these books to patients to provide extra support and structure in medical treatment. This is particularly important given the expense and difficulty of accessing skilled CBT providers knowledgeable about GI issues, or registered dieticians knowledgeable about the low FODMAP diet.
This study was designed as a non-inferiority trial and did indeed demonstrate that both books were quite helpful overall, and equally helpful with respect to HRQL. However, it is worth noting that a large number of potential participants (27 in total) were excluded from the trial because they had previously tried and failed the low FODMAP diet. Excluded participants reported a range of experiences including finding the diet unhelpful, finding it very difficult to adhere to, or finding that it actually compromised quality of life despite reducing physical symptoms. Indeed, almost all of our participants reported having tried it to some extent in the past. Thus, our exclusion criteria actually introduced some pro-diet book bias into the study. We had already excluded individuals who had seriously tried and failed the diet in the past, or who were on it “successfully” but were still distressed by their IBS.
The study had several significant limitations. First, we did not require rigorous diagnostic interviewing and/or explicit physician confirmation of the IBS diagnosis. That said, only 2 participants failed to meet stringent Rome IV criteria by self-report, and both would have met Rome III criteria. This study was a test of 2 evidence-based self-help books publicly available through Amazon and other commercial book sellers. Book stores do not require physician confirmation of diagnosis prior to purchase of a selfhelp book for a condition the buyer believes they have. Thus, our sampling procedure and inclusion criteria drew from exactly the population of interest: people who believe they have IBS and are interested in self-help materials.
The second major limitation was attrition rate, which was substantial (but not significantly different) in both conditions. Studies of online behavioral health interventions typically have fairly high attrition rates (around 50%) [54]. The attrition rate was comparable for the diet book at post-treatment (50%) but higher for the CBT book (61%). Perhaps some participants simply wanted the free book and never planned to participate in further data collection, but it is also possible that these attrition rates are accurate estimates of how many people buy such a book and then never really read or follow it. Thus, self-help interventions with no clinician support or structure may only be useful to 40-50% of IBS patients. We elected not to attempt full intent-to-treat analyses using multiple imputation to account for missing data, as such an approach can inadvertently confound efficacy with acceptability. Self-help interventions may only be acceptable to about half of patients. Nevertheless, if used, the treatments are efficacious, and given the prevalence of IBS, such books could still benefit millions if recommended by GI doctors caring for patients with IBS.
The third limitation was our measure of treatment adherence. We sent participants brief, humorous “quizzes” every week to gauge progress through the material. Individuals retained to post-treatment completed on average 5 of the 6 quizzes in both conditions, which is a reasonable “dose” but may not reflect actual engagement with the material. Quiz completion was correlated with reduction in GI symptoms and depression in the diet group, and with reductions in catastrophizing in the CBT group, suggesting that the measure had some validity. However, it is notoriously difficult to measure the “dose” of a treatment like this. The fourth limitation was that despite having randomization procedures in place that should have minimized between group differences at baseline, the participants assigned to the CBT condition were significantly more depressed on average pre-treatment. This might help explain the puzzling finding that the CBT intervention was not more effective than the diet intervention at reducing depressive symptoms.
Conclusion
Despite its limitations, we believe this study is of significant value. It successfully demonstrated the efficacy of two competing evidence-based self-help books for IBS patients without any professional guidance, one focused on CBT, and the other on the low FODMAP diet. Although they presumably work via different mechanisms, both books resulted in statistically and clinically significant improvement in HRQL and GI symptoms, as well as depression, GI-specific anxiety, catastrophizing and fear of food. Of course, individuals who had previously tried and failed the low- FODMAP diet were excluded from the study, leaving the possibility that such individuals might do better with a CBT focused book. Selfhelp books are not restricted by geography, scheduling constraints, insurance, or the availability of GI knowledgeable CBT therapists or registered dieticians. Despite its relatively benign physical profile, IBS can be an extraordinarily debilitating condition. Finding novel ways to disseminate evidence-based, effective treatments to augment traditional medical care remains an important challenge, and both Reclaim Your Life from IBS and The Complete Low FODMAP Diet meet that goal.
To read more about this article...Open access Journal of Gastroenterology & Hepatology
Please follow the URL to access more information about this article





No comments:
Post a Comment