Authored by Errabi Mohammed Nizar*,
Introduction
Textiloma or Gossybipoma, is a very rare but well elucidated postoperative complication. Gossypiboma is made up of gossypium which means cotton (in Latin) and boma which means a hiding place (in Swahili). It is used to describe a foreign object made up of surgical pad(s) or sheet(s) left within the surgical site [1,2]. We report a case where surgical exploration came back negative, excluding the diagnosis initially made by CT scan which suggested the presence of a pre-hepatic textiloma.
Patient and Observation
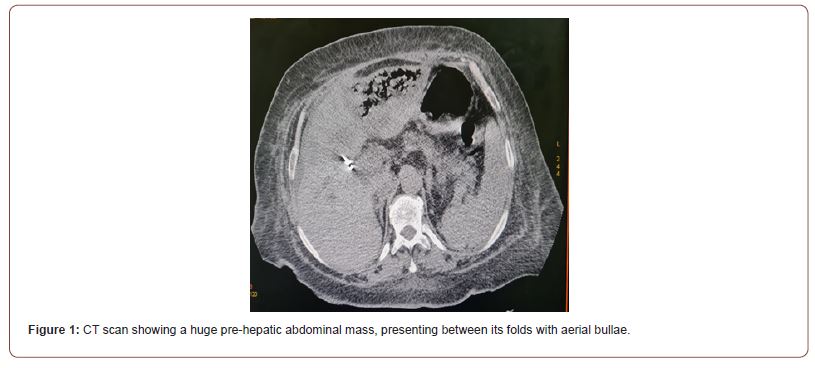
Mrs. Z.S, 71 years old, with no particular pathological history outside of a cholecystectomy, followed for a locally advanced peri hilar tumor (Klatskin) with pulmonary and hepatic metastases. The lesion was classified as Bismuth and Corlette type IIIa on MRI. The patient was referred to our visceral surgery department at the Moulay Ismail Military Hospital in Meknes, after failure of endoscopic biliary drainage by endoprosthesis. On admission, she had frank mucocutaneous jaundice, her GCS was 15/15, hemodynamically and respiratorily stable, apyretic with a normal digestive transit. The clinical examination found a slight tenderness of the right hypochondrium. The biological workup was strictly normal except for the elevation of the alkaline phosphatase level to 2.3 VN, the ALT was 191, the total bilirubin was 281 (predominantly conjugated) and the prothrombin rate was 81%. During the postoperative follow-up, in the short term (on day 4), the patient worsened her biological check-up with the reappearance of epigastric pain, abdominal bloating and sialorrhea, raising the suspicion of biliary peritonitis due to partial or total release of the drainage device. Thus, an abdominopelvic CT scan was performed (Figure 1), which revealed a small to medium-sized effusion, Redon’s drain still within the sectorial biliary convergence of the left liver, and an image of textiloma in the prehepatic area.
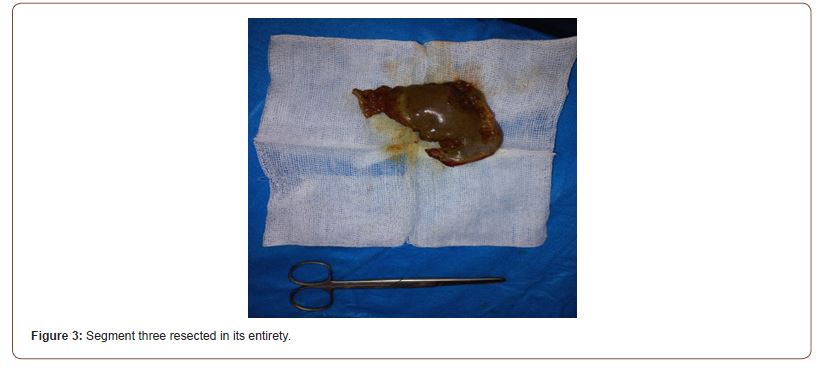
After a careful resuscitation adapted to her critical state, she was admitted to the operating room in emergency, for an exploratory laparotomy (by resumption of the right sub-costal approach) where we detected the true nature of the suspicious image in pre-hepatic, which corresponded to the sphacelic and infarcted segment 3 (Figure 2), suggesting an iatrogenic ligation of her feeder pedicle when digging towards the bile duct of the left paramedian segment along the round ligament. In the end, our procedure consisted of a segmentectomy (Figure 3), and a wide locoregional drainage of the bypass site by Salem Ch16 probe and Delbet blade. The postoperative course was simple and without any particularities with resumption of transit on the fourth postoperative day.
Discussion
Discus remains the surgeon’s dread during any procedure and the outcome for the patient can be dramatic, as its consequences are potentially serious (Diop, 2017). The frequency reported in the literature is 1/1000 to 1/10000 [3]. Clinical and radiological manifestations are variable, leading to diagnostic erraticities (Sar, 2018). Computed tomography (CT) is the reference examination (Alis, 2007).The diagnosis of textiloma is based on anatomopathological examination. Indeed, in the literature review by Le Neel et al. [4], the removal of textiloma resulted in cure without complication in 70 patients (59.8%), but complications worsened the evolution of 25 patients (21.3%) and 22 patients died (18.9%). Twenty-one of the 22 deaths were attributable to abdominal textilomas and concerned symptomatic textilomas recognized late, having required more aggressive procedures (intestinal and/ or colonic resection) with a non-negligible percentage of severe complications, in particular septic.
Hence the interest to act as quickly as possible since it considerably reduces the morbidity rate, as was considered in our case. CT scan is the reference imaging examination [5]. However, CT imaging of textiloma is not well known (Sarr, 2018). It may mimic a fecal impaction, abscess, hematoma, or tumor (Obeidat, 2020). Exceptionally in our patient, pure iatrogenic infarction of a liver segment is mistaken for a gossypiboma. Despite the use of imaging modalities, textilomas remain a diagnostic challenge and their discovery is often intraoperative [6]. The counting of pads and fields by the surgeon at the beginning and end of the procedure remains an effective but still insufficient means to overcome this oversight.
Conclusion
Gossypiboma with its diversified Clinico-radiological presentation entails - in spite of current advances - diagnostic difficulties and erraticities, causing significant tissue damage. CT and open surgery are the cornerstones for diagnosis and appropriate treatment. But by far, prevention remains the best option.
To read more about this article...Open access Journal of Anaesthesia & Surgery
Please follow the URL to access more information about this article
https://irispublishers.com/asoaj/fulltext/when-laparotomy-straightens-the-diagnosis.ID.000573.php
To know more about our Journals...Iris Publishers
To know about Open Access Publishers





No comments:
Post a Comment